What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about piroxicam. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Piroxicam Capsules. It contains the active ingredient, piroxicam.
It is used to treat symptoms such as swelling, stiffness and joint pain caused by:
- rheumatoid arthritis (when the tissue around a joint becomes thickened and inflamed leading to a build-up of fluid on the joint)
- osteoarthritis (when the cartilage between two bones becomes damaged)
- ankylosing spondylitis (a type of arthritis affecting the spine).
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
How it works
Piroxicam belongs to a group of medicines called non-steroidal anti-inflammatory drugs (NSAIDs). These medicines work by relieving pain and inflammation (heat, throbbing, swelling and redness).
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
There is no evidence that this medicine is addictive.
Use in children
Do not give this medicine to children under 12 years of age. The safety and effectiveness of this medicine in this age group have not been established.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You have any of the following problems affecting your digestive system:
- You have or have had a peptic ulcer (i.e. stomach or duodenal ulcer).
- You are vomiting blood, or material that looks like coffee grounds.
- You are bleeding from the rectum (back passage), have black, sticky bowel motions (stools).
- You have or have had inflammation of the lining of the stomach or bowel (e.g. Crohn's disease and ulcerative colitis). - You have or have had any of the following:
- heart (coronary artery) bypass surgery
- serious kidney or liver problems
- severe heart failure. - You are currently taking aspirin or any other NSAID medicine.
- You are hypersensitive to, or have had an allergic reaction to, piroxicam, aspirin, other NSAIDs or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include:
- Cough
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
- fainting
- hay fever-like symptoms.
Examples of serious allergic reactions affecting the skin include erythema multiforme (red patches on the arms, legs and face with blisters on the lips and lining of the mouth), Stevens-Johnson syndrome and toxic epidermal necrolysis (rash with blisters, and blisters covering large areas of the body; peeling or burning of the skin).
It is very important that you tell your doctor if you have had these or any type of skin reaction before.
You must not take piroxicam if you have had an allergic reaction to piroxicam, aspirin or other NSAID medicines.
If you think you are having an allergic reaction to piroxicam, stop taking this medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Do not take this medicine after the expiry date (EXP) printed on the pack or is the packaging is torn or shows signs of tampering. If it has expired or damaged, return it to your pharmacist for disposal.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies, hypersensitivity or intolerance to:
- any other medicines including aspirin or other NSAID medicines
- any other substances, such as foods, preservatives or dyes
- lactose - this medicine contains lactose.
- You have or have had any medical conditions, especially the following:
- heartburn, indigestion, stomach ulcer or other stomach problems
- asthma
- kidney or liver problems
- high blood pressure or heart problems
- swelling of the feet or ankles (oedema)
- a tendency to bleed
- an existing infection.
Piroxicam may hide some signs of infection (such as pain, fever, swelling or redness). This may lead you to mistakenly believe that you are better or that the infection is not serious.
- You are currently pregnant or plan to become pregnant. Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved.
Like most NSAID medicines, piroxicam is not recommended for use during pregnancy. It may affect your developing baby if you take it while you are pregnant, especially during the last three months of pregnancy.
- You are currently breastfeeding or you plan to breastfeed. Do not take this medicine whilst breastfeeding until you and your doctor have discussed the risks and benefits involved.
The active ingredient in this medicine passes into breast milk and may affect your baby.
- You are planning to have surgery.
- You are currently receiving or are planning to receive dental treatment.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, vitamins and supplements from the supermarket or health food shop.
Some medicines may interact with piroxicam. These include:
- aspirin, salicylates or any other anti-inflammatory agents used to relieve pain, swelling and other symptoms of inflammation
- diuretics (also called fluid or water tablets)
- medicines used to treat high blood pressure or heart problems. These include digoxin, ACE inhibitors, angiotensin receptor blockers and beta blockers
- warfarin, aspirin or other medicines used to stop blood clots
- medicines used to treat diabetes called sulphonylureas
- sulphonamide antibiotics
- methotrexate (used to treat arthritis, psoriasis and some cancers)
- medicines to treat depression such as lithium and SSRIs
- steroids (medicines used to treat allergies and hormone imbalances)
- cyclosporin or tacrolimus (given to help prevent rejection of transplanted organs)
- phenytoin (used to treat epilepsy or convulsions) and other medicines that effect, or is affected by, a liver enzyme called CYP 2C9.
If you are taking any of these medicines, you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with piroxicam.
Your doctor or pharmacist will have more information on medicines to be careful with or avoid while taking this medicine.
How to take this medicine
Follow carefully all directions given to you by your doctor or pharmacist. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor or pharmacist will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Normally you would start with 10 mg. After that the usual dose is 10 to 20 mg taken once each day.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
How to take it
Swallow the capsules whole, with a glass of water.
When to take it
Take this medicine with or immediately after food to reduce the chance of a stomach upset. Take this medicine at about the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
How long to take it for
Keep taking your medicine for as long as your doctor tells you. This is normally for a few weeks and then your doctor will review your treatment.
This medicine will not cure your condition but it should help to control pain, swelling and stiffness.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time. Otherwise, take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses. This may increase the chance of unwanted side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention. If you take too much piroxicam, you may feel sick, dizzy, drowsy or confused, or have stomach pain, vomiting or headache or faint or become unconscious and/or have problems breathing.
While you are taking this medicine
Things you must do
Be alert for any signs of allergy or hypersensitivity, or signs that this medicine may be seriously affecting your stomach or intestine or cardiovascular system. In particular, watch for skin rashes, passing or vomiting blood, feeling faint or having chest pain or tightness (see 'Possible side effects' for full details). Report anything new or unusual to your doctor immediately.
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you become pregnant or plan to breastfeed
- you are about to have any blood tests
- you are going to have surgery, including dental surgery.
Piroxicam can slow down blood clotting so it is important that your doctor, dentist or surgeon knows that you are taking it. - you get an infection.
Piroxicam may hide some of the signs of an infection and may make you think, mistakenly, that you are better or that it is not serious. Signs of an infection may include fever, pain, swelling and redness.
Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects by checking your potassium levels and seeing how your kidneys are working. Go to your doctor regularly for a check-up.
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking this medicine.
Things you must not do
Do not:
- give this medicine to anyone else, even if their symptoms seem similar to yours
- take your medicine to treat any other condition unless your doctor or pharmacist tells you to
- stop taking your medicine, or change the dosage, without first checking with your doctor.
Things to be careful of
Be careful while driving or operating machinery until you know how this medicine affects you.
As with other NSAID medicines, piroxicam may cause dizziness, drowsiness and blurred vision in some people.
If this occurs, do not drive, operate machinery or do anything else that could be dangerous.
Be careful of ingesting alcohol whilst taking piroxicam. As with other NSAID medicines ingesting alcohol may increase your risk of developing stomach problems.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking piroxicam or if you have any questions or concerns.
If you are over 70 years of age, you may have a higher chance of getting side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects. Sometimes they are serious but most of the time they are not.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- stomach upsets including nausea (feeling sick), vomiting, heartburn, indigestion and cramps
- constipation, diarrhoea, stomach pain and wind
- loss of appetite, weight loss or weight gain
- dizziness or light-headedness
- feeling thirsty
- chills, sweating or flushing
- sleepiness and drowsiness
- headache
- buzzing or ringing in the ears
- hair loss or thinning
- loose nails
- change in mood (eg. anxiety, nervousness or depression, or change in personality)
- sore mouth or tongue
- nose bleeds
- memory loss
- heavy periods
- numbness or tingling in hands or feet
- mild skin rash.
Tell your doctor as soon as possible if you notice any of the following.
These may be serious side effects. You may need medical attention:
- severe pain or tenderness in the stomach, often with nausea and vomiting
- eye problems such as blurred vision, sore red eyes or itching
- severe dizziness or a spinning sensation
- high or low blood sugar
- fast or irregular heart beat
- difficulty hearing or deafness
- unusual bruising or bleeding, reddish or purple blotches under the skin
- signs of frequent infections such as fever, chills, sore throat or mouth ulcers
- signs of anaemia such as tiredness, being short of breath and looking pale
- a change in the colour of the urine, blood in the urine
- a change in the amount of urine passed, burning feeling when passing urine
- unusual weight gain, swelling of the ankles or legs
- the symptoms of sunburn including redness, itching, swelling, blistering which may occur more quickly than normal
- high blood pressure
- hallucinations (seeing, feeling or hearing things that are not there)
- shaking or feeling uncoordinated.
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
These are very serious side effects and are usually very rare. You may need urgent medical attention or hospitalisation.
- yellowing of the eyes or the skin (jaundice)
- vomiting blood or material that looks like coffee grounds
- bleeding from your back passage (rectum), black sticky stools or bloody diarrhoea
- seizures or fits
- pain or tightness in the chest, possibly also with breathlessness
- meningitis (stiff neck, light sensitivity, drowsiness / confusion, unconsciousness and/or convulsions).
Other side effects not listed above may also occur in some people.
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it. If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C. Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
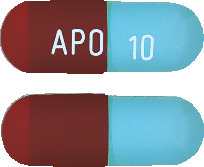
What APO-Piroxicam capsules look like
APO-Piroxicam 10 mg capsules
Deep powder blue opaque body, maroon opaque cap, hard gelatin capsule. Imprinted APO 10. Off-white powder fill.
Blister packs of 50 capsules.
APO-Piroxicam 20 mg capsules
Maroon cap/maroon body, marked "APO 20".
Blister packs of 25 capsules.
Ingredients
Each capsule contains 10 mg or 20 mg of piroxicam as the active ingredient.
It also contains the following inactive ingredients:
- lactose monohydrate
- microcrystalline cellulose
- maize starch
- stearic acid
- purified talc
- gelatin
- titanium dioxide
- allura red AC (CI 16035)
- iron oxide red (CI 77491)
- brilliant blue FCF (CI 42090)
- Opacode S-1-7085 white.
This medicine contains sulfites and sugars (as lactose).
This medicine is gluten-free, sucrose-free, tartrazine-free and free of other azo dyes.
Australian Registration Numbers
APO-Piroxicam 10mg capsules
Blister packs
AUST R 75039.
APO-Piroxicam 20mg capsules
Blister packs
AUST R 75043.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
This leaflet was last updated in: October 2021.
Published by MIMS December 2021


 Chemical name: 4-hydroxy-2-methyl-N-2-pyridinyl-2H-1, 2-benzothiazine-3-carboxamide 1, 1-dioxide. It is a member of a new chemical class of non-steroidal anti-inflammatory agents, N-heterocyclic carboxamides of 1, 2-benzothiazine-1, 1-dioxide.
Chemical name: 4-hydroxy-2-methyl-N-2-pyridinyl-2H-1, 2-benzothiazine-3-carboxamide 1, 1-dioxide. It is a member of a new chemical class of non-steroidal anti-inflammatory agents, N-heterocyclic carboxamides of 1, 2-benzothiazine-1, 1-dioxide.