What is in this leaflet
This leaflet answers some common questions about risedronate. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may want to read it again.
What this medicine is used for
Risedronate is used to treat osteoporosis, including osteoporosis caused by taking steroids. It is also used to preserve bone mineral density in patients on long term steroid therapy.
Osteoporosis
Throughout life, old bone is broken down and replaced with new bone. After the age of 35, bone loss may occur faster than your body can replace it. Excessive bone loss causes bones to become thinner and weaker, and therefore more likely to break.
Osteoporosis is a disease that gradually weakens bones. Early osteoporosis may not show symptoms. However, if left untreated, it can result in broken bones. Osteoporosis can also cause back pain, height loss and a curved back.
How it works
Risedronate works by slowing down the process of old bone being removed, which allows the bone-forming cells time to rebuild normal bone. This reverses the progression of osteoporosis by creating stronger bone which is less likely to fracture.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
This medicine is not addictive.
There is not enough information to recommend the use of risedronate in children under the age of 18 years.
Before you use this medicine
When you must not use it
Do not use this medicine if you have an allergy to:
- risedronate
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine if you are unable to stand or sit upright for at least 30 minutes.
Do not take this medicine if you have a condition called hypocalcaemia (a low level of calcium in the blood).
Do not take this medicine if you have severe kidney problems.
Do not take this medicine if you are pregnant. It is not recommended for use during pregnancy, unless you and your doctor have discussed the risks and benefits involved.
Do not take this medicine if you are breastfeeding. It is not known whether this medicine passes into breast milk.
Do not take this medicine after the expiry date printed on the pack.
If you take this medicine after the expiry date has passed, it may not work as well.
Do not take this medicine if the packaging is torn or shows signs of tampering. If it is expired or damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, any other substances, such as foods, preservatives or dyes.
Tell your doctor if you have any of the following medical conditions:
- disturbances of bone and mineral metabolism (for example vitamin D deficiency, parathyroid hormone abnormalities)
- problems with the tube that takes food from your mouth to your stomach (oesophagus) such as ulcers
- pain, swelling or numbness of the jaw or a "heavy jaw feeling" or loosening of a tooth
Check with your doctor or dentist to see if a dental check-up is required before starting Risedronate. This is especially important if you are receiving medicines or therapy used to treat cancer or taking corticosteroids (e.g. prednisone or cortisone).
Tell your doctor if you are pregnant, plan to become pregnant, are breastfeeding or plan to breastfeed.
Do not take this medicine until you and your doctor have discussed the risks and benefits involved.
If you have not told your doctor about any of the above, tell them before you use this medicine.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and risedronate may interfere with each other if taken at the same time. These include:
- antacids, used to treat indigestion eg Gaviscon, Mylanta
- other products containing calcium
- iron supplements
Check with your doctor or pharmacist if you are not sure whether you are taking any of these products. You may need to stop taking these products or take them at a different time of day to Risedronate.
These medicines may be affected by risedronate or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
You can take aspirin while you are being treated with Risedronate.
Your doctor may have more information on medicines to be careful with or avoid while taking Risedronate.
How to take this medicine
Follow all directions given to you by your doctor and pharmacist carefully. They may differ to the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to take
The usual dose is either:
- one 35 mg tablet weekly on the same day each week; or
- one 75 mg tablet taken on two consecutive days (two tablets in total) each month; or
- one 150 mg tablet monthly on the same date each month.
Choose the day that best fits your schedule.
How to take it
Swallow your tablet whole with a glass of plain water. Do not chew or suck the tablet.
Stay upright (sitting, standing or walking around) for at least 30 minutes after swallowing the tablet and until after you have eaten your first food of the day
Do not lie down immediately after swallowing it.
Do not take any food, medicines or drinks other than plain water for 30 minutes during this time.
These actions will help make sure the tablet reaches your stomach quickly and helps avoid irritation to your oesophagus.
It is important to take Risedronate with plain water only (120 ml), not mineral water. Mineral water and other drinks, including fruit juices, coffee and tea, will reduce the effect of Risedronate.
When to take it
This medicine should be taken on empty stomach. Food, drinks (other than plain water), and other medicines will lessen the effect of this medicine by interfering with its absorption into the body.
How long to take it
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
Risedronate 35 mg
If you have forgotten to take your 35 mg tablet, take your tablet on the day you remember. Do not take two tablets on the same day to make up for the missed dose. Return to taking one tablet once a week on your original chosen day.
Risedronate 75 mg
If you have forgotten to take one or both of your 75 mg tablets and it is more than 7 days until your next monthly doses are due, take the missed doses in the morning after the day you remembered (and the next morning if you missed both doses).
If the missed dose is within 7 days of your next month's doses, wait until the doses are next due and then continue taking your tablets as normal.
Risedronate 150 mg
If you have forgotten to take your 150 mg tablet and it is more than 7 days until your next monthly dose is due, take the missed dose in the morning after the day you remembered.
If the missed dose is within 7 days of your next month's dose, do not take your missed dose. Wait until the date you would normally take your tablet and continue taking your tablets as normal.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking this medicine
Things you must do
Tell any other doctors, dentists and pharmacists who are treating you that you are using this medicine.
If you are about to be started on any new medicine, tell your doctor or pharmacist that you are using this medicine.
If you become pregnant while you are using this medicine, tell your doctor immediately.
If you require a dental procedure, tell your dentist that you are taking risedronate. Invasive dental procedures should be avoided where possible. This type of medicine may cause jaw-bone problems in some people, such as infection or delayed healing after teeth are pulled out or other work that involves drilling into the jaw.
Tell your doctor or dentist immediately if you develop a toothache, jaw pain, painful exposed bone or swelling, especially following dental work.
Speak to your doctor and dentist about good oral hygiene and regular dental check-ups while you are using risedronate.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are taking Risedronate.
Tell your doctor immediately if you develop new or unusual thigh, hip or groin pain.
If you are going to have surgery, tell the surgeon and anaesthetist that you are using this medicine.
If you are about to have any blood tests, tell your doctor that you are taking this medicine.
Keep all of your doctor's appointments so that your progress can be checked. Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects.
Things you must not do
Do not lie down for 30 minutes after taking Risedronate.
Do not have any food or drink except for plain water for 30 minutes after taking Risedronate.
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not take your medicine to treat any other complaint unless your doctor tells you to.
Do not stop taking your medicine or change the dosage without first checking with your doctor or pharmacist.
Things to be careful of
Be careful while driving or operating machinery until you know how risedronate affects you.
Side effects
Tell your doctor and pharmacist as soon as possible if you do not feel well while you are taking risedronate.
This medicine helps most people with osteoporosis but may have unwanted side effects in some people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- stomach pain
- diarrhoea
- aching muscles, joints or bones
- headache
- nausea
- runny nose
- sore throat
- dizziness
The above list includes the more common side effects of this medicine. They are usually mild.
Tell your doctor as soon as possible if you notice any of the following:
- skin rash or redness of the skin, sometimes made worse by sunlight, itchiness
- blurred vision, pain or redness in the eyes
- jaw or teeth problems associated with delayed healing and/or infection, often following a tooth extraction or invasive dental work
These side-effects are rare.
If any of the following happen, stop taking Risedronate and tell your doctor immediately:
- difficulty or pain on swallowing
- chest pain
- new or worsening heartburn
These side effects may be due to irritation or ulceration of the food pipe. They may worsen if you continue taking the tablets. These side effects are rare.
If you notice any of the following, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- swelling of the face, lips, mouth, throat or tongue
- severe skin reactions.
The above list includes very serious side effects. You may need urgent medical attention.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some patients.
Storage and disposal
Storage
Keep your medicine in the pack until it is time to take it. If you take your medicine out of the pack it may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 25°C.
Do not store your medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine left over.
Product description
What it looks like
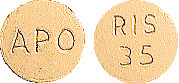
35 mg tablets:
Orange, round, biconvex coated tablets, engraved "APO" on one side, "RIS" over "35" on the other side.
Blister packs of 1, 4, 8, 12 and 16 tablets. AUST R 160642
Bottles of 4, 8, 12 and 30 tablets. AUST R 160644
75 mg tablets:
Dark pink, round, biconvex coated tablets, engraved "APO" on one side, "RIS" over "75" on the other side.
Blister packs of 2, 4, 6 and 8 tablets. AUST R 181973
Bottles of 30 tablets AUST R 181977
150 mg tablets:
Blue, round, biconvex coated tablets, engraved "APO" on one side, "RIS" over "150" on the other side. Blister packs of 1, 2, 3 and 4 tablets. AUST R 181970
*Not all strengths, pack types and/or pack sizes may be available
Ingredients
Each tablet contains 35 mg, 75 mg or 150 mg of risedronate sodium as the active ingredient.
It also contains the following:
- lactose
- crospovidone
- magnesium stearate
- colloidal anhydrous silica
- hypromellose
- hyprolose
- macrogol 8000
- titanium dioxide
- iron oxide red (35 mg and 75 mg tablets only)
- iron oxide yellow (35 mg tablets only)
- indigo carmine aluminium lake (150 mg tablets only)
- monobasic sodium phosphate dihydrate (150 mg tablets only)
- dibasic sodium phosphate (150 mg tablets only)
Contains sugars as lactose (150mg tablets).
This medicine does not contain gluten, sucrose, tartrazine or any other azo dyes.
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15 – 17 Chapel Street
Cremorne, VIC, 3121
Australia
Web: https://arrotex.com.au
This leaflet was prepared in January 2023.
Published by MIMS March 2023



 In a 2 year study in men with osteoporosis, the overall safety and tolerability were similar between the treatment and the placebo groups. Adverse experiences were consistent with those previously observed in women.
In a 2 year study in men with osteoporosis, the overall safety and tolerability were similar between the treatment and the placebo groups. Adverse experiences were consistent with those previously observed in women.

 Three patients that received risedronate 30 mg/day experienced acute iritis in one supportive study. All three patients recovered from their events; however, in one of these patients, the event recurred during risedronate treatment and again during treatment with pamidronate. All patients were effectively treated with topical steroids.
Three patients that received risedronate 30 mg/day experienced acute iritis in one supportive study. All three patients recovered from their events; however, in one of these patients, the event recurred during risedronate treatment and again during treatment with pamidronate. All patients were effectively treated with topical steroids.
 The incidence of non-vertebral fractures in the pooled analysis (RVN and RVE) was lower in the risedronate sodium 5 mg daily group than in the placebo group for all fractures at these sites combined, as well as for the wrist, humerus, pelvis and leg separately. This difference was significant for all non-vertebral osteoporosis related fractures (p = 0.005), as well as for the humerus (p = 0.024) and pelvis (p = 0.044), while a trend was seen at the wrist (p = 0.075) (Table 6). These findings demonstrate a beneficial effect of risedronate in preventing non-vertebral, osteoporosis-related fractures.
The incidence of non-vertebral fractures in the pooled analysis (RVN and RVE) was lower in the risedronate sodium 5 mg daily group than in the placebo group for all fractures at these sites combined, as well as for the wrist, humerus, pelvis and leg separately. This difference was significant for all non-vertebral osteoporosis related fractures (p = 0.005), as well as for the humerus (p = 0.024) and pelvis (p = 0.044), while a trend was seen at the wrist (p = 0.075) (Table 6). These findings demonstrate a beneficial effect of risedronate in preventing non-vertebral, osteoporosis-related fractures.

 Very few patients in any treatment group had new fractured vertebrae at month 12 (5 mg daily: 1.5%; 35 mg once a week: 1.3%). No patient had more than one new fractured vertebra. There were no statistically significant differences in the percentage of patients with new vertebral fractures among the two treatment groups.
Very few patients in any treatment group had new fractured vertebrae at month 12 (5 mg daily: 1.5%; 35 mg once a week: 1.3%). No patient had more than one new fractured vertebra. There were no statistically significant differences in the percentage of patients with new vertebral fractures among the two treatment groups. The effect of risedronate discontinuation on bone mineral density was studied in a double-blind, placebo-controlled study in post-menopausal women with glucocorticoid dependent rheumatoid arthritis. Women were treated for two years with risedronate 2.5 mg daily, cyclic risedronate (averaged 2.5 mg risedronate per day over the 96 week active period) or placebo and then followed without treatment for one more year. Patients continued glucocorticoid treatment during the third year of the study. Risedronate discontinuation resulted in bone loss at all skeletal sites (proximal femur and lumbar spine) during the third year. The rate of bone loss, however, was similar to the placebo group indicating that bone loss was not accelerated after risedronate was discontinued. The study supports the use of continuous treatment with risedronate to prevent bone loss.
The effect of risedronate discontinuation on bone mineral density was studied in a double-blind, placebo-controlled study in post-menopausal women with glucocorticoid dependent rheumatoid arthritis. Women were treated for two years with risedronate 2.5 mg daily, cyclic risedronate (averaged 2.5 mg risedronate per day over the 96 week active period) or placebo and then followed without treatment for one more year. Patients continued glucocorticoid treatment during the third year of the study. Risedronate discontinuation resulted in bone loss at all skeletal sites (proximal femur and lumbar spine) during the third year. The rate of bone loss, however, was similar to the placebo group indicating that bone loss was not accelerated after risedronate was discontinued. The study supports the use of continuous treatment with risedronate to prevent bone loss.
 Chemical name: [1-hydroxy-2-(3-pyridinyl)ethylidene]bis[phosphonic acid], monosodium salt, hemipentahydrate.
Chemical name: [1-hydroxy-2-(3-pyridinyl)ethylidene]bis[phosphonic acid], monosodium salt, hemipentahydrate.