What is in this leaflet
This leaflet answers some common questions about simvastatin. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may want to read it again.
What this medicine is used for
Simvastatin is used:
- to help lower cholesterol and triglyceride levels
- in people who have coronary heart disease (CHD)
- in people with a high risk of CHD (e.g. diabetes, a history of stroke, or other blood vessel disease)
Simvastatin can reduce the risk of a heart attack or stroke, reduce the need for surgery to increase blood flow to the heart, and can reduce the need for hospitalisation due to angina.
Cholesterol:
Everyone has cholesterol and triglycerides in their blood. The body uses them for many things, such as building cell walls and hormones.
Your body makes cholesterol, but it also comes from food. The body balances the cholesterol it makes with the cholesterol it gets from food. This means if more cholesterol comes from food, less is made by the body. However, if you eat a high-fat diet, your body may not keep this balance and your cholesterol levels rise.
Too much cholesterol or triglycerides can be a problem. When you have high levels of cholesterol, it may 'stick' to the inside of your blood vessels instead of being carried to the parts of the body where it is needed. Over time this can form hard areas (called plaque) on the walls of blood vessels, making it more difficult for the blood to flow. This blocking of your blood vessels can lead to coronary heart disease (such as heart attacks and angina) and stroke. High cholesterol is more likely to occur with certain diseases or if you have a family history of high cholesterol.
There is usually no symptoms of high cholesterol or triglycerides. Your doctor can measure your cholesterol and triglycerides with a blood test.
There are two types of cholesterol, called LDL and HDL cholesterol. LDL cholesterol is the 'bad' cholesterol that can block vessels. HDL cholesterol is the 'good' cholesterol that is thought to remove bad cholesterol from blood vessels.
Triglycerides are an energy source for the body.
How it works
Simvastatin belongs to a group of medicines known as HMG-CoA reductase inhibitors.
Simvastatin works by reducing bad (LDL) cholesterol made by the liver and raises the good (HDL) cholesterol. It may slow the hardening of blood vessels and reduce the risk of developing new plaque.
Simvastatin does not reduce the cholesterol and triglycerides that come from fat in food. Therefore, you also need to follow a low-fat diet and other measures, such as exercise and weight control, while you are taking simvastatin.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
This medicine is not addictive.
Safety and effectiveness have been studied in 10-17 year old boys and in girls, who had started their menstrual period at least one year before (see How to take this medicine). This medicine has not been studied in children under the age of 10 years. For more information, talk to your doctor.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- simvastatin
- lactose
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- painful joints
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine if you have or have had any of the following medical conditions:
- liver disease or unexplained high levels of liver enzymes
- muscle pain, tenderness or weakness (myopathy) from other medicines used to treat high cholesterol or triglycerides
Do not take this medicine if you are taking the following medicines:
- gemfibrozil
- cyclosporin
- danazol
- CYP3A4 inhibitors (e.g. itraconazole, ketoconazole, posaconazole, voriconazole)
- HIV protease inhibitors (e.g. indinavir, nelfinavir, ritonavir, saquinavir)
- hepatitis C virus protease inhibitors (e.g. boceprevir, telaprevir)
- some antibiotics (e.g. fusidic acid, erythromycin, clarithromycin, telithromycin)
- nefazodone
Do not take this medicine if you are pregnant or there is a chance that you could become pregnant (e.g. not using adequate contraception). Simvastatin may affect your developing baby if you take it during pregnancy.
Do not take this medicine if you are breastfeeding. Your baby may absorb this medicine from breast milk, and therefore there is a possibility of harm to the baby.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- liver disease
- kidney disease
- thyroid problems
- unexplained muscle pain, tenderness or weakness not caused by exercise
Tell your doctor if you drink alcohol regularly.
Tell you doctor is become pregnant or plan to breast feed.
Tell you doctor if you are Asian.
Tell your doctor if you are taking niacin (also known as nicotinic acid) or a niacin-containing product, particularly if you are Chinese.
If you have not told your doctor about any of the above, tell them before you start taking this medicine.
you have or have had myasthenia gravis (a disease causing general muscle weakness including in some cases muscles used for breathing) or ocular myasthenia (a disease causing eye muscle weakness) as statins may lead to occurrence of myasthenia or aggravate the condition.
Taking other medicines
Tell your doctor and pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines must not be taken with simvastatin as they may increase the risk of muscle side effect with this medicine. It is particularly important to tell your doctor if you are taking:
- nefazodone, used to treat depression
- gemfibrozil, used to treat high cholesterol levels
- cyclosporin, used to suppress the immune system
- danazol
- medicines known as 'CYP3A4 inhibitors', used to treat certain fungal infections (e.g. itraconazole, ketoconazole, posaconazole, voriconazole)
- medicines containing cobicistat, used for HIV infection
- HIV protease inhibitors (e.g. indinavir, nelfinavir, ritonavir, saquinavir)
- certain hepatitis C virus protease inhibitors (e.g. boceprevir, telaprevir)
- antibiotics used to treat infections (e.g. erythromycin, fusidic acid, clarithromycin, telithromycin)
If you are taking any of the above, your doctor may suggest stopping this medicine temporarily or permanently.
Some other medicines may interact with simvastatin. Because taking this medicine with any of the following drugs can increase the risk of muscle problems (see Side Effects), it is particularly important to tell your doctor if you are taking:
- other medicines used to lower cholesterol levels, such as other fibrates, niacin (also known as nicotinic acid)
- warfarin and other medicines used to prevent blood clots
- colchicine, used for gout
- medicines used to treat high blood pressure, angina or other heart conditions (e.g. verapamil, diltiazem, amlodipine)
- lomitapide, used for a serious and rare genetic cholesterol condition
- amiodarone, used to treat irregular heart beat
- digoxin, used to treat heart failure
- certain hepatitis C antiviral agents (e.g. elbasvir or grazoprevir)
- daptomycin, a drug used to treat complicated skin and skin structure infections and bacteraemia.
These medicines may be affected by this medicine, may affect how well it works, or may increase the risk of side effects with this medicine. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
You should also tell any doctor who is prescribing a new medication for you that you are taking this medicine.
Grapefruit juice, especially in large amounts, may also interfere with the way simvastatin works in your body. However, one glass of grapefruit juice per day is unlikely to have any effect.
How to take this medicine
Follow all directions given to you by your doctor or pharmacist carefully. They may differ to the information contained in this leaflet.
If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
How much to take
Take this medicine only when prescribed by your doctor.
Your doctor will tell you how much of this medicine you should take, depending on your condition and whether you are taking other medicines.
For adults, the recommended starting dose is 10 mg or 20 mg per day, taken in the evening, which may need to be increased up to 80 mg daily to have the best effect.
Because of the increased risk of muscle problems, the 80 mg dose should only be used in patients at a high risk of heart problems who have not reached their cholesterol goal on lower doses.
For children (10-17 years old), the maximum recommended dose is 40 mg a day.
For people with CHD or risk of CHD:
The usual starting dose is 40 mg per day, taken in the evening.
How to take it
Swallow the tablets whole with a glass of water.
When to take it
Take this medicine at the same time each day, preferably in the evening. The liver produces its greatest amount of cholesterol when the body is at rest and when there is no dietary intake. For most people, this is at night when asleep. Therefore, this medicine is more effective when taken in the evening, such as after your evening meal, however it can be taken without food.
Taking it at the same time each day will have the best effect and will also help you remember when to take it.
How long to take it for
Continue taking this medicine for as long as your doctor tells you.
Simvastatin helps to lower your cholesterol, but it does not cure your condition. It is important to keep taking your medicine even if you feel well. You may have to take cholesterol-lowering medicines for the rest of your life. If you stop taking this medicine, your cholesterol levels may rise again.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
If it is almost time to take your next dose, skip the dose you missed and take your next dose at the usual time.
Otherwise take it as soon as you remember and then go back to taking your medicine as you would normally.
If you are not sure whether to skip the dose, talk to your doctor or pharmacist.
Do not take a double dose to make up for missed doses. This may increase the chance of you experiencing side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking this medicine.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
If you become pregnant while taking this medicine, stop taking it and tell your doctor immediately.
Keep all of your doctor's appointments so that your progress can be checked. Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects.
Your doctor may suggest stopping the tablets a few days before surgery.
Things you must not do
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not take your medicine to treat any other complaint unless your doctor tells you to.
Do not stop taking your medicine or change the dosage without first checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how this medicine affects you. Simvastatin generally does not affect your ability to drive a car or operate machinery. However, this medicine may cause dizziness in some people. Make sure you know how you react to this medicine before you drive a car or operate machinery.
Avoid drinking large quantities of alcohol. Drinking large amounts of alcohol may increase the risk of liver problems.
Avoid drinking grapefruit juice. Grapefruit juice can alter the metabolism of simvastatin.
Changes to lifestyle that may help reduce the chance of coronary heart disease
Lowering high cholesterol can help reduce your chances of having coronary heart disease (CHD). However, your chances of having CHD may be increased by several other factors including high blood pressure, cigarette smoking, diabetes, excess weight, family history of CHD, being a male and being a woman who has reached menopause.
Some self help measures suggested below may help your condition and help reduce your chances of having CHD. Talk to your doctor, pharmacist, or dietician about these measures and for more information.
- Diet
- continue the low fat diet recommended by your doctor, dietician or pharmacist. - Weight
- your doctor may advise you to lose weight if you are overweight. - Exercise
- make exercise a part of your routine – walking is good. Ask your doctor for advise before starting exercise. - Smoking
- your doctor may advise you to stop smoking or at least cut down.
Side effects
Tell your doctor and pharmacist as soon as possible if you do not feel well while you are taking simvastatin.
This medicine helps most people, but may cause unwanted side effects in some people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following:
- stomach upset, such as nausea, vomiting, constipation, diarrhoea, flatulence, pain, reflux
- headache
- dizziness
The above list includes the more common side effects of your medicine. For the most part, these have been mild and short-lived.
Tell your doctor as soon as possible if you notice any of the following:
- tingling or numbness in the hands or feet
- tiredness, shortness of breath, looking pale (signs of anaemia)
- fever, flushing and/or generally feeling unwell
- skin rash, itchiness
- pinkish, itchy swellings on the skin, also called hives or nettle rash
- painful, swollen joints
- bruising more easily than normal
- larger breasts than normal in men
The above list includes serious side effects that may require medical attention.
Liver problems can also occur and may be serious. Your doctor will do blood test to check your liver.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, or other parts of the body; rash, itching or hives on the skin (signs of an allergic reaction)
- dry cough, trouble breathing, high temperature, weight loss, feeling tired (signs of interstitial lung disease)
- feeling unusually tired or weak; loss of appetite; yellowing of the skin and/or eyes, also called jaundice; dark urine (signs of a liver problem)
- sharp pain in the upper stomach (pancreatitis)
- brown or dark coloured urine, severe muscle aching all through the body, muscle weakness (muscle breakdown)
Rarely, muscle breakdown can be serious and result in kidney damage or lead to death. The risk of muscle problems is greater for:
- patients taking higher doses of simvastatin, such as 80 mg
- older patients (65 years of age and older)
- female patients
- patients with abnormal kidney function
- patients with thyroid problems.
Tell your doctor if you notice:
- hair loss
- muscle cramps
- trouble sleeping
- poor memory, memory loss, confusion
- feelings of depression
- blurred vision and impaired vision
- erectile dysfunction
- breathing problems including persistent cough and/or shortness of breath or fever
- gynaecomastia (breast enlargement in men) (very rare)
- muscle rupture (very rare)
- rash that occur on the skin or sores in the mouth (lichenoid drug eruptions) (very rare)
These are other side effects that have been reported with simvastatin.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some patients.
Storage and disposal
Storage
Keep your medicine in its pack until it is time to take it. If you take your medicine out of its pack it may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C. Protect from light and moisture.
Do not store your medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine leftover.
Product description
What it looks like
10 mg Tablets
Light pink coloured, oval, biconvex film-coated tablets, marked 'SVN 10' on one side and 'NEO' on the other side.
Blister packs of 30 tablets: AUST R 223448.
Bottles of 30 tablets: AUST R 223452.
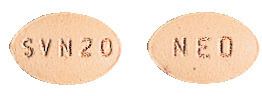
20 mg Tablets
Tan coloured, oval, biconvex film-coated tablets, marked with 'SVN 20' on one side and 'NEO' on the other side.
Blister packs of 30 tablets: AUST R 223449.
Bottles of 30 tablets:): AUST R 223453.
40 mg Tablets
Pink coloured, oval, biconvex film-coated tablets, marked 'SVN 40' on one side and 'NEO' on the other side. Blister packs of 30 tablets: AUST R 223450.
Bottles of 30 tablets: AUST R 223454.
80 mg Tablets
Pink coloured, capsule-shaped, biconvex film-coated tablets marked with 'SVN 80' on one side and 'NEO' on the other side.
Blister packs of 30 tablets: AUST R 223451.
Bottles of 30 tablets: AUST R 223455.
*Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains either 10, 20, 40 or 80 mg of simvastatin as the active ingredient.
It also contains the following:
- butylated hydroxyanisole
- ascorbic acid
- citric acid monohydrate
- microcrystalline cellulose
- magnesium stearate
- lactose monohydrate
- pregelatinised maize starch
- Opadry 20A54692 Pink (10 mg only)
- Opadry 20A56767 Brown (20 mg only)
- Opadry 20A54535 Pink (40 mg and 80 mg only)
Contains sugars as lactose.
This medicine does not contain gluten, sucrose, tartrazine or any other azo dyes.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
APO and APOTEX are registered trademarks of Apotex Inc.
This leaflet was prepared in August 2023.
Published by MIMS September 2023





 Myopathy has been reported rarely.
Myopathy has been reported rarely. In a separate study involving 180 patients with combined hyperlipidaemia, simvastatin 10 mg/day for 17 weeks was also shown to be effective in lowering total-C, LDL-C, VLDL-C, TGs and Apo B (see Table 4).
In a separate study involving 180 patients with combined hyperlipidaemia, simvastatin 10 mg/day for 17 weeks was also shown to be effective in lowering total-C, LDL-C, VLDL-C, TGs and Apo B (see Table 4). The data from these studies demonstrate that in patients with hypercholesterolaemia and normal or slightly raised TG, simvastatin consistently reduces total-C, LDL-C, TG, VLDL-C and Apo B in a dose dependent manner.
The data from these studies demonstrate that in patients with hypercholesterolaemia and normal or slightly raised TG, simvastatin consistently reduces total-C, LDL-C, TG, VLDL-C and Apo B in a dose dependent manner. In the upper dose comparative study, one-third of patients obtained a reduction in LDL-C of 53% or more at the 80 mg dose. The percent reduction in LDL-C was essentially independent of the baseline level. In contrast, the percent reduction in TG was related to the baseline level of TG. Of the 664 patients randomised to 80 mg, 475 patients with plasma TG ≤ 2.25 mmol/L had a median reduction in TG of 21%, while in 189 patients with hypertriglyceridaemia (> 2.25 mmol/L), the median reduction in TG was 36%. In these studies, patients with TG > 4.0 mmol/L were excluded.
In the upper dose comparative study, one-third of patients obtained a reduction in LDL-C of 53% or more at the 80 mg dose. The percent reduction in LDL-C was essentially independent of the baseline level. In contrast, the percent reduction in TG was related to the baseline level of TG. Of the 664 patients randomised to 80 mg, 475 patients with plasma TG ≤ 2.25 mmol/L had a median reduction in TG of 21%, while in 189 patients with hypertriglyceridaemia (> 2.25 mmol/L), the median reduction in TG was 36%. In these studies, patients with TG > 4.0 mmol/L were excluded. The effects of simvastatin on major vascular events and major coronary events were similar in all subgroups of patients (see Figure 1).
The effects of simvastatin on major vascular events and major coronary events were similar in all subgroups of patients (see Figure 1). N = number of patients in each subgroup. All subgroups were defined at baseline. In this study, patients were classified with metabolic syndrome if they had abdominal obesity, elevated blood pressure, and low HDL-C; other factors such as fasting TG and insulin resistance were not measured. Placebo incidence is the percentage of patients in the placebo group who had one or more MVE or MCE during the study. The inverted triangles are point estimates of the risk ratio in the simvastatin group, with their 95% confidence intervals represented as a line. If the point estimate fell on the left of the unity line, the observed outcome was better in patients allocated active simvastatin. Conversely, if it fell on the right, the observed outcome was better in patients taking the placebo. The areas of the triangles are proportional to the number of patients with the relative endpoint. The vertical dashed line represents the point estimate of relative risk in the entire study population. RRR (%) represents relative risk reduction, i.e. (1 risk ratio) x 100%.
N = number of patients in each subgroup. All subgroups were defined at baseline. In this study, patients were classified with metabolic syndrome if they had abdominal obesity, elevated blood pressure, and low HDL-C; other factors such as fasting TG and insulin resistance were not measured. Placebo incidence is the percentage of patients in the placebo group who had one or more MVE or MCE during the study. The inverted triangles are point estimates of the risk ratio in the simvastatin group, with their 95% confidence intervals represented as a line. If the point estimate fell on the left of the unity line, the observed outcome was better in patients allocated active simvastatin. Conversely, if it fell on the right, the observed outcome was better in patients taking the placebo. The areas of the triangles are proportional to the number of patients with the relative endpoint. The vertical dashed line represents the point estimate of relative risk in the entire study population. RRR (%) represents relative risk reduction, i.e. (1 risk ratio) x 100%.

 A single dose of 2 g niacin extended release coadministered with 20 mg simvastatin increased the AUC and Cmax of simvastatin acid by approximately 60% and 84%, respectively, compared to administration of 20 mg simvastatin alone. In this study, the effect of simvastatin on niacin pharmacokinetics was not measured.
A single dose of 2 g niacin extended release coadministered with 20 mg simvastatin increased the AUC and Cmax of simvastatin acid by approximately 60% and 84%, respectively, compared to administration of 20 mg simvastatin alone. In this study, the effect of simvastatin on niacin pharmacokinetics was not measured. Chemical name: [1S-[1α,3α,7β,8β (2S*,4S*),8aβ]]-1,2,3,7,8,8a-hexahydro-3,7-dimethyl-8-[2-(tetrahydro-4-hydroxy-6-oxo-2H-pyran-2-yl)ethyl]-1-naphthalenyl 2,2-dimethylbutanoate.
Chemical name: [1S-[1α,3α,7β,8β (2S*,4S*),8aβ]]-1,2,3,7,8,8a-hexahydro-3,7-dimethyl-8-[2-(tetrahydro-4-hydroxy-6-oxo-2H-pyran-2-yl)ethyl]-1-naphthalenyl 2,2-dimethylbutanoate.