What is in this leaflet
This leaflet answers some common questions about valaciclovir. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
Valaciclovir is used to treat:
- shingles (herpes zoster)
- shingles affecting the eye region (ophthalmic zoster)
- cold sores (herpes labialis)
It belongs to a group of medicines called antivirals.
How it works
Valaciclovir works by stopping the multiplication of the virus which causes shingles and cold sores. It can reduce the length and severity of an outbreak, as well as reduce the duration of pain associated with shingles and cold sores.
It is important that treatment for shingles is started within the first three days of the shingles attack.
For the treatment of cold sores, the tablets should be taken at the earliest symptom of a cold sore (e.g. tingling, itching, or burning).
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
Valaciclovir is more effective in patients 50 years of age and older.
This medicine is available only with a doctor's prescription.
This medicine is not addictive.
There is not enough information to recommend the use of this medicine in children.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- valaciclovir
- aciclovir
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- kidney or liver disease
- anaemia (reduced red blood cells or iron stores)
Care should be taken to ensure adequate fluid intake in patients who are risk of dehydration, such as the elderly.
Tell your doctor if you are currently pregnant or you plan to become pregnant, or are breastfeeding. Your doctor will discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell them before you start taking valaciclovir.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and valaciclovir interfere with each other. These include:
- mycophenolate mofetil, cyclosporin and tacrolimus, medicines taken for organ transplantation
- aminoglycoside antibiotics, such as gentamicin
- pentamidine, used to treat or prevent certain infections
- foscarnet, used against viruses
- methotrexate, used for conditions such as rheumatoid arthritis
- organoplatinum compounds, used in cancer
- iodine based contrast media for scans
These medicines may be affected by this medicine or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
Other medicines not listed above may also interact with valaciclovir.
How to take this medicine
Follow all direction given to you by your doctor or pharmacist carefully. They may differ to the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to take
Shingles (herpes zoster), including shingles affecting the eye region (ophthalmic zosters):
The usual dose is two 500 mg tablets taken three times a day, or one 1000 mg tablet taken three times a day.
Cold sores (herpes labialis):
The usual dose for the one-day regimen is four 500 mg tablets taken twice a day, or two 1000 mg tablets taken twice a day. The second dose is taken about 12 hours after the first dose.
How to take it
Swallow the tablets whole with a full glass of water. You should drink plenty of fluids whilst taking valaciclovir, especially if you are elderly.
When to take it
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Shingles (herpes zoster), including shingles affecting the eye region (ophthalmic zosters):
The usual course of treatment is seven days.
Do not stop taking it unless your doctor tells you to, even if you feel better.
Make sure you have enough to last over weekends and holidays.
Cold sores (herpes labialis):
The course of treatment should not exceed one day (2 doses) and the doses should be taken 12 hours apart.
If you forget to take it
Shingles (herpes zoster), including ophthalmic zosters (shingles affecting the eye region):
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, then go back to taking your medicine as you would normally.
Cold sores (herpes labialis):
Take the second dose as soon as possible once 12 hours have passed.
If you miss more than one dose, or you are not sure what to do, ask your doctor or pharmacist.
Do not take a double dose to make up for missed doses. This may increase the chance of side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Signs of an overdose with valaciclovir may include:
- acute renal failure, which may present as: decreased urine; fluid retention causing swollen legs, ankles or feet; nausea; drowsiness; fatigue; difficulties breathing.
- confusion, hallucinations, agitation, decreased consciousness and coma.
- nausea and vomiting
While you are taking this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking valaciclovir.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking valaciclovir.
If you become pregnant while you are taking valaciclovir, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine.
Keep all of your doctor's appointments so that your progress can be checked. Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects.
Things you must not do
Do not take your medicine to treat any other complaints unless your doctor tells you to.
Do not give this medicine to anyone else, even if they have the same condition as yours.
Do not stop taking your medicine, or change the dosage, without first checking with your doctor.
Things to be careful of
Be careful when driving or operating machinery until you know how valaciclovir affects you. This medicine may cause dizziness and drowsiness in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking valaciclovir.
This medicine helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
If you are over 65 years of age you may have an increased chance of getting side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following:
- headache
- gastrointestinal discomfort (vomiting, nausea, diarrhoea, constipation, flatulence, abdominal pain, indigestion)
- dry mouth
- nervousness
- drowsiness
- increase in blood pressure
- swelling
- difficulty sleeping
- muscle aches, pain or weakness
The above list includes the more common side effects of your medicine.
Tell your doctor as soon as possible if you notice any of the following:
- decreased consciousness, dizziness, weakness
- fever, chills, infections or flu like symptoms
- back or joint pain
- skin rash, which may be itchy
- sensitivity to UV light, such as development of a rash like sunburn even after short exposure to UV light
The above list includes serious side effects that may need medical attention.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- allergic reaction, which may present as: shortness of breath; wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body;
- damage to the kidney, which may present as: decreased urine; fluid retention causing swollen legs, ankles or feet; nausea; drowsiness; fatigue; difficulties breathing
- damage to the liver, which may present as: nausea and vomiting; loss of appetite; feeling generally unwell; fever; itching; yellowing of the skin and eyes; dark coloured urine
- unusual bruising or bleeding, which may indicate that the number of platelets (a type of blood cell responsible for blood clotting) in your blood are reduced
- coma
- agitation, tremor
- uncoordinated eye and muscle movements, difficulty speaking
- confusion, difficulty thinking, imagining sights or sounds (hallucinations), psychotic episodes
- convulsions or seizures.
These are very serious side effects and you may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some patients.
Storage and disposal
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What APO-Valaciclovir looks like
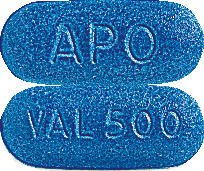
500 mg tablets
Dark blue, capsule-shaped, biconvex film-coated tablets, engraved "APO" on one side, "VAL 500" on the other side.
Blisters of 2, 4, 6, 8, 10, 20, 30, 42, 60, 80, 90, 100 tablets and bottles of 100 tablets.
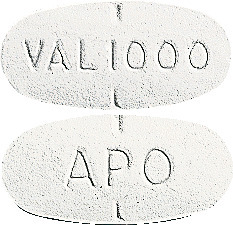
1000 mg tablets
White, oval shaped, biconvex film-coated tablet, partially scored and engraved "APO" on one side, "VAL 1000" on the other side.
Blisters of 3, 4, 21 tablets and bottles of 100 tablets.
Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains valaciclovir as the active ingredient.
It also contains the following:
- Stearic Acid
- Colloidal Anhydrous Silica
- Hypromellose
- Macrogol 8000
- Titanium Dioxide
- Indigo Carmine Aluminium Lake
This medicine is free from gluten, lactose, sucrose, tartrazine and other azo dyes.
Australian Registration Numbers
APO-Valaciclovir 500 mg tablets (blister pack): AUST R 158911
APO-Valaciclovir 500 mg tablets (bottle): AUST R 158910
APO-Valaciclovir 1000 mg tablets (bottle): AUST R 158907
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park, NSW 2113
APO and APOTEX are registered trade marks of Apotex Inc.
This leaflet prepared in July 2018.
Published by MIMS October 2018


 There was no significant difference to the duration of zoster associated pain when treatment was started within 48 hours or 72 hours. Patients treated within 48 hours of rash onset were found to have faster healing rates as measured by the duration of new lesion formation and time to crusting or healing of 50% or more of lesions. Thus, greater benefit is gained if the drug is started within 48 hours (see Figure 1).
There was no significant difference to the duration of zoster associated pain when treatment was started within 48 hours or 72 hours. Patients treated within 48 hours of rash onset were found to have faster healing rates as measured by the duration of new lesion formation and time to crusting or healing of 50% or more of lesions. Thus, greater benefit is gained if the drug is started within 48 hours (see Figure 1). In a second, placebo controlled trial in patients under 50 years of age (n = 399), demonstration of efficacy was restricted to a small decrease in mean time to cessation of new lesion formation. No significant effects were demonstrated for other outcomes of herpes zoster in this age group. Nevertheless, the occasional younger patients with severe herpes zoster may benefit from therapy with valaciclovir. Herpes zoster is usually a milder condition in younger patients.
In a second, placebo controlled trial in patients under 50 years of age (n = 399), demonstration of efficacy was restricted to a small decrease in mean time to cessation of new lesion formation. No significant effects were demonstrated for other outcomes of herpes zoster in this age group. Nevertheless, the occasional younger patients with severe herpes zoster may benefit from therapy with valaciclovir. Herpes zoster is usually a milder condition in younger patients. Results show that 250 mg twice daily offered the best clinical efficacy for suppression of genital herpes recurrences in this group of patients. However, the same total daily dose given as single daily dose (i.e. 500 mg once daily) was also very effective, as confirmed with Study BQRT/95/0026.
Results show that 250 mg twice daily offered the best clinical efficacy for suppression of genital herpes recurrences in this group of patients. However, the same total daily dose given as single daily dose (i.e. 500 mg once daily) was also very effective, as confirmed with Study BQRT/95/0026. Valaciclovir was also significantly better than placebo in preventing or delaying the development of viraemia, viruria and clinical HSV disease during the study period. No valaciclovir recipient developed VZV disease, whereas 2% and 4% of placebo patients did, R+ and D+R- strata respectively. Additionally in D+R- patients, valaciclovir was shown to significantly reduce acute graft rejections (biopsy proven and clinical acute rejection by 57% and 45% respectively) and opportunistic infections (48% primarily bacterial and fungal infections). There were no significant differences in rates of chronic graft rejection. Allograft function and survival, including the proportion of patients with a functional graft at their last assessment were similar between treatment groups.
Valaciclovir was also significantly better than placebo in preventing or delaying the development of viraemia, viruria and clinical HSV disease during the study period. No valaciclovir recipient developed VZV disease, whereas 2% and 4% of placebo patients did, R+ and D+R- strata respectively. Additionally in D+R- patients, valaciclovir was shown to significantly reduce acute graft rejections (biopsy proven and clinical acute rejection by 57% and 45% respectively) and opportunistic infections (48% primarily bacterial and fungal infections). There were no significant differences in rates of chronic graft rejection. Allograft function and survival, including the proportion of patients with a functional graft at their last assessment were similar between treatment groups.






 In patients on haemodialysis the valaciclovir dose recommended for patients with a creatinine clearance of less than 15 mL/min should be used, but the dose should be administered after the haemodialysis has been performed.
In patients on haemodialysis the valaciclovir dose recommended for patients with a creatinine clearance of less than 15 mL/min should be used, but the dose should be administered after the haemodialysis has been performed. The creatinine clearance should be monitored frequently, especially during periods when renal function is changing rapidly e.g. immediately after transplantation or engraftment. The valaciclovir dosage should be adjusted accordingly.
The creatinine clearance should be monitored frequently, especially during periods when renal function is changing rapidly e.g. immediately after transplantation or engraftment. The valaciclovir dosage should be adjusted accordingly.