What is in this leaflet
This leaflet answers some common questions about Arava.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Arava against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Arava is used for
Arava is a type of medicine used to treat rheumatoid or psoriatic arthritis. Arava helps to slow down the process of joint damage and to relieve the symptoms of the disease, such as joint tenderness and swelling, pain and morning stiffness.
Arava works by selectively interfering with the ability of white blood cells called lymphocytes to produce the disease response that ultimately leads to pain, inflammation and joint damage.
Your doctor, however, may have prescribed Arava for another purpose.
Ask your doctor if you have any questions about why it has been prescribed for you.
This medicine is only available with a doctor's prescription.
Before you take it
When you must not take it
Do not take Arava if you:
- have any diseases which reduce your body's natural defences such as bacterial or viral infections
- have any diseases of the blood
- have any serious skin disorders
- have liver disease
- have a condition called hypoproteinaemia (when you do not have enough protein in your blood)
- are pregnant or plan to become pregnant
- are not using reliable birth control
- are breastfeeding
You must not become pregnant while taking Arava and for a certain period of time after stopping Arava. Arava may increase the risk of birth defects.
Women of childbearing potential must use reliable contraception while taking Arava.
Do not take it if you are breastfeeding or planning to breastfeed. Arava passes into breast milk and therefore there is a possibility that the breastfed baby may be affected.
Do not take Arava if you are allergic to it, teriflunomide or any of the ingredients listed at the end of this leaflet. Some symptoms of an allergic reaction include skin rash, itching, shortness of breath or swelling of the face, lips or tongue, which may cause difficulty in swallowing or breathing.
Do not give Arava to a child or adolescent. Arava is not approved for use in children or adolescents under 18 years old.
Do not take it after the expiry date (EXP) printed on the pack. If you take it after the expiry date has passed, it may not work as well.
Do not take it if the packaging is torn or shows signs of tampering.
Before you start to take it
Tell your doctor or pharmacist if you have allergies to:
- any of the ingredients listed at the end of this leaflet
- any other substances, such as foods, preservatives or dyes.
Tell your doctor immediately if you think you could be pregnant while taking Arava.
Tell your doctor if you intend to become pregnant or father a child. Arava may increase the risk of birth defects. To reduce any risk to the developing baby, you will need to stop taking Arava and may need to undergo a wash-out procedure. Your doctor will discuss the wash-out procedure with you.
Tell your doctor if you are breastfeeding or planning to breastfeed.
Tell your doctor if you have or have had any medical conditions, especially the following:
- a decrease in the number of white blood cells
- liver problems
- kidney problems
- chronic infections
- an illness which lowered your body's resistance to disease
- tuberculosis
- lung problems, such as interstitial lung disease (an inflammation of lung tissue) which is a serious and potentially fatal disease
Tell your doctor if you plan to have surgery.
If you have not told your doctor about any of the above, tell them before you take Arava.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with Arava. These include:
- warfarin, a medicine used to stop blood clots
- some medicines used for diabetes
- some medicines used to treat epilepsy
- some medicines used for tuberculosis (TB)
- some medicines used to lower cholesterol
These medicines may be affected by Arava, or may affect how well it works. You may need to use different amounts of your medicine, or take different medicines. Your doctor or pharmacist will advise you.
In certain situations, for example, if you experience a serious side effect, you change your medication or you want to fall pregnant, your doctor will ask you to take medication that will help your body get rid of Arava faster.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking Arava.
How to take it
How much to take
Your doctor will tell you how many tablets you will need to take each day. This depends on your condition and whether or not you are taking any other medicines.
The standard dose for this medicine is one 100 mg tablet per day for the first 3 days, and after that one 10 mg or 20 mg tablet daily.
Your doctor may have prescribed a different dose.
Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
Follow the instructions they give you. These directions may differ from the information contained in this leaflet. If you take the wrong dose, Arava may not work as well.
How to take it
Swallow the tablets whole with a full glass of water.
When to take it
It does not matter if you take Arava before or after food.
Take Arava at about the same time each day. Taking your tablets at the same time each day will have the best effect. It will also help you to remember when to take the tablets.
If you are not sure when to take it, ask your doctor or pharmacist.
How long to take it
Continue taking your medicine for as long as your doctor or pharmacist tells you. The medicine helps control your condition, but it does not cure it. Therefore, you must take it every day.
Ask your doctor or pharmacist if you are not sure how long to take the medicine for.
If you forget to take it
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
If there is still a long time to go before your next dose, take it as soon as you remember, and then go back to taking it as you would normally.
If you are not sure what to do, ask your doctor or pharmacist.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 POISON or 0800 764766), or go to Accident and Emergency at your nearest hospital, if you think you or anyone else may have taken too much Arava.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
Tell all the doctors, dentists and pharmacists who are treating you that you are taking Arava.
If you are about to be started on any new medicine, tell your doctor and pharmacist that you are taking Arava.
If you become pregnant while you are taking this medicine, stop taking it and tell your doctor or pharmacist immediately.
Tell your doctor before stopping contraception. You must continue using appropriate reliable contraception (the 'Pill' or condoms) while you are taking Arava.
If you have an infection or notice a fever or signs of an infection while taking this medicine, tell your doctor immediately.
If your skin becomes itchy or yellow, if the whites of your eyes become yellow, or if you start to bleed or bruise easily, stop taking it and tell your doctor or pharmacist immediately. You may be developing a liver problem. Your doctor may need to take blood samples to monitor the health of your liver and blood cells while you are taking Arava.
Tell your doctor immediately if you develop new or worsening symptoms such as a cough or trouble breathing. Inflammation of the lung tissue which can be fatal, has been reported in some patients.
Tell your doctor if you develop symptoms such as pins and needles or tingling in the hands or feet or numbness or weakness of the arms and legs.
Tell your doctor if you need to have a vaccination during treatment with this medicine or for 6 months after stopping treatment.
Things you must not do
Do not take more than the recommended dose unless your doctor tells you to.
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not use this medicine to treat any other complaints unless your doctor tells you to.
Do not stop taking Arava, or lower the dosage, without checking with your doctor.
Things to be careful of
The effects of alcohol could be made worse while taking Arava. It is recommended that you minimise your alcohol intake while taking Arava.
Side effects
All medicines have some unwanted side effects. Sometimes they are serious, but most of the time they are not. Your doctor or pharmacist has weighed the risks of using this medicine against the benefits they expect it will have for you.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Arava. It helps most people with arthritis, but it may have unwanted side effects in a few people.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- diarrhoea
- rashes, itchy skin
- hair loss
- weight loss
- unusual tiredness or weakness
- nausea and vomiting
- abdominal pain
These are the more common side effects of Arava.
Tell your doctor immediately, or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- signs and symptoms of severe infection eg. Fever
- severe upper stomach pain, often with nausea and vomiting
- severe skin rash or sores in your mouth
- your skin becomes pale, you start to feel tired, you become prone to infections or bruising
- if you develop new or worsening symptoms such as cough or trouble breathing, with or without a fever.
- if you develop blisters and bleeding in the lips, eyes, mouth, nose and genitals.
These may be serious side effects of Arava. You may need urgent medical attention. Serious side effects are uncommon.
Arava decreases your body's immune response and can cause some of the side effects listed above.
If any of the following happen, stop taking this medicine and tell your doctor immediately, or go to Accident and Emergency at your nearest hospital:
- swelling of the face, lips, mouth or throat, which may cause difficulty in swallowing or breathing
- hives
- fainting
- yellowing of the skin and eyes (jaundice)
- thickened patches of red skin
These are very serious side effects. If you have them, you may have had a serious allergic reaction to Arava. You may need urgent medical attention or hospitalisation.
These side effects are very rare.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some consumers.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
After taking it
Storage
Keep your tablets in the container until it is time to take them. If you take the tablets out of the box or the blister pack they may not keep well.
Keep the medicine in a cool dry place where the temperature stays below 25°C.
Do not store it or any other medicine in the bathroom or near a sink.
Do not leave it in the car on hot days or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it.
Disposal
If your doctor or pharmacist tells you to stop taking Arava or the medicine has passed its expiry date, ask your pharmacist what to do with any that are left over.
Return any unused medicine to your pharmacist.
Product description
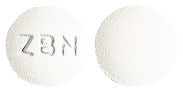
What it looks like
Arava 10 mg tablets are white to almost white, round film-coated tablets with the embossing ZBN. Arava 10mg tablets are supplied in bottles in packs of 10# and 30 tablets.
Arava 20 mg tablets are yellowish to ochre, spherical triangular film-coated tablets with the embossing ZBO. Arava 20mg tablets are supplied in bottles in packs of 10# and 30 tablets.
Arava 100 mg tablets are white to almost white, round film-coated tablets with the embossing ZBP. Arava 100mg tablets are supplied in blisters in packs of 3.
#Presentations currently not marketed.
Ingredients
Active Ingredient:
Each tablet contains 10 mg, 20 mg or 100 mg of the active ingredient, leflunomide.
Inactive Ingredients:
- lactose monohydrate
- maize starch
- povidone
- colloidal anhydrous silica
- magnesium stearate
- crospovidone
- hypromellose
- macrogol 8000
- purified talc
- titanium dioxide
- iron oxide yellow (20 mg tablet only)
Arava does not contain sucrose, gluten, tartrazine or any other azo dyes.
Manufacturer/Sponsor
Arava is supplied in Australia by:
sanofi-aventis australia pty ltd
12-24 Talavera Road
Macquarie Park NSW 2113
Freecall No: 1800 818 806
Arava is supplied in New Zealand by:
sanofi -aventis new zealand limited
Level 8, 56 Cawley Street
Ellerslie, Auckland 1051
Freecall No: 0800 283 684
Australian Registration Number(s):
Arava 10 mg AUST R 69692
Arava 20 mg AUST R 69694
Arava 100 mg AUST R 69695
This leaflet was prepared in April 2020
arava-ccdsv18-19-cmiv14-28apr20
Published by MIMS June 2020


 In addition, the following adverse events have been reported in 1% to 3% of the RA patients in the leflunomide treatment group in controlled clinical trials. See Table 2.
In addition, the following adverse events have been reported in 1% to 3% of the RA patients in the leflunomide treatment group in controlled clinical trials. See Table 2. Other less common adverse events seen in clinical trials include: 1 case of anaphylactic reaction occurred in phase II following rechallenge of drug after withdrawal due to rash (rare); urticaria, transient thrombocytopenia (uncommon), eosinophilia (rare); and leukopenia < 2 x 109/L (rare). A causal relationship of these events to leflunomide has not been established.
Other less common adverse events seen in clinical trials include: 1 case of anaphylactic reaction occurred in phase II following rechallenge of drug after withdrawal due to rash (rare); urticaria, transient thrombocytopenia (uncommon), eosinophilia (rare); and leukopenia < 2 x 109/L (rare). A causal relationship of these events to leflunomide has not been established. ACR 20, 50 and 70% response rates in all treatment groups of the US301 trial are shown in Figure 2. In US301, the ACR 20% response rate of patients treated with Arava was significantly increased from that seen in placebo treated patients and similar to that seen in patients treated with methotrexate. Similarly, ACR 50% and 70% responses were approximately two times higher in patients treated with Arava or methotrexate than in patients who received placebo.
ACR 20, 50 and 70% response rates in all treatment groups of the US301 trial are shown in Figure 2. In US301, the ACR 20% response rate of patients treated with Arava was significantly increased from that seen in placebo treated patients and similar to that seen in patients treated with methotrexate. Similarly, ACR 50% and 70% responses were approximately two times higher in patients treated with Arava or methotrexate than in patients who received placebo.



 The use of a loading dose may increase toxicity associated with leflunomide when used in children. The population pharmacokinetic data indicate that adult doses of leflunomide would be inappropriate in some children who would require a dose calculated from bodyweight. The safety and effectiveness of Arava in paediatric patients have not been fully evaluated. Arava is not recommended for use in patients under 18 years.
The use of a loading dose may increase toxicity associated with leflunomide when used in children. The population pharmacokinetic data indicate that adult doses of leflunomide would be inappropriate in some children who would require a dose calculated from bodyweight. The safety and effectiveness of Arava in paediatric patients have not been fully evaluated. Arava is not recommended for use in patients under 18 years. In a differing analysis which excluded some patients, the Psoriasis Area and Severity Index (PASI) was assessed to reflect changes in the extent and severity of psoriasis lesions as judged by erythema, desquamation, and infiltration. Arava resulted in a significant improvement in PASI scores over the 24 week study relative to placebo, with a mean (± SD) improvement of 22.4% (± 51.6%) in the leflunomide group compared with a deterioration of 2.2% (± 70.4%) in the placebo group (p = 0.0030). See Table 5.
In a differing analysis which excluded some patients, the Psoriasis Area and Severity Index (PASI) was assessed to reflect changes in the extent and severity of psoriasis lesions as judged by erythema, desquamation, and infiltration. Arava resulted in a significant improvement in PASI scores over the 24 week study relative to placebo, with a mean (± SD) improvement of 22.4% (± 51.6%) in the leflunomide group compared with a deterioration of 2.2% (± 70.4%) in the placebo group (p = 0.0030). See Table 5. Compared with the placebo group, a significantly greater proportion of patients in the leflunomide group experienced a ≥ 50% reduction in PASI scores (PASI 50; 18.9% vs 30.4%; p = 0.050) a ≥ 75% reduction in PASI scores (PASI 75; 7.8% vs 17.4%; p = 0.048) from baseline.
Compared with the placebo group, a significantly greater proportion of patients in the leflunomide group experienced a ≥ 50% reduction in PASI scores (PASI 50; 18.9% vs 30.4%; p = 0.050) a ≥ 75% reduction in PASI scores (PASI 75; 7.8% vs 17.4%; p = 0.048) from baseline. Relative to an oral solution, Arava tablets are 80% bioavailable. Food does not affect the bioavailability of Arava.
Relative to an oral solution, Arava tablets are 80% bioavailable. Food does not affect the bioavailability of Arava.
 Molecular formula: C12H9F3N2O2.
Molecular formula: C12H9F3N2O2.