What is in this leaflet
This leaflet answers some common questions about BACTRIM DS tablets and BACTRIM oral suspension (mixture is another name that can be used instead of oral suspension). It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking BACTRIM against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What BACTRIM is used for
BACTRIM contains the active ingredients sulfamethoxazole and trimethoprim, also known as co-trimoxazole.
BACTRIM is used to treat bacterial infections in different parts of the body.
BACTRIM belongs to a group of medicines called antibiotics. There are many different types of medicines used to treat bacterial infections. Sulfamethoxazole in BACTRIM belongs to a group of medicines known as sulfonamides. Trimethoprim belongs to a group of medicines known as the benzylpyrimidines.
BACTRIM works by stopping the growth of the bacteria causing the infection.
BACTRIM does not work against infections caused by viruses, such as colds and flu.
BACTRIM has been prescribed for your current infection. Another infection later on may require a different medicine.
Your doctor may have prescribed BACTRIM for another purpose.
Ask your doctor if you have any questions why BACTRIM has been prescribed for you.
This medicine is available only with a doctor's prescription.
Before you take BACTRIM
When you must not take it
Do not take BACTRIM if:
-
you have had an allergic reaction to sulfamethoxazole, trimethoprim, any other sulfonamide, or any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- skin rash
- peeling of the skin
- itching or hives
- swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing
- wheezing or shortness of breath. - you have severe liver or kidney disease, any blood disorder or megaloblastic anaemia
- the child you are treating is less than 3 months of age
- you have streptococcal pharyngitis
- the package is torn or shows signs of tampering
- you are taking dofetilide, a medicine used to treat irregular heartbeats
-
the expiry date (EXP) printed on the pack has passed
If you take this medicine after the expiry date has passed, it may not work as well.
If you are not sure if you should be taking BACTRIM, talk to your doctor.
Before you start to take it
Your doctor must know about all the following before you can start to take BACTRIM.
Tell your doctor if:
-
you are pregnant or intend to become pregnant
If BACTRIM is taken during pregnancy, it may harm the baby. Your doctor will discuss the risks and benefits of taking BACTRIM during pregnancy. -
you are breast-feeding or plan to breast-feed
BACTRIM passes into breast milk. Your doctor will discuss the risks and benefits of taking BACTRIM while breast-feeding. -
you have any other health problems including:
- an allergic reaction to any diuretic (fluid) tablet or medicines for diabetes or overactive thyroid. This may increase your chances of an allergic reaction to BACTRIM
- any type of blood disorder (including porphyria and glucose-6-phosphate dehydrogenase deficiency)
- kidney or liver disease
- a hereditary disorder called phenylketonuria
- epilepsy (fits or convulsions)
- asthma
- allergic disorders
- rheumatoid arthritis
- urinary obstruction
- folic acid deficiency - you are allergic to any other medicines, foods, dyes or preservatives
Taking other medicines
Tell your doctor if you are taking any other medicines including any that you have bought from a pharmacy, supermarket or healthfood shop.
Some medicines may interfere with BACTRIM. These medicines include:
- medicines used to treat diabetes such as repaglinide, rosiglitazone, pioglitazone, glibenclamide, gliclazide, glipizide, chlorpropamide and tolbutamide
- fluid tablets (diuretics)
- phenytoin, a medicine for epilepsy
- pyrimethamine, a medicine for malaria
- other medicines used to treat infections such as rifampicin, dapsone and polymyxin
- zidovudine, a medicine to treat HIV infection
- cyclosporin, a medicine used to treat organ transplant patients
- warfarin, acenocoumarol, phenprocoumon, medicines used to thin the blood
- medicines used to treat certain heart conditions such as digoxin and amiodarone
- amantadine, a medicine used to treat the influenza virus and Parkinson's Disease
- memantine, a medicine used to treat Parkinson's disease
- urinary acidifiers (for kidney conditions)
- oral contraceptives ("The Pill")
- sulfinpyrazone, a medicine used to treat gout
- salicylates, medicines to treat conditions such as psoriasis or warts
- medicines used to treat cancer such as paclitaxel, mercaptopurine and methotrexate
- clozapine, a medicine used to treat schizophrenia
- medicines used to treat overactive thyroid conditions
- medicines used to treat depression such as imipramine, clomipramine, amitriptyline, dothiepin, doxepin, nortriptyline and trimipramine
- immunosuppressant medicines such as azathioprine and methotrexate
- medicines used to treat high blood pressure as well as a variety of heart and kidney conditions such as captopril, enalapril, lisinopril, fosinopril, perindopril, quinapril, ramipril, trandolapril valsartan, telmisartan, irbesartan, candesartan, eprosartan, losartan, dofetilide and olmesartan.
These medicines may be affected by BACTRIM or may affect how well it works. You may need to use different amounts of your medicine, or you may need to take different medicines. Your doctor will advise you.
Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking BACTRIM.
If you have not told your doctor about any of the above, tell them before you start taking BACTRIM.
Use in very young children
BACTRIM should not be given to premature babies or children younger than 3 months of age.
Use in People Over 65 Years
People over 65 years are more at risk of severe side effects when taking BACTRIM. The risk is greater if you have kidney or liver disease or are taking some types of other medicines, such as diuretics.
Use in People with HIV infection
People with HIV infection have been reported to get more side effects while being treated with BACTRIM than people without HIV.
How to take BACTRIM
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
How much to take
Take BACTRIM exactly as your doctor has prescribed.
Your doctor will tell you how much BACTRIM to take each day.
The dose and length of time you have to take BACTRIM will depend on the type of infection you have.
For adults and children over 12 years, the usual dose of BACTRIM DS is one tablet twice per day.
For children under 12 years of age, the dose of BACTRIM oral suspension depends on the age and weight of your child. Your doctor or pharmacist will tell you how much your child should be given.
How to take it
Swallow BACTRIM DS tablets whole (or halve them if necessary) with a glass of water.
The correct amount of BACTRIM oral suspension should be measured, using a metric measure, before being given by mouth.
When to take it
Take BACTRIM DS tablets or oral suspension after a meal.
How long to take BACTRIM
Continue taking BACTRIM until your doctor tells you to stop. The full course of BACTRIM prescribed by your doctor should be taken, even if you feel better after a few days. This will help clear your infection completely.
If your symptoms do not improve within a few days, or if they become worse, let your doctor know.
If you forget to take BACTRIM
Do not take an extra dose. Wait until the next dose and take your normal dose then.
Do not try to make up for the dose that you missed by taking more than one dose at a time.
If you are not sure what to do, ask your doctor or pharmacist.
In case of an overdose
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much BACTRIM even, if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much BACTRIM, you may feel sick or vomit, feel dizzy, depressed or confused or have a headache. You may also feel drowsy or become unconscious.
Keep telephone numbers for these places handy.
If you are not sure what to do, contact your doctor or pharmacist.
While you are taking BACTRIM
Things you must do
Tell all doctors, dentists and pharmacists who are treating you that you are taking BACTRIM.
Tell your doctor if you become pregnant while taking BACTRIM.
Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed. Otherwise, your doctor may think that it was not effective and change your treatment unnecessarily.
Tell your doctor if you feel the tablets or oral suspension is not helping your condition.
Drink plenty of fluids while you are taking BACTRIM. This will help to flush the medicine through your system.
If you are taking BACTRIM for a long time, visit your doctor regularly so your progress can be checked. Your doctor may ask you to have regular tests to check your kidneys, liver or blood.
Tell your doctor you are taking BACTRIM if you have to have any blood tests. BACTRIM may affect the results of some blood tests.
Contact your doctor immediately if you get severe diarrhoea, even if it develops several weeks after stopping BACTRIM. DO NOT take any diarrhoea medicine without first checking with your doctor. Diarrhoea medicines may make your diarrhoea worse or make it last longer.
Things you must not do
Do not stop taking BACTRIM or change the dose without first checking with your doctor.
Do not let yourself run out of medicine over the weekend or on holidays.
Do not give BACTRIM to anyone else even if their symptoms seem similar to yours.
Do not use BACTRIM to treat other complaints unless your doctor says to.
Do not take any other medicines whether they require a prescription or not without first telling your doctor or consulting with a pharmacist.
Things to be careful of
Be careful driving or operating machinery until you know how BACTRIM affects you.
Sometimes use of this medicine allows other bacteria and fungi which are not sensitive to BACTRIM to grow. If other infections such as thrush occur while you are taking BACTRIM, tell your doctor.
If you are going outdoors, wear protective clothing or use a SPF 15+ sunscreen. Your skin may burn more easily while you are taking BACTRIM.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking BACTRIM. BACTRIM helps most people with susceptible infections but it may have unwanted side effects in a few people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
If side effects do occur, they may be:
- nausea, with or without vomiting
- diarrhoea or other abdominal (gut) or stomach discomfort
These side effects are not usually serious or long lasting.
Tell your doctor if you notice these side effects and they worry you:
- oral thrush (white, furry sore tongue and mouth)
- vaginal thrush (sore itchy vagina with vaginal discharge)
Your doctor will need to treat the thrush infection separately.
Tell your doctor immediately if you notice any of the following:
- jaundice (yellowing of the skin)
- severe or watery diarrhoea
- any type of skin rash, peeling of the skin, severe itching or hives
- fever, sore throat, lumps in the neck
- cough, shortness of breath
- severe persistent headache
- discolouration of urine
- swelling of the face and throat
These symptoms are usually rare but may be serious and need urgent medical attention.
Very rarely, people have died from complications due to certain severe skin, liver or blood reactions. Elderly people, people with liver or kidney disease and people taking certain other medicines are more at risk of these severe reactions.
Other rare side effects include:
- other allergic reactions
- pins and needles in the hands and feet
- loss of appetite, fits, headaches, depression, imagined sensations or nervousness
- increased or decreased urine production
- unsteadiness or dizziness
- sleeplessness, weakness, tiredness, increased sensitivity to light and stomach pains.
If you experience any of these effects contact your doctor as soon as possible.
This is not a complete list of all possible side effects. Others may occur in some people and there may be some side effects not yet known.
Tell your doctor if you notice anything else that is making you feel unwell, even if it is not on this list.
Ask your doctor or pharmacist if you don't understand anything in this list.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking BACTRIM
Storage
Keep your BACTRIM DS tablets in the blister pack until it is time to take them.
Keep the oral suspension in the bottle until it is time to take it. If you take the tablets out of the blister pack or the oral suspension out of the bottle before it is time to take them, they may not keep well.
Keep BACTRIM in a cool dry place where the temperature stays below 30°C.
Do not store it, or any other medicine, in a bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Keep BACTRIM where young children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking BACTRIM, or the tablets or oral suspension has passed its expiry date, ask your pharmacist what to do with any medicine that is left over.
Product Description
Availability
BACTRIM is available as tablets (800 mg/ 160 mg) or as an oral suspension (mixture) 200 mg/ 40 mg per 5 mL).
BACTRIM comes in the following pack sizes:
- BACTRIM DS - 10 tablets per carton
- BACTRIM oral suspension - 100 mL per bottle
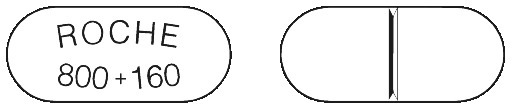
What BACTRIM looks like
BACTRIM DS tablets are white to almost white, oblong, with a breakline on one side and "ROCHE 800 + 160" on the other side.
The tablets have a breakline so that they can be broken in half if needed.
BACTRIM oral suspension is light beige in colour with a banana flavour.
Ingredients
Active ingredient
BACTRIM DS tablets and BACTRIM oral suspension contain the active ingredients trimethoprim and sulfamethoxazole.
- each BACTRIM DS tablet contains 160 mg of trimethoprim and 800 mg of sulfamethoxazole.
- each 5 mL of BACTRIM oral suspension contains 40 mg of trimethoprim and 200 mg of sulfamethoxazole.
Inactive ingredients
BACTRIM DS tablets also contain:
- povidone (1201)
- docusate sodium (480)
- sodium starch glycollate
- magnesium stearate (470)
BACTRIM DS tablets are gluten free and lactose free.
BACTRIM oral suspension also contains:
- Cellulose - dispersible (460)
- methyl hydroxybenzoate (218)
- propyl hydroxybenzoate (216)
- sorbitol solution (420)
- polysorbate 80 (433)
- banana flavour 85509 H
- vanilla flavour 73690-36
- water
BACTRIM oral suspension is gluten free and sugar free.
Distributor
BACTRIM is distributed by:
Roche Products Pty Limited
ABN 70 000 132 865
Level 8, 30 - 34 Hickson Road
Sydney NSW 2000
AUSTRALIA
Medical enquiries: 1800 233 950
Please check with your pharmacist for the latest Consumer Medicine Information.
Australian Registration numbers:
BACTRIM DS tablets:
- AUST R 162563
BACTRIM Oral suspension:
- AUST R 119404
This leaflet was prepared 29 April 2019.
Published by MIMS July 2019