What is in this leaflet
Please read this leaflet carefully before you start taking BRAFTOVI.
This leaflet answers some common questions about BRAFTOVI. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking BRAFTOVI against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What BRAFTOVI is used for
BRAFTOVI is an anti-cancer medicine containing the active ingredient encorafenib, which belongs to a group of medicines called ‘BRAF inhibitors’.
BRAFTOVI is used in combination with another medicine which contains the active ingredient binimetinib (called MEKTOVI®) to treat adult patients with a type of skin cancer called melanoma, which has spread to other parts of the body, or cannot be removed by surgery. The type of melanoma which BRAFTOVI and MEKTOVI are used to treat has a particular change (mutation) in a gene called BRAF. This mutation in the BRAF gene may have produced proteins which caused the melanoma to develop. BRAFTOVI targets proteins made from this modified BRAF gene.
BRAFTOVI can only be used to treat patients whose melanoma has this particular mutation in the BRAF gene.
Before you start treatment, your doctor will have tested you to confirm that you have this BRAF mutation.
When BRAFTOVI is used in combination with MEKTOVI, it slows down or stops the growth of your cancer.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is available only with a doctor's prescription.
BRAFTOVI is not recommended for children and adolescents aged under 18 years. The safety and efficacy of this medicine has not been established in this age group.
Before you take BRAFTOVI
As BRAFTOVI is to be used in combination with MEKTOVI, you must also read the Consumer Medicine Information for MEKTOVI.
When you must not take it
Do not take BRAFTOVI if you have an allergy to:
- any medicine containing encorafenib
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
If you experience an allergic reaction, stop taking the medicine and inform your doctor or pharmacist immediately.
Do not take BRAFTOVI after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. The expiry date refers to the last day of that month. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor, nurse or pharmacist if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions, especially the following:
- heart problems, including alteration of the electrical activity of your heart (QT prolongation)
- liver problems
- kidney problems
- bleeding problems, or if you are taking medicines that may increase your risk of bleeding
- eye problems
Tell your doctor if you have had a different type of cancer than melanoma as BRAFTOVI may cause progression of certain other types of cancers.
Pregnancy
Taking BRAFTOVI during pregnancy is not recommended. Tell your doctor if you are pregnant, think you may be pregnant or are planning to become pregnant before taking BRAFTOVI.
BRAFTOVI may cause permanent harm or birth defects to an unborn baby.
Breast-feeding
BRAFTOVI is not recommended while breast-feeding. If you are breastfeeding or planning to breastfeed, you must tell your doctor before taking this medicine.
It is not known if BRAFTOVI passes into breastmilk.
If you have not told your doctor about any of the above, tell them before you start taking BRAFTOVI.
Fertility
BRAFTOVI may temporarily reduce male fertility by causing a reduced sperm count. This could affect the ability to father a child. Talk to your doctor about any concerns you may have regarding your fertility while taking BRAFTOVI.
Taking other medicines
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and BRAFTOVI may interfere with each other. These include:
- some medicines to treat fungal infections (such as itraconazole, posaconazole, fluconazole)
- some medicines to treat bacterial infections (such as rifampicin, clarithromycin, telithromycin, erythromycin, penicillin)
- medicines typically used to treat epilepsy (seizures) (such as phenytoin, carbamazepine)
- medicines typically used to treat cancer (such as, imatinib)
- a herbal treatment for depression: St. John’s wort
- some medicines for HIV treatment such as ritonavir or amprenavir
- birth control medicines containing hormones
- medicines typically used to treat high blood pressure (such as diltiazem, furosemide)
- a medicine used to treat an uneven heartbeat: amiodarone.
These medicines may be affected by BRAFTOVI or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Keep a list of the medicines you take so you can show it to your doctor, nurse or pharmacist when you get a new medicine.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking BRAFTOVI.
How to take BRAFTOVI
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions in this leaflet, ask your doctor or pharmacist for help.
How much to take
Always take BRAFTOVI exactly as your doctor has prescribed.
The recommended dose of BRAFTOVI, when taken in combination with MEKTOVI, is six 75 mg capsules once daily (corresponding to a daily dose of 450 mg).
If you have liver or kidney problems, your doctor may start you on a lower dose of BRAFTOVI. If you experience serious side effects (such as skin, heart, liver, eye or bleeding problems), your doctor may lower the dose of BRAFTOVI, or stop treatment temporarily or permanently.
How to take it
Swallow the capsules whole with a full glass of water.
BRAFTOVI can be taken with or without food. Avoid grapefruit juice.
If vomiting occurs at any time after taking the capsules, do not take an additional dose. Take the next dose as scheduled.
How long to take it
Continue taking BRAFTOVI for as long as your doctor tells you to.
Do not stop unless your doctor advises you to.
If you forget to take it
If you miss a dose of BRAFTOVI:
- If the missed dose is less than 12 hours late, take it as soon as you remember.
- If the missed dose is more than 12 hours late, skip that dose and take your next dose at the usual time. Then go back to taking your capsules as you would normally.
Do not take a double dose to make up for the dose that you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your doctor, nurse or pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (In Australia telephone 13 11 26. In New Zealand telephone 0800 764 766) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much BRAFTOVI. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking BRAFTOVI
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking BRAFTOVI.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking BRAFTOVI.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking BRAFTOVI.
If you become pregnant while taking BRAFTOVI, tell your doctor immediately.
If you are a woman who could become pregnant, you must use effective birth control (contraception) while you are taking BRAFTOVI, and you must continue to use effective contraception for at least 1 month after taking your last dose.
Birth control medicines containing hormones (such as pills, injections, patches, implants and certain intrauterine devices (IUDs) which release hormones) may not work as well as expected while you are taking BRAFTOVI. You will need to use another reliable method of birth control such as a barrier method (e.g. condom) to prevent falling pregnant while you are taking BRAFTOVI. Ask your doctor, pharmacist or nurse for advice.
Tell your doctor if you are breastfeeding while being treated with BRAFTOVI.
Tell your doctor, nurse or pharmacist immediately if you experience the following while you are taking BRAFTOVI.
Skin changes
BRAFTOVI may cause other types of skin cancer such as cutaneous squamous cell carcinoma. New melanoma lesions may also occur while taking BRAFTOVI.
Your doctor will periodically check for new cancers on your skin and inside your body before, during and after your treatment with BRAFTOVI. Tell your doctor immediately if you detect any skin changes including new warts, skin soreness, reddish bumps which bleed or don’t heal, or any changes in the size or colour of a mole.
Heart problems
BRAFTOVI when taken with MEKTOVI can lower the amount of blood pumped by your heart, alter the electrical activity of your heart, or make existing heart problems worse. Your doctor will run tests to check that your heart is working properly before and during your treatment with these medicines.
Bleeding problems
BRAFTOVI when taken with MEKTOVI may cause serious bleeding problems. Tell your doctor immediately if you have any signs of bleeding.
Eye problems
BRAFTOVI when taken with MEKTOVI can cause serious eye problems. Your doctor will examine your eyes for any new or worsening problems with your sight while you are taking these medicines.
Liver problems
BRAFTOVI can increase the amounts of liver enzymes in your blood. Your doctor will run blood tests to monitor your liver function before and during treatment.
Kidney problems
BRAFTOVI can alter your kidney activity (often abnormal blood tests, more rarely dehydration and vomiting). Your doctor will run blood tests to monitor your kidneys before and during treatment. Drink plenty of fluids during treatment. Tell your doctor immediately if you vomit and become dehydrated
Keep all of your doctor's appointments so that your progress can be checked.
Things you must not do
Do not take BRAFTOVI to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if their symptoms seem similar to yours or they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
BRAFTOVI can affect your ability to drive or use machines. Be careful driving or operating machinery until you know how BRAFTOVI affects you. If you experience any problems with your vision, or any other side-effects that may affect your ability, avoid driving or using machines. Talk to your doctor if you are not sure if you should drive.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking BRAFTOVI.
Like other medicines, BRAFTOVI can cause side effects but not everybody gets them. Some may be serious and need medical attention.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Possible serious side effects
BRAFTOVI may cause serious side effects. Tell your doctor immediately if you experience any of the following serious side effects, either for the first time or if they get worse.
Heart problems
BRAFTOVI when taken with MEKTOVI can affect how well your heart pumps (left ventricular ejection fraction decrease) alter the electrical activity of your heart (QT interval prolongation), or make existing heart problems worse. Signs and symptoms can include:
- feeling dizzy, tired or lightheaded
- shortness of breath
- feeling like your heart is pounding, racing or beating irregularly
- swelling in the legs ¨
Bleeding problems
BRAFTOVI when taken with MEKTOVI can cause serious bleeding problems. Tell your doctor immediately if you have any unusual bleeding or signs of bleeding including:
- headaches, dizziness or weakness
- coughing up of blood or blood clots
- vomit containing blood or that looks like “coffee grounds”
- red or black stools that look like tar
- passing blood in the urine
- stomach (abdominal) pain
- unusual vaginal bleeding
Eye problems
BRAFTOVI when taken with MEKTOVI can induce serious eye problems such as fluid leakage under the retina in the eye that results in detachment of different layers in the eye (retinal pigment epithelial detachment). Tell your doctor immediately if you experience the following problems with your eyes:
- blurred vision, loss of vision or other vision changes (e.g. coloured dots in your vision)
- halo (seeing blurred outline around objects)
- eye pain, swelling or redness
Muscle problems
BRAFTOVI when taken with MEKTOVI may lead to the breakdown of muscles (rhabdomyolysis) which can lead to kidney damage and can be fatal. Signs and symptoms can include:
- muscle pain, cramps, stiffness or spasm
- dark urine
Other skin cancers
BRAFTOVI may cause other types of skin cancer such as cutaneous squamous cell carcinoma. Usually these skin cancers can be removed with surgery and treatment with BRAFTOVI and MEKTOVI can be continued without interruption.
New melanoma lesions may also appear while taking BRAFTOVI. These melanomas are usually removed by surgery and treatment with BRAFTOVI and MEKTOVI can be continued without interruption.
Other side effects
Besides the serious side effects mentioned above, taking BRAFTOVI may cause other side effects.
When BRAFTOVI was taken with MEKTOVI the following side effects were reported.
Very common side effects (may affect more than 1 in 10 people):
- reduced red blood cell count (anaemia)
- problems with nerves that can cause pain, loss of sensation or tingling in hands and feet
- headache
- dizziness
- bleeding at various sites in the body
- high blood pressure
- problems with your vision (visual impairment)
- stomach pain
- diarrhoea
- being sick (vomiting)
- feeling sick (nausea)
- constipation
- itching
- dry skin
- abnormal hair loss or thinning (alopecia)
- skin rash of various types
- thickening of the outer layers of the skin
- joint pain (arthralgia)
- muscle pain (myalgia), weakness or spasm
- back pain
- pain in the hands and feet
- fever
- swelling of the hands or feet (peripheral oedema), localised swelling
- fatigue
- abnormal blood test results for liver function
- abnormal blood test results related to blood creatine kinase, indicating damage to the heart and muscle
Common side effects (may affect up to 1 in 10 people)
- some types of skin tumours such as skin papilloma and basal cell carcinoma
- allergic reaction that may include swelling of the face and difficulty breathing
- changes in the way things taste
- inflammation of the eye (uveitis)
- blood clots
- inflammation of the colon (colitis)
- redness, chapping or cracking of the skin
- inflammation of the fatty layer under the skin, symptoms include tender skin nodules
- skin rash with a flat discoloured area or raised bumps like acne (dermatitis acneiform)
- redness, skin peeling or blisters on the hands and feet (palmar-plantar erythrodysaesthesia or hand and foot syndrome)
- kidney failure
- abnormal kidney test results (creatinine elevations)
- abnormal blood test results for liver function (blood alkaline phosphatase)
- abnormal blood test results for pancreas function (amylase, lipase)
- increased skin sensitivity to sunlight
Uncommon side effects (may affect up to 1 in 100 people)
- weakness and paralysis of the face muscles (facial paresis)
- inflammation of the pancreas (pancreatitis) causing severe abdominal pain
When BRAFTOVI was used alone the following side effects were reported.
If you continue Braftovi on its own while the other medicine (binimetinib) is temporarily stopped based on your doctor’s decision, you may get some of the side effects given in the lists above, although the frequency may change (increase or decrease)
Very common side effects (may affect more than 1 in 10 people)
- fatigue
- being sick (vomiting)
- feeling sick (nausea)
- constipation
- skin rash of various types
- redness, skin peeling or blisters on hands and feet (called palmar-plantar erythrodysaesthesia or hand and foot syndrome)
- thickening of the outer layers of the skin (hyperkeratosis)
- itching
- dry skin
- abnormal hair loss or thinning (alopecia)
- redness, chapping or cracking of the skin
- skin darkening
- loss of appetite
- difficulty sleeping (insomnia)
- headache
- problems with nerves which can cause pain, loss of sensation or tingling in hands and feet
- changes in the way things taste
- joint pain (arthralgia)
- muscle pain, spasm or weakness
- pain in the extremities
- back pain
- fever
- some types of benign (non-cancerous) skin tumours such as melanocyte naevus and skin papilloma
- abnormal blood tests results related to the liver
Common side effects (may affect up to 1 in 10 people)
- allergic reaction which may include swelling of the face and difficulty breathing
- weakness and paralysis of face muscles
- fast heart beat
- skin rash with a flat discoloured area or raised bumps like acne (dermatitis acneiform)
- peeling or scaly skin
- inflammation of joints (arthritis)
- kidney failure
- abnormal kidney test results (creatinine elevations)
- increased skin sensitivity to sunlight
- abnormal blood test result for pancreas function (lipase)
- Uncommon side effects (may affect up to 1 in 100 people)
- type of skin cancer such as basal cell carcinoma
- inflammation of the eye (uveitis)
- inflammation of the pancreas (pancreatitis)causing severe abdominal pain
- abnormal blood test result for pancreas function (amylase)
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After using BRAFTOVI
Storage
Keep your BRAFTOVI capsules in their original pack until it is time to take them. Keep your BRAFTOVI capsules in a place where the temperature stays below 25°C.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Do not store BRAFTOVI or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Do not throw any medicines away via wastewater or household waste.
Product description
What it looks like
BRAFTOVI 50 mg hard capsules are supplied in blister packs of 28 capsules (7 strips of 4 capsules).
The 50 mg capsules have an orange opaque cap and a flesh-coloured opaque body, with a stylised “A” printed on the cap and “LGX 50 mg” printed on the body.
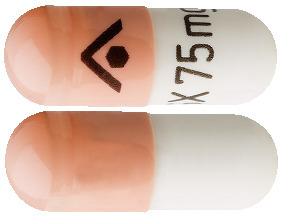
BRAFTOVI 75 mg hard capsules are supplied in blister packs of 42 capsules (7 strips of 6 capsules).
The 75 mg capsules have a flesh-coloured opaque cap and a white opaque body, with a stylised “A” printed on the cap and “LGX 75 mg” printed on the body.
Ingredients
BRAFTOVI contains 50 or 75 mg of encorafenib as the active ingredient.
Capsule fill:
- copovidone
- poloxamer
- microcrystalline cellulose
- succinic acid
- crospovidone
- colloidal anhydrous silica
- magnesium stearate
Capsule shell:
- gelatin
- titanium dioxide
- iron oxide red
- iron oxide yellow
- iron oxide black
Printing ink:
- shellac
- iron oxide black
- propylene glycol
Supplier
BRAFTOVI is supplied in Australia by:
Pierre Fabre Australia Pty Limited
901/1 Elizabeth Plaza
North Sydney NSW 2060 Australia
® = Registered Trademark
This leaflet was prepared in August 2019.
50 mg: AUST R 295764
75 mg: AUST R 295441
Internal document code
(Aus Braftovi CMI v5 based on Aus Braftovi PI v8)
Published by MIMS October 2019


 If encorafenib is temporarily interrupted, interrupt binimetinib.
If encorafenib is temporarily interrupted, interrupt binimetinib. If encorafenib is permanently discontinued, cetuximab should be discontinued.
If encorafenib is permanently discontinued, cetuximab should be discontinued.





 The efficacy results based on investigator assessment were consistent with the independent central assessment. The PFS analysis per investigator assessment showed an improvement of PFS in patients treated with Combo 450 compared with patients treated with vemurafenib (14.8 vs 7.3 months, respectively), HR 0.49 (95% CI 0.37, 0.64) (p < 0.001 one sided).
The efficacy results based on investigator assessment were consistent with the independent central assessment. The PFS analysis per investigator assessment showed an improvement of PFS in patients treated with Combo 450 compared with patients treated with vemurafenib (14.8 vs 7.3 months, respectively), HR 0.49 (95% CI 0.37, 0.64) (p < 0.001 one sided).





