What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about escitalopram.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine.
You may want to read it again.
What this medicine is used for
The name of your medicine is Chemmart Escitalopram. It contains the active ingredient, escitalopram (as escitalopram oxalate).
It is used to treat
- depression
- obsessive-compulsive disorder.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
How it works
Escitalopram belongs to a group of medicines called Selective Serotonin Reuptake Inhibitors (SSRIs). Escitalopram and other SSRIs are thought to help by increasing the amount of serotonin in your brain.
Depression is longer lasting or more severe than the "low moods" everyone has from time to time due to the stress of everyday life. It is thought to be caused by a chemical imbalance in parts of the brain. This imbalance affects your whole body and can cause emotional and physical symptoms such as feeling low in spirit, loss of interest in activities, being unable to enjoy life, poor appetite or overeating, disturbed sleep, often waking up early, loss of sex drive, lack of energy and feeling guilty over nothing.
Escitalopram corrects this chemical imbalance and may help relieve the symptoms of depression.
There is no evidence that escitalopram is addictive. However, if you suddenly stop taking it, you may get side effects.
Tell your doctor if you get any side effects after stopping escitalopram.
Use in children
Do not give this medicine to a child or adolescent.
There is no experience with its use in children and adolescents under 18 years of age.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You are taking the following other medicines:
- pimozide, used to treat disorders which affect the way you think, feel or act
- monoamine oxidase inhibitors (MAOIs), used to treat depression (phenelzine, tranylcypromine, moclobemide), Parkinson's Disease (selegiline) or infections (linezolid).
Do not take escitalopram until 14 days after stopping most MAOIs. The exception is the MAOI, moclobemide, where you may take escitalopram one whole day after finishing taking moclobemide. Similarly, do not take any MAOI until at least 14 days after stopping taking escitalopram.
Taking escitalopram with MAOIs may cause a serious reaction with signs such as a sudden increase in body temperature, very high blood pressure, rigid muscles, nausea/vomiting and/or fits (convulsions). Your doctor will know when it is safe to start escitalopram after the MAOI has been stopped. - The expiry date (EXP) printed on the pack has passed.
- The packaging is torn, shows signs of tampering or it does not look quite right.
- You have had an allergic reaction to escitalopram, citalopram or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin; fainting or hayfever-like symptoms.
If you think you are having an allergic reaction do not take any more of the medicine and contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances such as foods, preservatives, lactose or dyes.
- You have or have had any medical conditions, especially the following:
- mania, hypomania, bipolar disorder or any other conditions which affect the way you think, feel or act
- epilepsy or convulsions, fits or seizures (you should avoid taking escitalopram if your epilepsy is not properly controlled; if it is properly controlled your doctor will wish to watch you carefully if you take escitalopram)
- heart problems
- liver problems
- kidney problems
- problems with blood clotting or abnormal bleeding, i.e. a tendency to bleed or bruise easily
- thoughts or actions relating to self-harm or suicide
- diabetes
- a decreased level of sodium in your blood
- restlessness and/or a need to move often (akathisia)
- You are currently pregnant or you plan to become pregnant.
There have been reports that babies exposed to certain antidepressants during the third trimester of pregnancy may develop complications after birth.
Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved. - You are currently breast-feeding or you plan to breast-feed.
It is not recommended that you breast-feed while taking this medicine because escitalopram passes into breast milk and may affect your baby.
Do not take this medicine whilst breast-feeding until you and your doctor have discussed the risks and benefits involved. - You are receiving electroconvulsive therapy (ECT).
- You are planning to have, or have very recently had, surgery or an anaesthetic.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines
This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Some combinations of medicines may increase the risk of serious side effects and are potentially life-threatening.
Therefore some medicines MUST NOT be taken with escitalopram. These include:
- monoamine oxidase inhibitors, such as moclobemide, phenelzine, tranylcypromine, selegiline and linezolid
- pimozide
(see also "When you must not take it").
Some other medicines may interact with escitalopram.
These include:
- tryptophan, contained in some multivitamin and herbal preparations
- sumatriptan, used to treat migraines
- tramadol, a strong pain killer
- sumatriptan and similar medicines used to treat migraines and cluster headaches
- St John's Wort (Hypericum perforatum), a herbal remedy
- other medicines used to treat depression, including SSRIs, imipramine, clomipramine, nortriptyline and desipramine
- lithium, used to treat mood swings and some types of depression
- any other medicines used to treat anxiety, obsessive-compulsive disorder or pre-menstrual dysphoric disorder.
- antipsychotics, medicines used to treat psychoses, schizophrenia and other conditions which affect the way you think, feel or act (e.g. risperidone, thioridazine and haloperidol)
- any other medicines affecting the chemicals in the brain
- prochlorperazine, used to prevent or treat severe nausea and vomiting
- bupropion, a medicine helping to treat nicotine dependence
- mefloquine, an anti-malaria medicine
- some heart or blood pressure medications, e.g. dipyridamole, flecainide, propafenone, metoprolol
- medicines known to prolong bleeding e.g. aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) and anti-coagulants (such as warfarin and ticlopidine), which are used to prevent blood clots
- medicines used to treat reflux and ulcers, such as cimetidine, omeprazole, esomeprazole and lansoprazole
- imipramine and desipramine types of antidepressants.
If you are taking any of these you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with escitalopram.
How to take this medicine
Follow carefully all directions given to you by your doctor.
Their instructions may be different to the information in this leaflet.
How much to take
Your doctor will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
The standard dose for this medicine is 10 mg per day. Your doctor may increase your dose to 20 mg per day depending on how you respond to this medicine.
Elderly people may need smaller doses. The maximum dose for elderly people is 10 mg per day.
Patients with liver disease or with a lack of certain liver enzymes may receive a lower initial dose of 5 mg daily for the first two weeks. Your doctor may increase the dose to 10 mg daily.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
How to take it
Swallow the tablets whole with a full glass of water.
Do not chew them.
When to take it
Take escitalopram as a single dose, either in the morning or in the evening.
Take this medicine at the same time each day.
Taking it at the same time each day will have the best effect and will also help you remember when to take it.
It does not matter if you take it before, with or after food.
How long to take it for
Continue taking your medicine for as long as your doctor tells you, even if it takes some time before you feel any improvement in your condition.
Make sure you have enough to last over weekends and holidays.
As with other medicines for the treatment of these conditions, it may take a few weeks before you feel any improvement.
Individuals will vary greatly in their response to escitalopram.
Your doctor will check your progress at regular intervals.
The length of treatment may vary for each individual, but is usually at least 6 months.
In some cases, your doctor may decide that longer treatment is necessary.
Occasionally the symptoms of depression or other psychiatric conditions may include thoughts of harming yourself or committing suicide. It is possible that these symptoms may continue or increase until the full anti-depressant effect of your medicine becomes apparent.
You or anyone close to you or caring for you should watch for these symptoms and tell your doctor immediately or go to the nearest hospital if you have any distressing thoughts or experiences during this initial period or at any other time.
Also contact your doctor if you experience any worsening of your depression or other symptoms at any time during your treatment.
Stopping Treatment
Do not stop taking this medicine even if you begin to feel better.
Your doctor may decide that you should continue to take it for some time, even when you have overcome your problem. For best effect, this medicine must be taken regularly.
The underlying illness may persist for a long time and if you stop your treatment too soon, your symptoms may return.
Do not stop taking this medicine suddenly.
If you suddenly stop taking your medicine, you may experience mild, but usually temporary, symptoms such as dizziness, pins and needles, electric shock sensations, sleeping problems (vivid dreams, nightmares, inability to sleep), feeling anxious, restless or agitated, headaches, feeling sick (nausea), vomiting, sweating, tremor (shaking), feeling confused, feeling emotional or irritable, diarrhoea, visual disturbances, or fast or irregular heartbeats.
When you have completed your course of treatment, the dose of escitalopram is gradually reduced over a couple of weeks rather than stopped abruptly.
Your doctor will tell you how to reduce the dosage so that you help avoid getting side effects.
If you forget to take it
If you missed a dose and remember in less than 12 hours, take it straight away, and then go back to taking it as you would normally.
Otherwise, if you are more than 12 hours late, skip the dose you missed and take the next dose when you are meant to.
Do not take a double dose to make up for missed doses.
This may increase the chance of you experiencing side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much escitalopram, you may get symptoms of drowsiness, sleepiness, dizziness, high or low blood pressure, nausea (feeling sick), vomiting, agitation or tremor (shaking), fast or slow heart beat or change in heart rhythm, dilated pupils or, rarely, temporary paralysis or weakness of muscles, convulsions or coma.
A condition called serotonin syndrome may occur, with high fever, agitation, confusion, trembling and abrupt contraction of muscles.
While you are taking this medicine
Things you must do
People taking escitalopram may be more likely to think about killing themselves or actually trying to do so, especially when escitalopram is first started or the dose is changed. Tell your doctor immediately if you have thoughts about killing yourself or if you are close to or care for someone using escitalopram who talks about or shows signs of killing him or herself.
All mentions of suicide or violence must be taken seriously.
Occasionally, the symptoms of depression may include thoughts of suicide or self-harm. It is possible that these symptoms continue or get worse until the full antidepressant effect of the medicine becomes apparent. This is more likely to occur if you are a young adult, i.e. 18 to 24 years of age, and you have not used antidepressant medicines before.
If you or someone you know or care for demonstrates any of the following warning signs of suicide-related behaviour while taking escitalopram, contact a doctor immediately, or even to go to the nearest hospital for treatment:
- thoughts or talk of death or suicide
- thoughts or talk of self-harm or harm to others
- any recent attempts of self-harm
- increase in aggressive behaviour, irritability or agitation
- worsening of depression.
Follow your doctor's instructions. Do not stop taking this medicine or change the dose without consulting your doctor, even if you experience increased anxiety at the beginning of treatment.
At the beginning of treatment, some patients may experience increased anxiety, which will disappear during continued treatment.
Tell your doctor immediately if you experience symptoms such as restlessness or difficulty sitting or standing still.
These symptoms can also occur during the first weeks of treatment.
Contact your doctor as soon as possible if you suddenly experience an episode of mania.
Some people with bipolar disorder (manic depression) may enter into a manic phase. Symptoms of mania include lots of rapidly changing thoughts or ideas, exaggerated gaiety, being much more physically active and much more restless.
Sometimes you may not know that you are manic, so it may be helpful to have a friend or relative watch over you for any possible signs of change in your behaviour.
Visit your doctor regularly so they can check on your progress.
Tell your doctor immediately if you become pregnant. If you are a woman of child-bearing age, you should avoid becoming pregnant while taking escitalopram.
Make sure your midwife and/or doctor know you are taking escitalopram. When taken during pregnancy, particularly in the last 3 months of pregnancy, medicines like escitalopram may increase the risk of a serious condition in babies, called persistent pulmonary hypertension of the newborn (PPHN), making the baby breathe faster and appear bluish. These symptoms usually begin during the first 24 hours after the baby is born. If this happens to your baby you should contact your midwife and/or doctor immediately.
Low Sodium
Some people (especially older people or those taking diuretics/water tablets) may experience a lack of sodium in the blood when taking this medicine. Tell your doctor if you get a headache or start to feel sick, restless, irritated, confused or fatigued or if you vomit or have fits, muscle weakness or spasms.
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you are breast-feeding or are planning to breastfeed
- you are about to have any blood tests
- you are going to have surgery or an anaesthetic or are going into hospital.
Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects.
Go to your doctor regularly for a check-up.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed.
Otherwise your doctor may think that it was not effective and change your treatment unnecessarily.
Tell your doctor if you feel this medicine is not helping your condition.
If you are being treated for depression, be sure to discuss with your doctor any problems you may have and how you feel, especially any feelings of severe sadness, thoughts of suicide, bursts of unusual energy, anger or aggression, or if you become particularly agitated or restless.
Tell your doctor immediately if you have any suicidal thoughts or other mental/mood changes.
Make sure you have enough tablets to last over weekends and holidays.
Things you must not do
Do not:
- Give this medicine to anyone else, even if their symptoms seem similar to yours.
- Take your medicine to treat any other condition unless your doctor or pharmacist tells you to.
- Stop taking your medicine, or change the dosage, without first checking with your doctor.
Do not let yourself run out of medicine over the weekend or on holidays.
Suddenly stopping escitalopram may cause unwanted discontinuation symptoms, such as dizziness, headache and nausea. Your doctor will tell you when and how escitalopram should be discontinued. You doctor will gradually reduce the amount you are using, usually over a period of one to two weeks, before stopping completely.
Things to be careful of
Be careful when driving or operating machinery until you know how this medicine affects you.
This medicine may cause nausea, fatigue, drowsiness, sight problems or dizziness in some people, especially early in the treatment. If you have any of these symptoms, do not drive, operate machinery, or do anything else that could be dangerous.
Avoid alcohol while you are taking this medicine.
It is best not to drink alcohol while you are being treated for depression.
You should be aware that people over 50 years of age who take antidepressants have an increased risk of having a bone fracture.
Possible side effects
Tell your doctor as soon as possible if you do not feel well while you are taking escitalopram or if you have any questions or concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects. Sometimes they are serious, but most of the time, they are not.
Tell your doctor if you notice any of the following:
- feeling tired and weak (fatigued), hot flushes, fever, feeling unwell, shaking or tremors, migraine, headache, or giddiness
- muscle, back, bone, nerve or joint pain, stiffness, weakness or cramps, decrease or loss of touch or other senses
- increased or decreased sensitivity to outside stimuli
- feeling or being sick, reflux, diarrhoea or loose bowel motions, constipation, indigestion, stomach pain or discomfort, wind, burping, hiccups, problems swallowing, sore mouth, tongue or throat, haemorrhoids (piles)
- dry mouth, feeling thirsty increased saliva, taste disturbance
- fatigue, sleepiness or drowsiness, yawning, sleeping difficulties, strange or terrifying dreams
- teeth grinding or clenching
- increased or decreased appetite, weight loss
- excessive and/or abnormal movements
- increased muscle tension, muscle twitching
- sexual problems, painful erection, prostate problems
- symptoms of hyperglycaemia (high blood sugar): feeling hungry, thirsty and/or frequent or excessive urination;
- problems with eyes or eyesight
- dizziness when you stand up suddenly, due to low blood pressure
- unable to tolerate alcohol
- menstrual irregularities, period pain, breast pain, unusual vaginal bleeding
- loss of bladder control unusual hair loss or thinning
- tingling or numbness of the hands or feet
- breast enlargement or unusual secretion of breast milk in men or women
- mild rash, or itching or prickling of the skin
- acne, eczema, dermatitis, dry skin, psoriasis or other skin problem
- pain of any type
- ringing or other persistent noise in the ears, problems hearing or earache
- increased or decreased sweating
- bruises
- osteoporosis
- tooth or jaw problems
- flu-like symptoms, runny or blocked nose, sneezing, facial pressure or pain, coughing or sore throat
Tell your doctor as soon as possible if you notice any of the following.
These may be serious side effects. You may need medical attention.
- becoming nervous, confused, forgetful, unable to concentrate, agitated, confused, panicky or anxious
- feeling restless or unable to sit still
- stomach pain with nausea and vomiting of blood, or blood in the bowel movements
- aggression, worsening of depression
- general swelling or swollen hands, ankles, feet or face or eye area due to fluid build-up
- problems speaking
- feelings of not being part of your body, or in a daze
- feeling sick or unwell with weak muscles or feeling confused (these symptoms may be signs of a rare condition as a result of low levels of sodium in the blood, which may be caused by antidepressants and occurs especially in elderly women) increased tendency to bleed, develop bruises or broken bones
- passing more or less urine than normal, or problems when urinating, or bladder infection
- abnormal liver function tests (increased amount of liver enzymes)
- flushing, varicose veins
- infection in any part of your body
- dizziness
- agitation, anxiety, feeling tense and restless, tired, drowsy, lack of energy, irritable, problems sleeping, headache, nausea and tingling or numbness of the hands and feet after stopping escitalopram.
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
These are very serious side effects. You may need urgent medical attention or hospitalisation.
- seizures, tremors, movement disorders (involuntary movements of the muscles or being unco-ordinated).
- coma (unconsciousness)
- a collection of symptoms including weight gain (despite loss of appetite), feeling and being sick, muscle weakness and irritability
- severe rash, with blisters and/ or excessive peeling of skin and also possibly severe blisters and bleeding in the lips, eyes, mouth, nose and genitals
- a sudden increase in body temperature, very high blood pressure, rigid muscles, nausea/vomiting and/or fits (convulsions). These symptoms may be signs of a rare condition called Serotonin Syndrome.
- Neuroleptic Malignant Syndrome (a serious reaction to some medicines with a sudden increase in body temperature, extremely high blood pressure and severe convulsions)
- fast, slow or irregular heartbeat, high blood pressure
- palpitations, fainting or chest pain or tightness
- abnormal bleeding
- kidney pain, difficulty in passing urine, dark coloured urine or blood in the urine
- a collection of symptoms including fever, sore throat, swollen glands, mouth ulcers, unusual bleeding or bruising under the skin
- mania (mood of excitement, over-activity and uninhibited behaviour or aggression), hallucinations (hearing, seeing or feeling things that are not there)
- jaundice (yellowing of the skin and/or eyes), with or without other signs of hepatitis or liver problems (loss of appetite, tiredness, feeling or being sick, dark urine, stomach pain or swelling, confusion, unconsciousness).
- feeling paranoid, panicky, or "high" or having mood swings or feeling more depressed or in a trance
- thoughts of suicide or attempting suicide or self-harm
- sudden, severe breathing problems
- sudden weakness or numbness of the face, arms or legs, especially on one side, slurred speech
Other side effects not listed above may also occur in some people.
Allergic reactions
If you think you are having an allergic reaction to escitalopram, do not take any more of this medicine and tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
- fainting
- hayfever-like symptoms
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it.
If you take your medicine out of its original packaging, it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 30°C.
Do not store your medicine, or any other medicine, in the bathroom, or near a sink.
Do not leave it on a window-sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine, or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
What Chemmart Escitalopram looks like
Chemmart Escitalopram tablets are available in the following strengths:
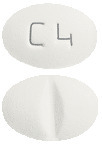
- 10 mg tablets: white to off - white, oval, biconvex, film-coated tablets with "C4" embossed on one side and a notch break-line on the other side.
- 20 mg tablets: white to off - white, oval, biconvex, film-coated tablets with "C3" embossed on one side and a notch break-line on the other side.
Blister packs of 28 tablets.
* Not all strengths may be available.
Ingredients
Each tablet contains 10 mg, or 20 mg of escitalopram (as oxalate) as the active ingredient.
It also contains the following inactive ingredients:
- microcrystalline cellulose
- colloidal anhydrous silica
- hypromellose
- magnesium stearate
- croscarmellose sodium
- purified talc
- macrogol 400
- titanium dioxide.
This medicine is gluten-free, lactose free, sucrose-free, tartrazine-free and free of other azo dyes.
Australian Registration Numbers
Chemmart Escitalopram 10 mg tablets (blister pack): AUST R 213723.
Chemmart Escitalopram 20 mg tablets (blister pack): AUST R 213724.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
This leaflet was last updated in:
January 2017.



 Furthermore, escitalopram 20 mg/day was significantly more efficacious than placebo on the Y-BOCS subscale of rituals at week 12. Both escitalopram 10 mg/day and escitalopram 20 mg/day were significantly more efficacious than placebo on the Y-BOCS subscale of obsessions as well as on the NIMH-OCS total score, CGI-I score and CGI-S score.
Furthermore, escitalopram 20 mg/day was significantly more efficacious than placebo on the Y-BOCS subscale of rituals at week 12. Both escitalopram 10 mg/day and escitalopram 20 mg/day were significantly more efficacious than placebo on the Y-BOCS subscale of obsessions as well as on the NIMH-OCS total score, CGI-I score and CGI-S score. Results after 24 weeks showed that both escitalopram 10 mg/day (p < 0.05) and escitalopram 20 mg/day (p < 0.01) were significantly more efficacious than placebo as measured by the primary outcome measure, the Y-BOCS total score, as well as on the secondary subscales of Y-BOCS (obsessions and rituals) and the NIMH-OCS score (escitalopram 10 mg/day (p < 0.01) and escitalopram 20 mg/day (p < 0.001)). See Table 3.
Results after 24 weeks showed that both escitalopram 10 mg/day (p < 0.05) and escitalopram 20 mg/day (p < 0.01) were significantly more efficacious than placebo as measured by the primary outcome measure, the Y-BOCS total score, as well as on the secondary subscales of Y-BOCS (obsessions and rituals) and the NIMH-OCS score (escitalopram 10 mg/day (p < 0.01) and escitalopram 20 mg/day (p < 0.001)). See Table 3. The beneficial efficacy of long-term treatment with escitalopram was also demonstrated by the analyses of responders and remitters in this study as shown in Tables 4 and 5.
The beneficial efficacy of long-term treatment with escitalopram was also demonstrated by the analyses of responders and remitters in this study as shown in Tables 4 and 5.
 Maintenance of efficacy and prevention of relapse were investigated in the relapse prevention study. This 24 week relapse prevention study was preceded by a 16 week open label period with patients initially receiving escitalopram 10 mg/day. In case of lack of efficacy (as judged by the investigator), the dose could be increased to a maximum of 20 mg/day. If dose limiting adverse effects occurred, it was permissible to decrease the dose to 10 mg/day. Thus the dose of escitalopram was flexible at 10-20 mg/day from week 2 to 12. Subsequently, the dose was fixed at the dose received at the end of week 12 until week 16 to allow stabilisation of the patient on this dose. Responders to treatment were defined as patients with a decrease in Y-BOCS total score from baseline by ≥ 25% at week 16 and remitters were defined as Y-BOCS ≤ 10. See Table 6 for responder and remitter rates at the end of the 16 week open label phase.
Maintenance of efficacy and prevention of relapse were investigated in the relapse prevention study. This 24 week relapse prevention study was preceded by a 16 week open label period with patients initially receiving escitalopram 10 mg/day. In case of lack of efficacy (as judged by the investigator), the dose could be increased to a maximum of 20 mg/day. If dose limiting adverse effects occurred, it was permissible to decrease the dose to 10 mg/day. Thus the dose of escitalopram was flexible at 10-20 mg/day from week 2 to 12. Subsequently, the dose was fixed at the dose received at the end of week 12 until week 16 to allow stabilisation of the patient on this dose. Responders to treatment were defined as patients with a decrease in Y-BOCS total score from baseline by ≥ 25% at week 16 and remitters were defined as Y-BOCS ≤ 10. See Table 6 for responder and remitter rates at the end of the 16 week open label phase. Responders at the end of the above 16 week open label treatment phase (escitalopram 10 mg: 30 responders; escitalopram 20 mg: 133 responders) entered the 24 week randomised, double blind placebo controlled relapse prevention phase. Both escitalopram 10 mg/day (p = 0.014) and 20 mg/day (p < 0.001) showed significantly fewer relapses as seen in Table 7.
Responders at the end of the above 16 week open label treatment phase (escitalopram 10 mg: 30 responders; escitalopram 20 mg: 133 responders) entered the 24 week randomised, double blind placebo controlled relapse prevention phase. Both escitalopram 10 mg/day (p = 0.014) and 20 mg/day (p < 0.001) showed significantly fewer relapses as seen in Table 7.

