What is in this leaflet
This leaflet answers some common questions about COZAVAN.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking COZAVAN against the benefits expected for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What COZAVAN is used for
COZAVAN belongs to a group of medicines, called angiotensin II receptor antagonists. It works to lower high blood pressure (which doctors call hypertension) by relaxing your blood vessels. In addition, COZAVAN slows the progression of kidney disease in people who have type 2 diabetes mellitus (also known as non-insulin dependent diabetes) with protein in their urine (which doctors call proteinuria).
Hypertension:
Everyone has blood pressure. This pressure helps get your blood all around your body. Your blood pressure may be different at various times of the day, depending on how busy or worried you are.
You have hypertension (high blood pressure) when your blood pressure stays high, even when you are calm and relaxed.
There are usually no symptoms of hypertension. The only way of knowing that you have hypertension is to have your blood pressure checked on a regular basis. If high blood pressure is not treated it can lead to serious health problems. You may feel fine and have no symptoms, but eventually hypertension can cause stroke, heart disease or kidney failure. COZAVAN helps to lower your blood pressure.
Type 2 Diabetes Mellitus:
Type 2 diabetes mellitus is a condition in which the body's cells do not respond to the effects of insulin or too little insulin is produced, resulting in an elevated blood (sugar) level, known as hyperglycaemia.
Insulin maintains the appropriate level of glucose in the blood by transporting it into the body's cells so that they can produce energy or store glucose until it's needed.
Hyperglycaemia can lead to serious problems with your heart, eyes, circulation or kidneys. When kidney damage occurs, its ability to filter blood is reduced, and proteins in the blood are lost in the urine. This may eventually lead to kidney failure. In people who have type 2 diabetes mellitus with protein in their urine, COZAVAN helps to slow the worsening of kidney disease and reduce the need for dialysis or kidney transplantation.
COZAVAN is not addictive.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may prescribe COZAVAN on its own, or in addition to another medicine for controlling your seizures or migraines.
Your doctor may have prescribed COZAVAN for another reason.
Before you take COZAVAN
When you must not take it
Do not take COZAVAN if you are pregnant or breast-feeding. The use of COZAVAN while you are pregnant or breast-feeding is not recommended. Your baby may absorb this medicine in the womb. COZAVAN can cause harm or death to an unborn baby. Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant. If you get pregnant while taking COZAVAN tell your doctor right away.
It is not known whether COZAVAN passes onto breast milk, therefore it is not recommended that COZAVAN be taken while you are breast-feeding.
Do not take COZAVAN if you have diabetes and are taking a medicine called aliskiren to reduce blood pressure.
Do not take COZAVAN if you are allergic to:
- medicines containing losartan potassium
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include skin rash, itching or hives; swelling of the face, lips or tongue, which may cause difficulty in swallowing or breathing; wheezing or shortness of breath.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or show signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Do not give COZAVAN to a child. There is no experience with the use of COZAVAN in children.
Before you start to take it
Tell your doctor if you are pregnant or plan to become pregnant.
Tell your doctor if you are breast-feeding or plan to breast-feed. COZAVAN should not be used during pregnancy or while breast-feeding.
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you are taking other medicines that may increase serum potassium (see Taking other medicines).
Tell your doctor if you have, or have had, any medical conditions, especially the following:
- kidney disease
- liver problems
Your doctor may want to take special care if you have any of these conditions.
Tell your doctor if you have recently had excessive vomiting or diarrhoea.
If you have not told your doctor about any of the above, tell him/her before you start taking COZAVAN.
Your doctor will advise you whether or not to take COZAVAN or if you need to adjust the dose or adapt your treatment.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by COZAVAN or may affect how well COZAVAN works. These include:
- other blood pressure medicines
- diuretic tablets, also called fluid or water tablets, including potassium-sparing diuretics
- potassium tablets
- potassium-containing salt substitutes
- other medicines that may increase serum potassium (e.g., trimethoprim-containing products)
- lithium, a medicine used to treat mood swings and some types of depression
- medicines used to relieve pain, swelling, and other symptoms of inflammation, for example, indometacin
- grapefruit juice (which should be avoided while taking COZAVAN)
These medicines may have an additive effect with COZAVAN in either lowering your blood pressure, affecting how well it works, or leading to increases in potassium in your blood. You may need to take different amounts of your medicine, or you may need to take different medicines.
Your doctor can tell you what to do if you are taking any of these medicines.
If you are not sure whether you are taking any of these medicines, check with your doctor or pharmacist.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking COZAVAN.
How to take COZAVAN
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the pack, ask your doctor or pharmacist.
How to take it
Always swallow the film-coated tablets whole with plenty of water. You can take the film-coated tablets with or without food.
How much to take
Your doctor will tell you how many tablets you need to take each day. This depends on your condition and whether you are taking other medicines. Take COZAVAN only when prescribed to you by your doctor.
For high blood pressure:
For most patients, the usual starting dose is one 50 mg film-coated tablet taken once a day. Some patients may need a lower starting dose. The dose may need to be increased depending on your blood pressure. Most patients take between 25 to 100 mg each day, taken as a single dose or in divided doses.
For type 2 diabetes mellitus with protein in the urine:
The usual starting dose is one 50 mg film-coated tablet taken once a day. The dose may be increased to 100 mg once a day depending on your blood pressure.
When to take it
Take your COZAVAN at about the same time each day. Taking your film-coated tablet(s) at about the same time each day will have the best effect. It will also help you remember when to take the film-coated tablets.
Swallow COZAVAN with a glass of water.
It does not matter whether you take COZAVAN before or after food.
How long to take it for
Keep taking COZAVAN for as long as your doctor tells you to.
COZAVAN helps you control your high blood pressure but does not cure it, so it is important to take it every day.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your film-coated tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you miss more than one dose, or are not sure what to do, check with your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist or doctor for some hints.
If you take too much (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at the nearest hospital, if you think you or anyone else may have taken too much COZAVAN. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much COZAVAN, you may experience dizziness or light-headedness.
While you are taking COZAVAN
Things you must do
If you become pregnant while taking COZAVAN, tell your doctor immediately. Your doctor needs to know immediately so that COZAVAN can be replaced by another medicine.
Have your blood pressure checked when your doctor says, to make sure COZAVAN is working.
Before starting any new medicine, tell your doctor or pharmacist that you are taking COZAVAN.
If you feel light-headed, dizzy or faint, get up slowly when getting out of bed or standing up. You may feel light-headed or dizzy while taking COZAVAN, especially if you are also taking a diuretic (fluid tablet). This may become worse if you stand up quickly as your blood pressure may fall. Standing up slowly, especially when you get up from bed or a chair, will help your body get used to the change in position and blood pressure. This problem is not common. If it occurs and gets worse or continues, talk to your doctor.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking COZAVAN.
If you plan to have surgery (that requires an anaesthetic), including dental surgery, tell your doctor or dentist that you are taking COZAVAN.
Make sure you drink plenty of water during exercise and hot weather when you are taking COZAVAN, especially if you sweat a lot. If you do not drink enough water while taking COZAVAN, you may faint or feel light-headed or sick. This is because your body doesn't have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
If you have excessive vomiting and/or diarrhoea while taking COZAVAN, tell your doctor. This can also mean that you are losing too much water and your blood pressure may become too low.
If your doctor has prescribed potassium tablets for you, continue taking them. COZAVAN contains a very small amount of potassium, but this does not replace any potassium tablets that you may be taking.
Tell your doctor if, for any reason, you have not taken COZAVAN exactly as prescribed. Otherwise, your doctor may adjust your treatment unnecessarily.
Visit your doctor regularly so that they can check your progress. Your doctor may ask you to have regular blood tests to check the potassium level in your blood, and see how your kidneys are working.
Things you must not do
Do not drive or operate machinery until you know how COZAVAN affects you. COZAVAN may cause drowsiness, dizziness or affect alertness in some people. These effects may continue the following day.
Therefore, make sure you know how COZAVAN affects you before you drive a car, operate machinery or do anything else that could be dangerous. If you drink alcohol, dizziness or light-headedness may be worse.
Do not take COZAVAN for a longer time than your doctor has prescribed.
Do not let yourself run out of COZAVAN over the weekend or on holidays.
Do not use COZAVAN to treat any other conditions unless your doctor tells you to.
Do not give COZAVAN to anyone else, even if they have the same condition as you.
Things to be careful of
Effects on driving and operating machinery.
COZAVAN may cause drowsiness, dizziness or other symptoms which could affect your ability to drive or operate machinery. Make sure you know how you are affected by this medicine before you drive a car or use machinery, or do anything else that could be dangerous if you are dizzy or light-headed. If you drink alcohol, dizziness or lightheadedness may be worse.
Particular care is recommended when you are first taking COZAVAN or if the amount of COZAVAN or any other medicine you are taking is increased or decreased.
Be careful if you are elderly, unwell or taking other medicines. Some people may experience side effects such as drowsiness, confusion, dizziness and unsteadiness, which may increase the risk of a fall.
Lifestyle measures that help reduce heart disease risk
By following these simple measures, you can further reduce the risk from heart disease.
- Quit smoking and avoid second-hand smoke.
- Limit alcohol intake.
- Enjoy a healthy diet by:
- eating plenty of fresh vegetables, fruit, bread, cereals and fish.
- eat less sugar
- your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake you should avoid using salt in cooking or at the table.
- reducing your saturated fat intake (eat less fatty meats, full fat dairy products, butter, coconut and palm oils, most take-away foods, commercially-baked products). - Be active, regular exercise helps to reduce blood pressure and helps the heart get fitter, but it is important not to overdo it. Progress, over time, to at least 30 minutes of moderate-intensity physical activity on 5 or more days each week. Can be accumulated in shorter bouts of 10 minutes duration. If you have been prescribed anti-angina medicine, carry it with you when being physically active. Before starting any exercise, ask your doctor about the best kind of programme for you.
- Maintain a healthy weight. Your doctor may suggest losing some weight to help lower your blood pressure and help lessen the amount of work your heart has to do. Some people may need a dietician's help to lose weight.
- Discuss your lifestyle and lifestyle plans with your doctor.
- For more information and tools to improve your heart health, call Heartline, the Heart Foundation's national telephone information service, on 1300 36 27 87 (local call cost).
Know warning signs of heart attack and what to do:
- Tightness, fullness, pressure, squeezing, heaviness or pain in your chest, neck, jaw, throat, shoulders, arms or back.
- You may also have difficulty breathing, or have a cold sweat or feel dizzy or light headed or feel like vomiting (or actually vomit).
- If you have heart attack warning signs that are severe, get worse or last for 10 minutes even if they are mild, call triple zero (000). Every minute counts.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking COZAVAN.
COZAVAN helps most people with high blood pressure, but it may have unwanted side effects in some people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- dizziness
- lightheadedness
- tiredness or weakness
- spinning sensation
- generally feeling unwell
- increased sensitivity of the skin to sun
- inability to get or maintain an erection
These are the common side effects of COZAVAN. For the most part these have been mild.
Also, tell you doctor if you develop cough.
Tell your doctor as soon as possible if you have any of the following as you may need medical attention:
- skin rash, itchiness
- signs of anaemia, such as tiredness, shortness of breath, and looking pale
- aching muscles, not caused by exercise
- bleeding or bruising more easily than normal
The above list includes serious side effects that may require medical attention. Skin rash and itchiness may be symptoms of an allergic reaction. Serious side effects are rare.
If any of the following happen, stop taking COZAVAN and tell your doctor immediately or go to Accident and Emergency at the nearest hospital:
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- severe and sudden onset of pinkish, itchy swellings on the skin, also called hives or nettlerash
The above list includes very serious side effects. If you have them, you may have had a serious allergic reaction to COZAVAN. You may require urgent medical attention or hospitalisation. These side effects are rare.
Tell your doctor if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people. Tell your doctor if you notice any other effects.
After taking COZAVAN
Storage
Keep COZAVAN where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your film-coated tablets in the original pack until it is time to take them. If you take the film-coated tablets out of the pack they will not keep well.
Keep your film-coated tablets in a cool dry place where the temperature stays below 25°C.
Do not store COZAVAN or any other medicine in the bathroom or near a sink.
Do not leave COZAVAN in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking COZAVAN, or your film-coated tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
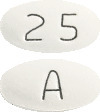
COZAVAN is available in 2 tablet strengths:
- 25 mg film-coated tablets are white to off white, oval shaped biconvex film-coated tablet with "A" engraved on one side and "25" on the other side
- 50 mg film-coated tablets are white to off white, oval shaped biconvex film-coated tablet with "A50"engraved on one side and has a central break line on the other side
Each blister pack of 25 mg contains either 10 (as starter pack) or 30 film-coated tablets.
Each blister pack of 50 mg contains either 10 (as starter pack) or 30 film-coated tablets.
Ingredients
The active ingredient in COZAVAN is losartan potassium.
- Each COZAVAN 25 film-coated tablet contains 25 mg of losartan potassium.
- Each COZAVAN 50 film-coated tablet contains 50 mg of losartan potassium.
The film-coated tablets also contain the following inactive ingredients:
- microcrystalline cellulose
- lactose monohydrate
- pregelatinised maize starch
- magnesium stearate
- Opadry complete film coating system 20A58900 White ARTG PI No: 13043)
COZAVAN film-coated tablet contains lactose.
COZAVAN film-coated tablets do not contain gluten, sucrose, tartrazine or any other azo dyes.
Supplier
COZAVAN is supplied by:
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
Phone: 1800 274 276
www.viatris.com.au
This leaflet was prepared in May 2023.
Australian registration numbers:
COZAVAN 25 mg -
AUST R 156235
COZAVAN 50 mg -
AUST R 156234
COZAVAN is a Viatris company trade mark
COZAVAN_cmi\May23/00
Published by MIMS July 2023


 The following adverse events were also reported at a rate of 1% or greater in patients treated with losartan, but were as, or more frequent, in the placebo group: asthenia/ fatigue, oedema/ swelling, abdominal pain, chest pain, nausea, headache, pharyngitis.
The following adverse events were also reported at a rate of 1% or greater in patients treated with losartan, but were as, or more frequent, in the placebo group: asthenia/ fatigue, oedema/ swelling, abdominal pain, chest pain, nausea, headache, pharyngitis. The difference in the incidence of stroke in patients treated with losartan potassium and atenolol amounts to 1 additional stroke prevented for every 53 patients treated with losartan potassium for 5 years. The reduction in the incidence of stroke does not replace the need to adequately titrate patients to adequate blood pressure control.
The difference in the incidence of stroke in patients treated with losartan potassium and atenolol amounts to 1 additional stroke prevented for every 53 patients treated with losartan potassium for 5 years. The reduction in the incidence of stroke does not replace the need to adequately titrate patients to adequate blood pressure control.
 There was no significant difference observed in the rate of death among patients treated with losartan potassium (21%) compared to those on placebo (20.3%). There was no significant difference observed in the incidence of cardiovascular mortality and morbidity between patients treated with losartan potassium and those who received placebo (p = 0.253).
There was no significant difference observed in the rate of death among patients treated with losartan potassium (21%) compared to those on placebo (20.3%). There was no significant difference observed in the incidence of cardiovascular mortality and morbidity between patients treated with losartan potassium and those who received placebo (p = 0.253). Molecular formula: C22H22ClKN6O.
Molecular formula: C22H22ClKN6O.