What is in this leaflet
This leaflet answers some common questions about DETRUSITOL. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking DETRUSITOL against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Read this leaflet carefully before you start DETRUSITOL.
Keep this leaflet with the medicine. You may need to read it again.
What DETRUSITOL is used for
DETRUSITOL is used to treat symptoms of an overactive bladder, for example urinary frequency, urgency or incontinence.
DETRUSITOL belongs to a group of medicines called antispasmodics. It helps to control the release of urine by reducing spasm, and relaxing the smooth muscle of the bladder wall. It also increases the storage volume of the bladder, and can act on the brain to delay the desire to urinate.
Ask your doctor if you have any questions about why DETRUSITOL has been prescribed for you.
This medicine is not addictive.
This medicine is available only with a doctor's prescription.
Before you take DETRUSITOL
When you must not take it
Do not take DETRUSITOL if:
- you have an allergy to
- tolterodine
- any of the ingredients listed at the end of this leaflet
- any other similar medicines
Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; rash, itching or hives on the skin.
- you are unable to pass urine
- you have a blocked gastro-intestinal tract or other gastro-intestinal disorders (ulcerative colitis, toxic megacolon)
- you have uncontrolled high pressure in the eye (narrow angle glaucoma)
- you have a disease of the muscles causing drooping eyelids, double vision, difficulty in speaking and swallowing and sometimes muscle weakness in the arms or legs (myasthenia gravis)
- you are breast feeding
Do not give DETRUSITOL to children. Safety and effectiveness of DETRUSITOL in children have not been established.
Do not take DETRUSITOL after the expiry date (EXP) printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking DETRUSITOL, talk to your doctor.
Before you start taking it
Tell your doctor if:
- you have allergies to any other medicines, foods, preservatives or dyes
- you have or have had any of the following medical conditions:
- kidney or liver problems
- heart problems
- problems with urine retention
- intestinal blockage or other intestinal or stomach problems
- autonomic neuropathy (a nerve problem which sometimes occurs with diabetes and can lead to diarrhoea, impotence or low blood pressure)
- hiatus hernia (a part of the stomach protrudes through the diaphragm, causing belching and heart burn)
- severe constipation
- raised pressure in the eye(s)
- you are pregnant or intend to become pregnant.
Your doctor will discuss the risks and benefits of taking DETRUSITOL during pregnancy.
If you have not told your doctor or pharmacist about any of the above, tell them before you start to take DETRUSITOL.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines and DETRUSITOL may interfere with each other. These include:
- some medicines used to treat depression such as: fluoxetine, amitriptyline
- certain medicines used to treat irregular heart beats: flecainide, quinidine, procainamide, disopyramide, sotalol, amiodarone
- some antifungals: fluconazole, ketoconazole, itraconazole, miconazole
- some antibiotics: erythromycin, clarithromycin
- cisapride, a medicine used to treat heartburn/reflux and related intestinal disorders
- metoclopramide, a medicine used to treat nausea and gastric retention
- tranquillisers, such as: haloperidol, chlorpromazine, thioridazine, pimozide
- anti-proteases, medicines used to treat HIV infection, such as: ritonavir, indinavir
- droperidol, a medicine used to prevent or reduce nausea and vomiting
These medicines may be affected by DETRUSITOL or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking DETRUSITOL.
How to take DETRUSITOL
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
The usual dose is 1mg or 2mg twice daily. Your doctor will prescribe the dose that is right for you.
How to take it
Swallow the tablets whole with a full glass of water.
When to take it
Take your medicine at about the same time each day. Taking DETRUSITOL at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take DETRUSITOL before or after food.
How long to take it
Continue taking your medicine for as long as your doctor tells you. This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
Your doctor should re-assess your condition at regular intervals, for example after 6 months, to determine how long you need to keep taking DETRUSITOL for.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not try to make up for missed doses by taking more than one dose at a time. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poison Information Centre - the telephone number in Australia is 131 126 and in New Zealand is 0800 POISON or 0800 764 766 - or go to the Accident and Emergency (Casualty) Department at your nearest hospital if you think you or anyone else may have taken too much DETRUSITOL. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
The symptoms of taking too much DETRUSITOL may include shortness of breath, fits, fast heart beat, inability to pass urine, dilated pupils, feeling excited or hallucinations.
While you are using DETRUSITOL
Things you must do
If symptoms of your overactive bladder do not improve, or if they become worse, tell your doctor.
If you are about to start taking any new medicine, remind your doctor and pharmacist that you are taking DETRUSITOL.
If you become pregnant while taking DETRUSITOL, tell your doctor.
Tell all doctors, dentists, and pharmacists who treat you that you are taking DETRUSITOL.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking DETRUSITOL. It may affect other medicines used during surgery.
Always discuss with your doctor any problems or difficulties during or after taking DETRUSITOL.
Things you must not do
Do not take DETRUSITOL to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you or their symptoms seem similar to yours.
Do not stop taking your medicine or lower the dosage unless your doctor tells you to, even if you are feeling better.
Things to be careful of
Be careful driving or operating machinery until you know how DETRUSITOL affects you. This medicine may cause dizziness and blurred vision in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Be careful when drinking alcohol while you are taking this medicine. If you drink alcohol, dizziness may be worse.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking DETRUSITOL.
This medicine helps most people with an overactive bladder, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- Dry mouth
- Heartburn
- Headache
- Constipation, stomach pain or diarrhoea
- Dry eyes
- Nausea
- Tiredness
- Swollen ankles
Tell your doctor immediately if you notice any of the following:
- Swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- Dizziness or confusion
- Fits
- Fast heartbeat or palpitations
- Shortness of breath and swelling of the feet or legs
- Blurred vision
- Difficulty or pain in urinating (passing water)
- Hallucinations (seeing, hearing or feeling things that are not really there)
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After using DETRUSITOL
Storage
Keep your tablets in the blister until it is time to take them. If you take the tablets out of the blister they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 25 degrees Celsius.
Do not store DETRUSITOL or any other medicine in the bathroom or near a sink. Do not leave it on a windowsill or in the car. Heat and dampness can destroy some medicines.
Keep DETRUSITOL where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking DETRUSITOL or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
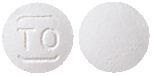
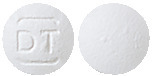
What it looks like
There are two strengths of tablets available, 1mg and 2mg. The 1mg tablet is a white round, biconvex, film-coated tablet, engraved with arcs above and below the letters 'TO'. The 2mg tablet is a white round, biconvex, film-coated tablet, engraved with arcs above and below the letters 'DT'.
DETRUSITOL tablets are available in blister packs containing 56 tablets.
Ingredients
Active Ingredients
DETRUSITOL contains either 1mg or 2mg of tolterodine tartrate as the active ingredient.
Inactive Ingredients
The other ingredients in the two strengths are:
- calcium hydrogen phosphate
- microcrystalline cellulose
- sodium starch glycollate
- silica colloidal anhydrous
- magnesium stearate
- hypromellose
- stearic acid
- titanium dioxide
Supplier
DETRUSITOL is supplied in Australia by:
Viatris Pty Ltd
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
DETRUSITOL is supplied in New Zealand by:
Viatris Ltd
PO Box 11-183
Ellerslie
AUCKLAND
www.viatris.co.nz
Telephone 0800 168 169
Australian Registration Numbers
DETRUSITOL 1 mg AUST R 99393
DETRUSITOL 2 mg AUST R 99394
This leaflet was prepared in August 2021.
DETRUSITOL® is a Viatris company trade mark
ujcdetrt10821
Published by MIMS December 2021


 In the three active comparator studies, Detrusitol and oxybutynin were equivalent in the reduction of mean number of micturitions per 24 hours and mean number of incontinence episodes per 24 hours. Significant improvement was seen after 2 weeks of treatment with Detrusitol, with further improvement up to 8 weeks of treatment; this therapeutic effect was sustained for up to 12 months of treatment.
In the three active comparator studies, Detrusitol and oxybutynin were equivalent in the reduction of mean number of micturitions per 24 hours and mean number of incontinence episodes per 24 hours. Significant improvement was seen after 2 weeks of treatment with Detrusitol, with further improvement up to 8 weeks of treatment; this therapeutic effect was sustained for up to 12 months of treatment.

