What is Diflucan One used for?
Diflucan One is used to treat vaginal thrush.
If this is the first time you have had these symptoms, talk to your doctor before using any treatment.
Vaginal thrush
Most women experience vaginal thrush at some point during their lives. Thrush is the common name given to a vaginal yeast infection. Vaginal yeast infections are caused by Candida, a type of yeast. Many women have this yeast living harmlessly within their bodies. However, some factors can cause an upset in the natural balance inside the vagina and an overgrowth of yeast can occur. These factors may include use of antibiotics, hormonal changes (during pregnancy, menstruation, menopause), diabetes, the contraceptive pill, wearing tight clothing, or using perfumed soaps, bath additives and vaginal deodorants. When the levels of yeast become too high, thrush develops.
Common thrush symptoms
You may experience one or more of these common symptoms:
- Vaginal itching
- Vaginal burning and redness
- Pain during intercourse
- A thick, white, cottage cheese-like discharge, usually odourless
Rubbing and scratching can aggravate the soreness and itching. Also, the salt in urine can sting the sore tissue.
Before using Diflucan One
Do not use Diflucan One:
- If you are pregnant, suspect you might be pregnant, are trying to become pregnant or are breastfeeding.
- If you are hypersensitive to any of the DIFLUCAN® One ingredients or any other thrush treatment.
- If you are taking cisapride (a medicine to treat stomach problems).
Do not use Diflucan One unless you have spoken to your doctor:
- If you are taking any medicine. Some medicines and Diflucan One may interfere with each other. These include phenytoin (for epilepsy), warfarin (to prevent blood clots) and oral hypoglycaemics (for diabetes). Tell your doctor or pharmacist before using Diflucan One if you are taking warfarin, as bleeding or bruising may occur.
- If you are unsure about the cause of your symptoms.
- If you have had thrush more than twice in the last six months.
- If you are diabetic.
- If you have any disease or illness affecting your liver or kidneys or have had unexplained jaundice.
- If you have had heart problems.
- If you or your partner have had exposure to a sexually transmitted disease.
- If you have any abnormal or irregular vaginal bleeding or a blood stained discharge.
- If you have vulval or vaginal sores, ulcers or blisters.
- If you are experiencing lower abdominal pain or burning on passing urine.
How to use Diflucan One
The complete Diflucan One course of treatment for thrush is one capsule, once.
Take by mouth with a drink of water at any time of day, with or without food.
You should notice an improvement in your symptoms in a day or two. Consult your doctor if you are no better in three days or if the thrush returns.
Diflucan One is not recommended for children.
What side effects may I experience after taking Diflucan One?
Taking this medicine may cause mild side effects such as nausea or feeling sick, headache, stomach pain, indigestion or diarrhoea.
Consult your doctor if you notice anything that is making you feel unwell.
A few people develop allergic reactions to medicines. If you experience difficulty with breathing, facial swelling or severe itchiness or skin rashes, consult your doctor immediately.
Be careful when driving vehicles or operating machinery as occasional dizziness or seizures may occur
How to avoid thrush in future
- Wear cotton briefs, stockings and loose-fitting clothes rather than tight synthetic clothing.
- Wash regularly but do not wash and dry yourself too harshly.
- Avoid perfumed soaps, bath additives and vaginal deodorants.
What is in Diflucan One?
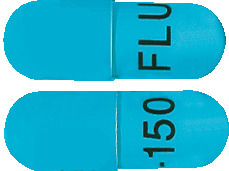
The Diflucan One pack contains one capsule. Each light turquoise blue capsule contains 150 mg fluconazole.
Other ingredients are colloidal anhydrous silica, magnesium stearate, maize starch, lactose, sodium lauryl sulfate, the colours patent blue V, TekPrint SW-9008 black ink and titanium dioxide and a gelatin capsule shell.
Fluconazole is an antifungal agent which fights the cause of infections such as thrush.
Diflucan One 150 mg: AUST R 100956.
Who supplies Diflucan One?
Diflucan One is supplied in Australia by:
Johnson & Johnson Pacific
AUSTRALIA • NEW ZEALAND
45 Jones Street, Ultimo NSW 2007, AUSTRALIA and Auckland, NEW ZEALAND
® Registered Trademark Pfizer Products Inc.
Storing Diflucan One
KEEP OUT OF REACH OF CHILDREN.
Do not use after the date stamped on the pack.
Store below 30°C. Keep dry. Protect from light.
Date of Preparation: September 2017
Published by MIMS January 2019