What is in this leaflet
This leaflet answers some common questions about DOVATO. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking DOVATO against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What DOVATO is used for
DOVATO is used to treat HIV (human immunodeficiency virus) infection in adults and in children over the age of 12 years.
DOVATO contains two active ingredients that are used to treat HIV infection: dolutegravir and lamivudine. Dolutegravir belongs to a group of anti-retroviral medicines called integrase inhibitors (INIs). Lamivudine belongs to a group of anti-retroviral medicines called nucleoside analogue reverse transcriptase inhibitors (NRTIs).
DOVATO does not cure HIV infection, it reduces the amount of virus in your body and keeps it at a low level. DOVATO also increases the CD4 cell count in your blood. CD4+ cells are a type of white blood cell that are important in helping your body to fight infection.
Not everyone responds to treatment with DOVATO in the same way. Your doctor will monitor the effectiveness of your treatment.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
DOVATO is not addictive.
DOVATO is not recommended for children under the age of 12 years as the dosage cannot be modified.
DOVATO is only available with a doctor's prescription.
DOVATO is not expected to affect your ability to drive a car or operate machinery.
Before you take DOVATO
When you must not take it
Do not take DOVATO if:
- you have ever had an allergic reaction to any medicine containing dolutegravir or lamivudine.
- you are allergic to any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin - if you're taking another medicine called dofetilide or pilsicainide (to treat heart conditions) or fampridine (to treat multiple sclerosis).
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- liver disease, including hepatitis B or C
- kidney disease
Tell your doctor if you are pregnant, think you could be pregnant or plan to become pregnant.
Your doctor will consider the benefit to you and the risk to your baby of taking DOVATO while you're pregnant
If you could get pregnant while receiving DOVATO, you need to use a reliable method of contraception, to prevent pregnancy.
Taking dolutegravir (one of the components of DOVATO) at the time of becoming pregnant, or during the first twelve weeks of pregnancy, may increase the risk of a type of birth defect, called neural tube defect, such as spina bifida (malformed spinal cord).
In babies and infants exposed to NRTIs during pregnancy or labour, small temporary increases in blood levels of a substance called lactate have been observed. Additionally, there have been very rare reports of diseases that affect the nervous system such as a delayed development and seizures.
Your doctor can discuss with you the risks and benefits involved.
Where possible, women who are HIV-positive should not breast-feed because HIV infection can be passed on to the baby in breast milk
If formula feeding is not possible, you should get advice from your doctor.
A small amount of the ingredients in DOVATO can also pass into your breast-milk.
If you have not told your doctor about any of the above, tell him/ her before you start taking DOVATO.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Do not take DOVATO with these medicines:
- dofetilide or pilsicainide which is used to treat heart conditions
- fampridine which is used to treat multiple sclerosis
These medicines should not be used with DOVATO:
- emtricitabine, to treat HIV infection
- sorbitol-containing medicines (usually liquids) used regularly
Tell your doctor if you're being treated with any of these.
Tell your doctor if you are taking:
- metformin, to treat diabetes
- medicines called antacids, to treat indigestion and heartburn. Do not take an antacid during the 6 hours before you take DOVATO, or for at least 2 hours after you take it.
- Calcium, magnesium and iron supplements. Do not take a calcium, magnesium or iron supplement during the 6 hours before you take DOVATO, or for at least 2 hours after you take it. If you take food with your medicine you can take a calcium, magnesium or iron supplement at the same time as DOVATO.
- etravirine, efavirenz, nevirapine or tipranavir/ritonavir, to treat HIV infection
- rifampicin, to treat tuberculosis (TB) and other bacterial infections
- co-trimoxazole, an antibiotic used to treat Pneumocystis jiroveci pneumonia (often referred to as PJP or PCP) or toxoplasmosis
- phenytoin and phenobarbital, to treat epilepsy
- carbamazepine, to treat epilepsy and bipolar disorder
- St. John's wort (Hypericum perforatum), a herbal remedy to treat depression
These medicines may be affected by DOVATO or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take DOVATO
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box or bottle, ask your doctor or pharmacist for help.
How much to take
The usual dose of DOVATO in adults and in children over the age of 12 years weighing at least 40 kg is one tablet (50 mg dolutegravir and 300 mg lamivudine) taken once a day.
If you weigh less than 40kg, you cannot take DOVATO, because the dose of each component of this medicine cannot be adjusted to your weight. Your doctor might prescribe the components separately for you.
How to take it
Swallow the tablets whole with a full glass of water.
Antacid medicines
Antacids, to treat indigestion and heartburn, can stop DOVATO being absorbed into your body and make it less effective.
Do not take an antacid during the 6 hours before you take DOVATO, or for at least 2 hours after you take it. Other acid-lowering medicines like ranitidine and omeprazole can be taken at the same time as DOVATO. Talk to your doctor or pharmacist for further advice on taking acidlowering (antacid) medicines with DOVATO.
Calcium or iron supplements
Calcium or iron supplements can stop DOVATO being absorbed into your body and make it less effective.
Do not take a calcium or iron supplement during the 6 hours before you take DOVATO, or for at least 2 hours after you take it. If you take food with DOVATO, then you can take calcium and iron supplements at the same time as DOVATO.
When to take it
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
How long to take it
Continue taking your medicine for as long as your doctor tells you.
If you forget to take it
If you miss a dose, take it as soon as you remember. But if your next dose is due within 4 hours, skip the dose you missed and take the next one at the usual time. Then continue your treatment as before.
Do not take a double dose to make up for the dose that you missed. Just take it as soon as you remember.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much DOVATO. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Don't stop DOVATO without advice
Take DOVATO for as long as your doctor recommends. Don't stop unless your doctor advises you to.
If you have hepatitis B infection, don't stop DOVATO without your doctor's advice, as your hepatitis may come back
While you are using DOVATO
You will need regular blood tests For as long as you're taking DOVATO, your doctor will arrange regular blood tests to check for side effects.
Stay in regular contact with your doctor.
DOVATO helps to control your condition, but it is not a cure for HIV infection. You need to keep taking it every day to stop your illness from getting worse. Because DOVATO does not cure HIV infection, you may still develop other infections and illnesses linked to HIV infection.
Keep in touch with your doctor and don't stop taking DOVATO without your doctor's advice.
Protect other people
HIV infection is spread by sexual contact with someone who has the infection, or by transfer of infected blood (for example, by sharing injection needles). DOVATO will not stop you passing HIV infection on to other people. To protect other people from becoming infected with HIV:
- Use a condom when you have oral or penetrative sex
- Don't risk blood transfer - for example, don't share needles.
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking DOVATO.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
If you become pregnant while taking this medicine, tell your doctor immediately.
Keep all of your doctor's appointments so that your progress can be checked.
Things you must not do
Do not take DOVATO to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
DOVATO can make you dizzy and have other side effects that make you less alert
Be careful driving or operating machinery until you know how DOVATO affects you.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking DOVATO.
This medicine helps most people with HIV, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
When you're being treated for HIV, it can be hard to tell whether a symptom is a side effect of DOVATO or other medicines you are taking, or an effect of the HIV disease itself. So it is very important to talk to your doctor about any changes in your health.
Some side effects may only be seen in your blood tests, and may not appear immediately after you start taking DOVATO. If you get any of these effects, and if they are severe, your doctor may advise you to stop taking DOVATO.
As well as the effects listed below for DOVATO, other conditions can develop during therapy for HIV.
Allergic reactions.
See a doctor as soon as possible if you develop a rash.
Allergic reactions are uncommon in people taking DOVATO. Signs include:
- Skin rash
- A high temperature (fever)
- Lack of energy (fatigue)
- Swelling, sometimes of the face or mouth (angioedema), causing difficulty in breathing
- Muscle or joint aches.
Your doctor may decide to carry out tests on your liver, kidneys or blood, and may tell you to stop taking DOVATO.
Lactic acidosis
Lactic acidosis is a rare but serious side effect
Some people taking DOVATO, or other medicines like it (NRTIs), develop a condition called lactic acidosis, together with an enlarged liver.
Lactic acidosis is caused by a buildup of lactic acid in the body. It is rare; if it happens, it usually develops after a few months of treatment. It can be life-threatening, causing failure of internal organs.
Lactic acidosis is more likely to develop in people who have liver disease, especially in women.
Signs of lactic acidosis include:
- deep, rapid, difficult breathing
- drowsiness
- numbness or weakness in the limbs
- feeling sick (nausea), being sick (vomiting)
- stomach pain.
During your treatment, your doctor will monitor you for signs of lactic acidosis. If you have any of the symptoms listed above or any other symptoms that worry you see your doctor as soon as possible.
As well as the conditions listed above, other side effects can develop during combination therapy for HIV
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
Very common side effects
These may affect more than 1 in 10 people:
- Headache
- Feeling sick (nausea)
- Diarrhoea.
Common side effects:
These may affect up to 1 in 10 people:
- Suicidal thoughts (mainly in patients who have had depression or mental health problems before)
- Depression
- Being sick (vomiting)
- Stomach pains (abdominal pain)
- Stomach (abdominal) discomfort
- Wind (flatulence)
- Lack of energy (fatigue)
- Generally feeling unwell (malaise)
- High Temperature (fever)
- Dizziness
- Feeling drowsy
- Abnormal dreams
- Difficulty in sleeping (insomnia)
- Anxiety
- Hair loss (alopecia)
- Rash
- Itching (pruritus)
- Joint pain (arthralgia)
- Muscle disorders
Common side effects that may show up in your blood tests:
- an increase in lactic acid in the blood, which on rare occasions can lead to lactic acidosis.
Uncommon side effects
These may affect up to 1 in 100 people:
- allergic reaction (See 'allergic reactions' earlier in this section)
- inflammation of the liver (hepatitis)
- Suicide attempt (mainly in patients who have had depression or mental health problems before)
- muscle pain (myalgia)
- weight gain.
Uncommon side effects that may show up in blood tests are:
- a low red blood cell count (anaemia) or low white blood cell count (neutropenia)
- a decrease in the number of cells involved in blood clotting (thrombocytopenia)
- an increase in the level of liver enzymes.
Rare side effects
These may affect up to 1 in 1000 people:
- lactic acidosis (see 'lactic acidosis is a rare but serious side effect' earlier in this section)
- liver failure (signs may include yellowing of the skin and the whites of the eyes or unusually dark urine)
- inflammation of the pancreas (pancreatitis)
- breakdown of muscle tissue (rhabdomyolysis).
Rare side effects that may show up in blood tests are:
- increase in an enzyme called amylase.
Very rare side effects
These may affect up to 1 in 10,000 people:
- tingling or numbness of the hands and feet (paraesthesiae)
- numbness, tingling or weakness of the arms and legs (peripheral neuropathy).
Very rare side effects that may show up in blood tests are:
- failure of the bone marrow to produce new red blood cells (pure red cell aplasia).
Other side effects that may show up in blood tests
Other side effects have occurred in some people but their exact frequency is unknown:
- increase in bilirubin (a substance produced by the liver) in the blood
- an increase in the level of enzymes produced in the muscles (creatine phosphokinase)
- an increase in a kidney function blood test result (creatinine).
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Tell your doctor or pharmacist if any of the side effects gets severe or troublesome, or if you notice any side effects not listed in this leaflet.
Conditions you need to look out for
Some other conditions may develop during HIV treatment.
Symptoms of infection and inflammation
People with advanced HIV infection (AIDS) have weak immune systems, and are more likely to develop serious infections (opportunistic infections). When they start treatment, the immune system becomes stronger, so the body starts to fight infections.
Symptoms of infection and inflammation may develop, caused by either:
- old, hidden infections flaring up again as the body fights them
- the immune system attacking healthy body tissue (autoimmune disorders)
The symptoms of autoimmune disorders may develop many months after you start taking medicine to treat your HIV infection.
Symptoms may include:
- muscle weakness and/or muscle pain
- joint pain or swelling
- weakness beginning in the hands and feet and moving up towards the trunk of the body
- palpitations or tremor
- hyperactivity (excessive restlessness and movement).
If you get any symptoms of infection while you're taking DOVATO, tell your doctor immediately. Don't take other medicines for the infection without your doctor's advice.
After using DOVATO
Storage
Store in the original package. Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store DOVATO tablets or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
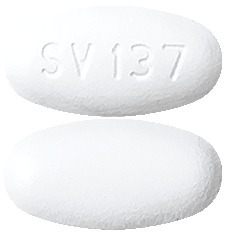
DOVATO tablets are oval, biconvex, white, film-coated tablet, debossed with "SV 137" on one face.
They are supplied in a white bottle which contains 30 tablets.
Ingredients
DOVATO tablets contain 50 mg of dolutegravir (as sodium) and 300 mg of lamivudine as the active ingredients.
DOVATO also contains
- Mannitol
- Magnesium stearate
- Microcrystalline cellulose
- Povidone
- Sodium starch glycollate Type A,
- Sodium stearylfumarate
- Hypromellose
- Macrogol 400
- Titanium dioxide
This medicine does not contain lactose, sucrose, gluten, tartrazine or any other azo dyes.
Supplier
DOVATO is supplied in Australia by:
ViiV Healthcare Pty Ltd
Level 4, 436 Johnston Street
Abbotsford, Victoria, 3067
Australia.
DOVATO: AUST R 309378
Trademarks are owned by or licensed to the ViiV Healthcare group of companies.
© 2021 ViiV Healthcare group of companies or its licensor.
This leaflet was prepared on 12 July 2021
Published by MIMS September 2021




 The rates of adverse events leading to discontinuation in the pooled analysis were 3% of subjects in both treatment arms. The most common adverse events leading to discontinuation were psychiatric disorders: 1% of subjects in both treatment arms. The incidence of serious adverse events was 9% in both treatment arms.
The rates of adverse events leading to discontinuation in the pooled analysis were 3% of subjects in both treatment arms. The most common adverse events leading to discontinuation were psychiatric disorders: 1% of subjects in both treatment arms. The incidence of serious adverse events was 9% in both treatment arms. The ADRs observed for the combination of dolutegravir and lamivudine in these studies were generally consistent with the ADR profiles and severities for the individual components when administered with other antiretroviral agents. A single treatment emergent ADR [Nervous system disorders: somnolence; frequency common] was observed with the combination which was not listed in the product information for dolutegravir or lamivudine.
The ADRs observed for the combination of dolutegravir and lamivudine in these studies were generally consistent with the ADR profiles and severities for the individual components when administered with other antiretroviral agents. A single treatment emergent ADR [Nervous system disorders: somnolence; frequency common] was observed with the combination which was not listed in the product information for dolutegravir or lamivudine.


 Virologic outcomes by baseline CD4+ (cells/mm3) in GEMINI-1 and GEMINI-2 at week 96 are shown in Table 9. In both trials, lower response rates (HIV-1 RNA < 50 copies/mL) were observed in subjects with baseline CD4+ ≤ 200 cells/mm3. These findings were seen irrespective of baseline plasma HIV-1 RNA.
Virologic outcomes by baseline CD4+ (cells/mm3) in GEMINI-1 and GEMINI-2 at week 96 are shown in Table 9. In both trials, lower response rates (HIV-1 RNA < 50 copies/mL) were observed in subjects with baseline CD4+ ≤ 200 cells/mm3. These findings were seen irrespective of baseline plasma HIV-1 RNA. The adjusted mean change from baseline in CD4+ cell count based on the pooled analysis at week 96 was 269 cells/mm3 for the group receiving dolutegravir plus lamivudine and 259 cells/mm3 for the group receiving dolutegravir plus tenofovir/emtricitabine FDC.
The adjusted mean change from baseline in CD4+ cell count based on the pooled analysis at week 96 was 269 cells/mm3 for the group receiving dolutegravir plus lamivudine and 259 cells/mm3 for the group receiving dolutegravir plus tenofovir/emtricitabine FDC. In TANGO, treatment outcomes between treatment arms were similar across the stratification factor, baseline third agent class (INSTI/NNRTI/PI), and across subgroups by age, sex, race, baseline CD4 cell count, CDC HIV disease stage and countries. The median change from baseline in CD4+ count at week 48 was 22.5 cells per mm3 in subjects who switched to Dovato and 11.0 cells per mm3 in subjects who stayed on TBR.
In TANGO, treatment outcomes between treatment arms were similar across the stratification factor, baseline third agent class (INSTI/NNRTI/PI), and across subgroups by age, sex, race, baseline CD4 cell count, CDC HIV disease stage and countries. The median change from baseline in CD4+ count at week 48 was 22.5 cells per mm3 in subjects who switched to Dovato and 11.0 cells per mm3 in subjects who stayed on TBR. Limited data are available in adolescents receiving a daily dose of 300 mg of lamivudine. Pharmacokinetic parameters are comparable to those reported in adults.
Limited data are available in adolescents receiving a daily dose of 300 mg of lamivudine. Pharmacokinetic parameters are comparable to those reported in adults. The structural formula of lamivudine is:
The structural formula of lamivudine is:
