What is in this leaflet
This leaflet answers some common questions about DuoResp Spiromax. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you using DuoResp Spiromax against the benefits they expect it will have for you.
If you have any concerns about using this medicine, ask your doctor or pharmacist.
Keep this leaflet with your DuoResp Spiromax.
You may need to read it again.
What DuoResp Spiromax is used for
DuoResp Spiromax is inhaled into the lungs for the treatment of asthma or Chronic Obstructive Pulmonary Disease (COPD).
DuoResp Spiromax contains two active ingredients in one inhaler: budesonide and formoterol (eformoterol) fumarate dihydrate (hereafter referred to as formoterol).
- Budesonide belongs to a group of medicines called corticosteroids. Budesonide acts directly on your airways to reduce inflammation.
- Formoterol belongs to a group of medicines called beta-2-agonists. Formoterol opens up the airways to help you breathe more easily.
ASTHMA
Asthma is a disease where the airways of the lungs become narrow and inflamed (swollen), making it difficult to breathe. This may for example be due to exercise, or exposure to allergens (e.g. an allergy to house dust mites, smoke or air pollution) or other things that irritate your lungs.
The budesonide in DuoResp Spiromax helps to improve your condition and to prevent asthma attacks from occurring.
The formoterol in DuoResp Spiromax helps you breathe more easily.
Some people can take DuoResp Spiromax when they need it – they use DuoResp Spiromax as an anti-inflammatory “reliever” to treat their symptoms when their asthma gets worse and to help prevent asthma attacks, or to help prevent symptoms from happening (e.g. before exercise or exposure to other triggers such as allergens).
Some people need to take DuoResp Spiromax every day – they use their DuoResp Spiromax as a daily maintenance preventer to help maintain control of their asthma symptoms and help prevent asthma attacks.
Chronic Obstructive Pulmonary Disease (COPD)
COPD (which includes chronic bronchitis and emphysema) is a long-term lung disease. There is often permanent narrowing and persistent inflammation of the airways.
Symptoms may include difficulty in breathing (breathlessness or wheezing), coughing and increased sputum.
DuoResp Spiromax when used as prescribed will help to control your COPD symptoms (i.e. breathing difficulties).
Ask your doctor if you have any questions about why DuoResp Spiromax has been prescribed for you. Your doctor may have prescribed it for another reason. The active substances in DuoResp Spiromax (budesonide and formoterol) are not addictive.
This medicine is available only with a doctor's prescription.
Before you use DuoResp Spiromax
When you must not use it
Do not use DuoResp Spiromax if you have an allergy to:
- any medicine containing formoterol or budesonide
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- rash, itching or hives on the skin
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body.
Do not give DuoResp Spiromax to a child or adolescent under 18 years.
Do not use DuoResp Spiromax after the expiry date (EXP) printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start using this medicine, talk to your doctor.
Before you start to use it
If you have asthma, ask your doctor or pharmacist if you have any questions about your Asthma Action Plan. Your doctor should give you a personal Asthma Action Plan to help manage your asthma. This plan will include what medicines to take as a reliever when you have symptoms or sudden attacks of asthma, medicines you can take to prevent symptoms from occurring (e.g. prior to exercise or allergen exposure) and if you need to take daily maintenance medicines to help control your asthma.
It is important that you discuss with your doctor both your exposure to triggers and how often you exercise, as these could impact how your doctor prescribes your DuoResp Spiromax.
Your doctor may prescribe DuoResp Spiromax for you to use as:
- an anti-inflammatory reliever medicine only,
- both an anti-inflammatory reliever and daily maintenance preventer medicine or,
- as a daily maintenance preventer only, where another medicine is used as a reliever.
Ask your doctor if you have any questions about how you should be using your DuoResp Spiromax.
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- thyroid or adrenal gland problems
- diabetes
- heart problems
- liver problems
- tuberculosis (TB)
- low levels of potassium in the blood
It may not be safe for you to take DuoResp Spiromax if you have, or have had, any of these conditions.
Tell your doctor if you currently have an infection. If you take DuoResp Spiromax while you have an infection, the medicine may hide some of the signs of an infection. This may make you think, mistakenly, that you are better or that it is not serious.
Tell your doctor if you are pregnant or intend to become pregnant or breastfeeding. Your doctor will discuss the possible risks and benefits of using DuoResp Spiromax during pregnancy and while breastfeeding.
If you have not told your doctor or pharmacist about any of the above, tell them before you start using DuoResp Spiromax.
Taking other medicines
Tell your doctor or pharmacist if you are using any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and DuoResp Spiromax may interfere with each other. These include:
- medicines used to treat heart problems or high blood pressure such as beta-blockers, diuretics and antiarrhythmics (disopyramide, procainamide and quinidine)
- medicines used to treat glaucoma such as beta-blockers
- medicines used to treat depression or other mood/mental disorders such as tricyclic antidepressants, monoamine oxidase inhibitors and phenothiazines
- medicines used to treat hayfever, coughs, colds and runny nose such as antihistamines
- medicines used to treat fungal infections (e.g. ketoconazole, itraconazole, voriconazole)
- xanthine derivatives (e.g. theophylline) which are a class of medicines used to treat asthma and COPD
- Medicines like digoxin used to treat heart failure
- Medicines used to treat HIV infection
- Medicines for Parkinson’s disease (e.g. L-dopa)
- Medicines for thyroid problems (e.g. thyroxine)
These medicines may be affected by DuoResp Spiromax, or may affect how well it works. You may need different amounts of your medicine, or you may need to use different medicines. Your doctor or pharmacist will advise you.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while using DuoResp Spiromax.
How to use DuoResp Spiromax
How to use your device
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
Each pack of DuoResp Spiromax contains an instruction leaflet that tells you the correct way to use it.
Please read this carefully.
If you are not sure how to use the device, ask your doctor or pharmacist to show you how.
How much to take
ASTHMA (Adults only)
Your doctor should give you a personal Asthma Action Plan to help manage your asthma. This plan will include what medicines to take as a reliever when you have symptoms or sudden attacks of asthma, medicines you take to prevent symptoms from occurring (e.g. prior to exercise or allergen exposure) and if you need to take daily maintenance medicines to help control your asthma.
It is important that you discuss with you doctor both your exposure to triggers and how often you exercise, as these could impact how your doctor prescribes your DuoResp Spiromax.
Your doctor may have prescribed DuoResp Spiromax for you to use as:
- an anti-inflammatory reliever medicine only,
- both an anti-inflammatory reliever and a daily maintenance preventer medicine or,
- as a daily maintenance preventer only, where another medicine is used as a reliever.
Ask your doctor if you have any questions about how you should be using your DuoResp Spiromax. If your asthma has been under control for some time, your doctor may tell you to take less inhalations of DuoResp Spiromax, prescribe you a lower strength of DuoResp Spiromax or recommend that you use DuoResp Spiromax in a different way.
If you are using more inhalations of your reliever medicine or you are wheezing or breathless more than usual tell your doctor as your asthma may be getting worse.
Anti-inflammatory reliever only (DuoResp Spiromax 200/6)
AUSTRALIA
Adults only:
DuoResp Spiromax 200/6 can be used to treat asthma symptoms when they happen and to help stop asthma symptoms from happening (e.g. just before exercise or before you get exposed to other triggers).
If you get asthma symptoms, take 1 inhalation and wait a few minutes. If you do not feel better, take another inhalation.
Your doctor will tell you how many inhalations to take before exercising or exposure to other triggers to help stop symptoms from happening.
Do not use more than 6 inhalations on a single occasion or more than 12 inhalations in any day. If your symptoms continue to worsen over 3 days, despite using additional inhalations, tell your doctor.
Have your DuoResp Spiromax reliever with you at all times.
NEW ZEALAND
Adults only, usual dose: If you experience symptoms or if you want to stop symptoms from happening, take 1 inhalation and wait a few minutes. If you don’t feel better, take another inhalation. You must not use more than 6 inhalations each time.
Contact your doctor:
- if you need to take an increasing number of inhalations for symptom relief without getting better asthma control within 2 weeks, or
- if you regularly use more than 8 inhalations per day
Never take more than 12 inhalations in total per day.
Anti-inflammatory reliever plus maintenance therapy (DuoResp Spiromax 200/6)
AUSTRALIA
Adults only
DuoResp Spiromax 200/6 can be used to treat asthma symptoms when they happen. DuoResp Spiromax 200/6 can also be used to help stop asthma symptoms from happening (e.g. just before exercise or before you get exposed to other triggers).
If you get asthma symptoms, take 1 inhalation of DuoResp Spiromax 200/6 and wait a few minutes. If you do not feel better, take another inhalation.
Your doctor will tell you how many inhalations of DuoResp Spiromax 200/6 to take before exercising or exposure to other triggers to help stop symptoms from happening.
Have your DuoResp Spiromax 200/6 reliever with you at all times.
You also need to take your DuoResp Spiromax 200/6 daily as your maintenance preventer. The usual maintenance dose is 2 inhalations per day (given either as 1 inhalation in the morning and evening or as 2 inhalations in either the morning or evening). Your doctor may prescribe a maintenance dose of DuoResp Spiromax 200/6, 2 inhalations twice a day.
Do not use more than 6 inhalations on a single occasion or more than 12 inhalations of DuoResp Spiromax (as needed and daily dose) in any day. If your symptoms continue to worsen over 3 days, despite using additional inhalations, tell your doctor.
NOTE: DuoResp Spiromax 400/12 is not recommended to be used as anti-inflammatory reliever medicine.
NEW ZEALAND
Adults only:
You take a maintenance dose of DuoResp Spiromax every day. You also use DuoResp Spiromax if you need extra doses for relief and prevention of asthma symptoms. This means that you use DuoResp Spiromax as your only inhaler both for regular daily use and as reliever medication. You will not need a separate inhaler for relief of symptoms.
Always carry DuoResp Spiromax with you for relief of symptoms. It is important that you contact your doctor if you find the treatment ineffective or if you exceed the highest recommended dose.
It is important that you discuss with your doctor both your exposure to “triggers” and how often you exercise, as these could impact the dose frequency that it is recommended to you.
DuoResp Spiromax 200/6
Usual doses for adults and adolescents 12 years and older:
- 2 inhalations per day, given either as one inhalation in the morning and evening or as 2 inhalations in either the morning or evening. Your doctor may prescribe a maintenance dose of 2 inhalations twice daily.
- If you experience symptoms or if you want to stop symptoms from happening, take 1 additional inhalation and wait a few minutes. If you don’t feel better, take another inhalation. You must not use more than 6 inhalations each time. Never take more than 12 inhalations in total per day.
Contact your doctor:
- If you need to take an increasing number of inhalations for symptom relief without getting better asthma control within 2 weeks, or
- If you regularly use more than 8 inhalations per day.
Daily fixed dose maintenance therapy (DuoResp Spiromax 200/6 and 400/12)
AUSTRALIA
Adults only
DuoResp Spiromax 200/6 can be used as a daily fixed-dose maintenance preventer. The usual dose is 1 2 inhalations twice a day.
DuoResp Spiromax 400/12 is recommended for only for patients who need a higher daily dose.
The usual dose is 2 inhalations twice a day. Your doctor may also tell you to take 1 inhalation twice a day, if your asthma has been under control.
Do not take more than 2 inhalations twice a day of DuoResp Spiromax 200/6 or 400/12.
Have your separate reliever with you at all times.
NEW ZEALAND
Adults only
As an alternative, you take a maintenance dose of DuoResp Spiromax every day (fixed dose). In addition, you use a separate inhaler, containing only a shortacting bronchodilator (airway widening medicine) for relief of asthma symptoms. This means that you use two separate inhalers. Always carry your reliever medication with you for relief of symptoms. It is important that you contact your doctor if you find the treatment ineffective or if you exceed the highest recommended dose.
DuoResp Spiromax 200/6
The usual dose:
- 1-2 inhalations once or twice daily
- Maximum daily maintenance dose: 4 inhalations
- Maximum dose during worsening asthma: 4 inhalations twice daily
DuoResp Spiromax 400/12
The usual dose:
- 1 inhalation once or twice daily
- Maximum daily maintenance dose: 2 inhalations
- Maximum dose during worsening asthma: 2 inhalations twice daily.
COPD (Adults)
The usual dose (also maximum recommended dose) is:
- 2 inhalations of DuoResp Spiromax 200/6 twice daily
or
- 1 inhalation of DuoResp Spiromax 400/12 twice daily.
Your doctor should tell you the best way to manage your symptoms and any flare ups. This may include additional medicines (such as reliever medicines) to use when you have sudden attacks of breathlessness.
If you are using more inhalations of your reliever medicine or you are wheezing or breathless more than usual tell your doctor.
If your COPD gets worse, your doctor may give you some additional medicines (such as oral corticosteroids or antibiotics).
If you forget to use it
If you miss a dose of DuoResp Spiromax, take your dose as soon as you remember.
Do not use a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are using DuoResp Spiromax as a reliever medicine, consult your doctor on the correct use of the product.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to use your medicine, ask your pharmacist for some hints.
How long to use it
If your doctor has told you to take DuoResp Spiromax daily, it is important that you use it every day even if you feel well.
DuoResp Spiromax helps control your asthma or COPD, but does not cure it.
Keep using it for as long as your doctor tells you to. Do not stop using it unless your doctor tells you to.
If you take too much (overdose)
Telephone your doctor, pharmacist or the Poisons Information Centre (Australia telephone 13 11 26, New Zealand telephone 0800 764 766), or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have used too much DuoResp Spiromax.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you use too much DuoResp Spiromax, you may feel sick or vomit, have a fast or irregular heartbeat, a headache, tremble, feel shaky, agitated, anxious, tense, restless, excited or be unable to sleep.
While you are using DuoResp Spiromax
Things you must do
If you have an Asthma Action Plan that you have agreed with your doctor, follow it closely at all times.
Keep using DuoResp Spiromax for as long as your doctor tells you to, even if you are feeling well.
See your doctor regularly to make sure that your asthma or COPD is not getting worse.
Have your reliever medicine available at all times. As advised by your doctor, this may be your DuoResp Spiromax (200/6) or another reliever medication.
Rinse your mouth out with water after taking your daily morning and/or evening dose of DuoResp Spiromax and spit this out. If you don't rinse your mouth you are more likely to develop thrush in your mouth. You do not have to rinse your mouth if you have to take occasional doses of DuoResp Spiromax for relief of asthma symptoms (i.e. as an anti-inflammatory reliever).
Tell any other doctors, dentists, and pharmacists who are treating you that you are using DuoResp Spiromax.
If you become pregnant while using DuoResp Spiromax, tell your doctor.
Patients taking DuoResp Spiromax for COPD should tell their doctor or pharmacist immediately if they notice any signs of pneumonia (infection of the lung). Signs include fever or chills, increased mucus production or change in mucus colour, increased cough or increased breathing difficulties. Pneumonia is a serious medical condition and will require urgent medical attention.
Things you must not do
Do not take any other medicines for your asthma or COPD without checking with your doctor.
Do not give DuoResp Spiromax to anyone else, even if they have the same condition as you.
Do not use DuoResp Spiromax to treat any other complaints unless your doctor tells you to.
Do not stop using DuoResp Spiromax without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how DuoResp Spiromax affects you.
DuoResp Spiromax may cause dizziness, blurred vision, light-headedness, tiredness or drowsiness in some people when they first start using it.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are using DuoResp Spiromax.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
If you get any side effects, do not stop using DuoResp Spiromax without first talking to your doctor or pharmacist.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- sore, yellowish, raised patches in the mouth (thrush)
- hoarse voice
- irritation of the tongue and mouth
- coughing
These are less likely to happen if you rinse your mouth out after every time you use your usual morning and/or evening dose of DuoResp Spiromax.
- trembling or shakiness
- feeling anxious, nervous, restless or upset
- fast or irregular heart rate or pounding heart
- chest pain
- headache
- feeling light-headed or dizzy
- thirsty
- unpleasant taste in your mouth
- nausea (feeling sick)
- diarrhoea
- difficulty sleeping
- muscle twitching or cramps
- skin rash
- tiredness
- weight gain
- skin bruising
These side effects are usually mild.
Tell your doctor immediately if you notice any of the following as they could be symptoms of a lung infection (pneumonia):
- fever or chills
- increased mucus production, change in mucus colour
- increased cough or increased breathing difficulties
Tell your doctor or pharmacist immediately if you notice any of the following:
- difficulty breathing or worsening of your breathing problems
- swelling of the face, lips, tongue or other parts of the body
- severe rash
- mood changes
These may be serious side effects. You may need urgent medical attention. Serious side effects are rare.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some patients.
Some of these side effects (for example, changes in blood sugars) can only be found when your doctor does tests from time to time to check your progress.
Tell your doctor if you notice any issues with your eyes such as blurred vision or other problems with your eyesight. Your doctor may need to send you to an ophthalmologist (eye doctor) to check that you don't have eye problems such as cataracts (clouding on the eye lens), glaucoma (increased pressure in your eyeballs) or other rare eye conditions reported with corticosteroid use.
Corticosteroids taken into the lungs for long periods (e.g. 12 months) may affect growth. In rare cases, some patients may be sensitive to the growth effects of corticosteroids, so the doctor may monitor a patient’s height.
After using DuoResp Spiromax
Cleaning
Keep your Spiromax device dry and clean. If necessary, you may wipe the mouthpiece of your Spiromax device after use with a dry cloth or tissue. Full instructions on the right way to use and clean DuoResp Spiromax are inside each pack.
Storage
Keep your Spiromax in a cool dry place where the temperature stays below 25°C, with the cover firmly in place.
Do not store DuoResp Spiromax or any other medicine in the bathroom or near a sink.
Do not leave it in the car on hot days or on a window sill. Heat and dampness can destroy some medicines.
Keep it where young children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
Since some medicine may remain inside your DuoResp Spiromax you should always return it to your pharmacist for disposal including:
- when you have taken all your doses and the dose indicator is on zero ('0' - see instructions in the pack), or
- if it is damaged or past its expiry date, or
- if it has been removed from the foil wrapping for greater than 6 months, or
- if your doctor/pharmacist has told you to stop using it.
Product description
What it looks like
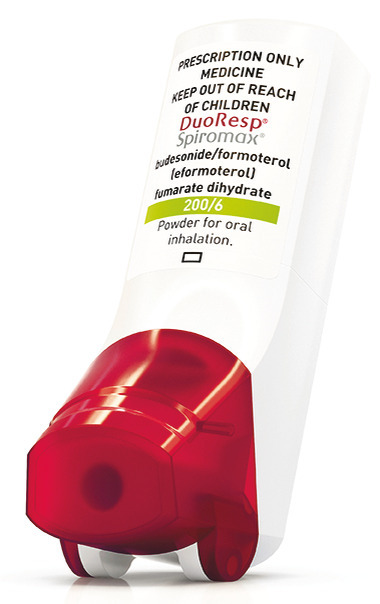
DuoResp Spiromax is a plastic inhaler containing the medicine as a dry powder. The Spiromax device is white in colour, with a semi-transparent wine red mouthpiece cover at the bottom.
DuoResp Spiromax 200/6 is registered in packs of 1, 2 or 3 inhalers. Each DuoResp Spiromax 200/6 inhaler contains 120 inhalations.
DuoResp Spiromax 400/12 is registered in packs of 1, 2 or 3 inhalers. Each DuoResp Spiromax 400/12 inhaler contains 60 inhalations.
Not all pack sizes may be marketed.
Ingredients
DuoResp Spiromax contains budesonide and formoterol (eformoterol) fumarate dihydrate as the active ingredients, and lactose monohydrate (which may contain milk protein residue).
The amount of lactose contained in DuoResp Spiromax is very small and does not normally cause problems in lactose intolerant people.
DuoResp Spiromax does not contain sucrose, gluten, tartrazine or any other azo dyes.
Sponsor
Teva Pharma Australia Pty Ltd
37 Epping Road
MACQUARIE PARK NSW 2113
Teva Pharma (New Zealand) Ltd
Auckland, New Zealand
This leaflet was prepared February 2020
Australian Registration Numbers
200/6 – AUST R 267385
400/12 – AUST R 267386
® DuoResp and Spiromax are registered trademarks of the Teva group of companies.
Published by MIMS July 2020



 As with other inhalation therapy, paradoxical bronchospasm may occur in very rare cases.
As with other inhalation therapy, paradoxical bronchospasm may occur in very rare cases. In these placebo-controlled studies, the incidence of pneumonia was low, with no consistent evidence of increased risk of pneumonia for budesonide + formoterol treated patients compared to patients on placebo.
In these placebo-controlled studies, the incidence of pneumonia was low, with no consistent evidence of increased risk of pneumonia for budesonide + formoterol treated patients compared to patients on placebo. Analysis of time to first severe exacerbation in SYGMA 1 showed that the likelihood of experiencing a severe exacerbation was statistically significantly higher for SABA as needed use compared to budesonide/formoterol anti-inflammatory reliever therapy over the 1 year treatment period, with a risk reduction of 56% (Hazard Ratio (HR): 0.44 (0.33, 0.58); p < 0.001). There were no differences in the probability of experiencing a severe exacerbation between budesonide/formoterol anti-inflammatory reliever therapy and a maintenance dose of budesonide given with SABA as needed.
Analysis of time to first severe exacerbation in SYGMA 1 showed that the likelihood of experiencing a severe exacerbation was statistically significantly higher for SABA as needed use compared to budesonide/formoterol anti-inflammatory reliever therapy over the 1 year treatment period, with a risk reduction of 56% (Hazard Ratio (HR): 0.44 (0.33, 0.58); p < 0.001). There were no differences in the probability of experiencing a severe exacerbation between budesonide/formoterol anti-inflammatory reliever therapy and a maintenance dose of budesonide given with SABA as needed.

 The study specifically demonstrates that both the budesonide and the formoterol components of budesonide/formoterol contribute to improved asthma control achieved through the as-needed dosing of budesonide/formoterol within the budesonide/formoterol anti-inflammatory reliever plus maintenance therapy concept.
The study specifically demonstrates that both the budesonide and the formoterol components of budesonide/formoterol contribute to improved asthma control achieved through the as-needed dosing of budesonide/formoterol within the budesonide/formoterol anti-inflammatory reliever plus maintenance therapy concept.

 This study showed that budesonide/formoterol anti-inflammatory reliever plus maintenance therapy treatment is more effective than adjustable therapy with fluticasone/salmeterol plus salbutamol in controlling asthma in adults and adolescents.
This study showed that budesonide/formoterol anti-inflammatory reliever plus maintenance therapy treatment is more effective than adjustable therapy with fluticasone/salmeterol plus salbutamol in controlling asthma in adults and adolescents. When administered twice daily, budesonide/formoterol 200/6 is a more effective treatment than budesonide, at corresponding budesonide doses.
When administered twice daily, budesonide/formoterol 200/6 is a more effective treatment than budesonide, at corresponding budesonide doses. In conclusion, there was a greater improvement in lung function and asthma control with budesonide/formoterol 100/6 than with a doubled dose of budesonide.
In conclusion, there was a greater improvement in lung function and asthma control with budesonide/formoterol 100/6 than with a doubled dose of budesonide. When administered twice daily, budesonide/formoterol 400/12 is a more effective treatment for the majority of clinical endpoints than the corresponding budesonide dose.
When administered twice daily, budesonide/formoterol 400/12 is a more effective treatment for the majority of clinical endpoints than the corresponding budesonide dose.

