SUMMARY CMI
DUROGESIC®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
WARNING: Important safety information is provided in a boxed warning in the full CMI. Read before using this medicine.
1. Why am I using DUROGESIC?
DUROGESIC contains the active ingredient fentanyl. DUROGESIC is used for the long-term management of severe pain that requires daily around-the-clock pain relievers, when other treatment options are not able to effectively manage your pain, or you cannot tolerate them. DUROGESIC is only used in people who have previously been using other opioid-based pain relief.
For more information, see Section 1. Why am I using DUROGESIC? in the full CMI.
2. What should I know before I use DUROGESIC?
Do not use if you have ever had an allergic reaction to fentanyl or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use DUROGESIC? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with DUROGESIC and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use DUROGESIC?
DUROGESIC is available in five different patches, each with a different size and strength. Your doctor will decide which patch, or combination of patches, is suitable to control your pain. The lowest effective strength should be used.
More instructions can be found in Section 4. How do I use DUROGESIC? in the full CMI.
5. What should I know while using DUROGESIC?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using DUROGESIC? in the full CMI.
6. Are there any side effects?
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
WARNING:
Limitations of use
DUROGESIC should only be used when your doctor decides that other treatment options are not able to effectively manage your pain or you cannot tolerate them.
Hazardous and harmful use
DUROGESIC poses risks of abuse, misuse and addiction which can lead to overdose and death. Your doctor will monitor you regularly during treatment
Life threatening respiratory depression
DUROGESIC can cause life-threatening or fatal breathing difficulties (slow, shallow, unusual or no breathing) even when used as recommended. These problems can occur at any time during use but the risk is higher when first starting DUROGESIC and after a dose increase, if you are older, or have an existing problem with your lungs. Your doctor will monitor you and change the dose as appropriate.
Concomitant use of benzodiazepines and other central nervous system (CNS) depressants, including alcohol
Using DUROGESIC with other medicines that can make you feel drowsy such as sleeping tablets (e.g. benzodiazepines), other pain relievers, antihistamines, antidepressants, antipsychotics, gabapentinoids (e.g. gabapentin and pregabalin), cannabis and alcohol may result in severe drowsiness, decreased awareness, breathing problems, coma and death. Your doctor will minimise the dose and duration of use; and monitor you for signs and symptoms of breathing difficulties and sedation. You must not drink alcohol while using DUROGESIC.
FULL CMI
DUROGESIC® Transdermal System
Active ingredient(s): fentanyl
Consumer Medicine Information (CMI)
This leaflet provides important information about using DUROGESIC. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using DUROGESIC.
Where to find information in this leaflet:
1. Why am I using DUROGESIC?
2. What should I know before I use DUROGESIC?
3. What if I am taking other medicines?
4. How do I use DUROGESIC?
5. What should I know while using DUROGESIC?
6. Are there any side effects?
7. Product details
1. Why am I using DUROGESIC?
DUROGESIC contains the active ingredient fentanyl. DUROGESIC is an opioid analgesic which are a group of strong pain relievers. Fentanyl relieves pain by blocking the nerves that recognise pain messages from the body.
DUROGESIC is used for the long-term management of pain that is severe enough to require daily around-the-clock pain relievers, when other treatment options are not able to effectively manage your pain or you cannot tolerate them. DUROGESIC is only used in people who have previously been using other opioid-based pain relief. DUROGESIC is not used to treat pain that you only have once in a while.
Each patch is applied onto the skin every three days (72 hours). The patch releases a continuous amount of fentanyl that is absorbed through the skin in contact with the patch.
2. What should I know before I use DUROGESIC?
Warnings
Opioids can be abused and misused, and you are at risk for opioid addiction, even if you take your dose as prescribed. Opioid addiction, abuse and misuse can lead to overdose and death.
DUROGESIC may become habit-forming causing mental and physical dependence. If abused, it may become less able to reduce pain.
DUROGESIC patches may be retrieved and abused or misused illegally. Please ensure that used patches are concealed and disposed of carefully. Return unused patches to the pharmacy (see Getting rid of any unwanted medicine at the end of this leaflet).
Keep used and unused patches where children cannot reach them. A patch may be tempting to a child. Accidental exposure or ingestion of used or unused DUROGESIC patches, particularly in children, may result in breathing difficulties, with slow or shallow breathing, that could lead to death. Improper use including DUROGESIC patches sticking to another person can be life-threatening.
DUROGESIC can cause sleep apnoea (stopping breathing from time to time while sleeping) which can lead to low levels of oxygen in the blood. Tell your doctor if you have a history of sleep apnoea or if anyone notices you stop breathing from time to time whilst sleeping.
Opioids can cause a high level of the hormone 'prolactin' and low levels of sex hormones in the blood. The effects of these hormone changes may include:
- In females – unexpected production of breast milk; loss of menstrual periods
- In males – enlarged breasts; difficulty getting and keeping an erection (impotence)
- In females or males – decreased sex drive; infertility.
Tell your doctor if you notice any of these symptoms. You may need blood tests, and your doctor may tell you to stop using DUROGESIC.
Opioids can cause a decreased level of hormones in the blood caused by a problem with the adrenal glands. The effects of these hormone changes may include:
- Nausea, vomiting, loss of appetite, feeling very tired and weak, feeling dizzy, or low blood pressure.
Tell your doctor if you notice any of these symptoms. You may need blood tests, and your doctor may tell you to stop using DUROGESIC.
Tolerance
As with all opioid analgesics, DUROGESIC may lead to tolerance with continued use. Tolerance means that the effect of the medicine may decrease and more is needed to produce the same effect. Therefore, it is possible your doctor will prescribe a higher dose of DUROGESIC after some time to produce the same result.
Dependance and withdrawal
As with all other opioids, your body may become used to you taking DUROGESIC after several days to weeks of continued use resulting in physical dependence. Physical dependence means that you may experience withdrawal symptoms if you stop taking DUROGESIC suddenly. Some examples of withdrawal symptoms include feeling uneasy and unwell, restless, agitated, anxious, increased pain, sweating, chills, weakness, stomach cramps, problems sleeping, nausea, vomiting, diarrhoea, increased blood pressure, fast breathing and fast heartbeat.
DUROGESIC must be stopped by decreasing the dose gradually. Your doctor will tell you how to do this, and will regularly monitor and support any increase in pain or withdrawal symptoms.
Increased sensitivity to pain
Rarely, increasing the dose of this medicine can make you more sensitive to pain. If this happens, you need to speak to your doctor about your treatment.
Do not use DUROGESIC:
- if you are allergic to fentanyl or any of the ingredients listed at the end of this leaflet
- Always check the ingredients to make sure you can use this medicine
- for acute pain or pain following surgery
- for mild or intermittent pain
- at a starting dose greater than 25 micrograms/hour
- if you have any lung condition or breathing difficulties
- if you have not used any opioid analgesics in the past. This is because you may be more likely to experience some of the side effects.
- Do not use DUROGESIC if the packaging is torn or shows signs of tampering.
- Do not use DUROGESIC beyond the expiry date (month and year) printed on the pack.
Check with your doctor if you:
- have any other medical conditions particularly:
- have or have ever had problems with your liver or kidney
- have or have ever had problems with your lungs or breathing difficulties
- have sleep apnoea or if anyone notices you stop breathing from time to time while sleeping
- have or have ever had problems with your heart
- have or have ever had a brain tumour or head injuries
- have problems with your stomach or intestines such as bowel blockage
- have problems with your immune system or medical conditions which lower your resistance to diseases. - take any medicines for any other condition
- (or a family member) have ever abused or been dependent on alcohol, prescription medicines, or illegal drugs or have a mental illness. Your doctor will advise you whether or not to use DUROGESIC or if you need to adjust the dose or adapt your treatment.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
Your doctor will decide whether you may use DUROGESIC if you are pregnant or plan to become pregnant.
DUROGESIC should not be used during childbirth as the medicine can slow the breathing of the newborn child. Prolonged use of DUROGESIC during pregnancy can cause withdrawal symptoms in your newborn baby that could be life-threatening if not recognised and treated.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
If you are breast feeding, you should not use DUROGESIC since it may be present in your milk. See your doctor.
Use in children and adolescents
DUROGESIC should not be used in children under 12 years of age or in adolescents under 18 years of age who weigh less than 50 kg.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with DUROGESIC and affect how it works.
In particular, tell your doctor or pharmacist if you are taking any of the following:
- medicines that slow down your central nervous system, for example:
- medicines that makes you sleepy, reduce anxiety such as sedatives, hypnotics, sleeping tablets, tranquillisers (benzodiazepines)
- other opioid medicines
- medicines used for surgery (anesthetics) and muscle relaxants
- antihistamines or allergy medicine that makes you drowsy
- gabapentinoid medicines used to treat epilepsy or nerve pain such as gabapentin and pregabalin
- alcohol, cannabis or some illegal drugs.
Taking these medicines with DUROGESIC may make you even more drowsy, slow down your ability to react, have decrease awareness, breathing difficulties with slow or shallow breathing, coma and death.
A change in dose by your doctor may be required if DUROGESIC is used with these medicines:
- antidepressant medicines belonging to the class monoamine oxidase inhibitors (MAOIs).
DUROGESIC should not be used together with MAOIs as this may cause severe serotonin syndrome which is a potentially life-threatening condition. Signs and symptoms can include confusion, restlessness, fever, heavy sweating, fast or irregular heart rate, diarrhoea, uncoordinated movement of limbs or eyes, uncontrollable jerking of muscles, seizures and unconsciousness. Do not use DUROGESIC if you have taken a MAOI in the last 14 days. - other antidepressant medicines belonging to the class selective serotonin re-uptake inhibitors (SSRIs), serotonin norepinephrine re-uptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs) and nefazodone.
Combination of these medicines with DUROGESIC may increase the risk of serotonin syndrome. - medicines used to treat mental illness or psychotic conditions and to relieve severe nausea and vomiting, such as phenothiazines.
- certain antibiotics used to treat infections such as erythromycin, clarithromycin and troleandomycin.
- certain medicines to treat fungal infections such as fluconazole, ketoconazole, itraconazole and voriconazole.
- ritonavir and nelfinavir (used to treat AIDS).
Do not take ritonavir or nelfinavir while using DUROGESIC, unless you are closely monitored by your doctor. - if taking rifampicin, carbamazepine, phenobarbital or phenytoin, careful monitoring by your doctor and dose adjustment may be required.
- idelalisib (cancer treatment)
- certain medicines that act on the heart and blood vessels such as calcium-channel blockers like verapamil and diltiazem, nicardipine.
- certain medicines used to treat arrhythmias such as amiodarone.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect DUROGESIC.
4. How do I use DUROGESIC?
How much to use
- DUROGESIC is available in five different patches, each with a different size and strength. Your doctor will decide which patch, or combination of patches, is suitable to control your pain. The lowest effective strength should be used.
Using it for the first time
- The first patch may take up to a day to take effect after it is applied onto the skin. This is because fentanyl is slowly absorbed through the skin into the blood. Your doctor may prescribe additional medicines to control the pain for the first day.
Using and changing the patches
- Make a note of the day, date and time you apply a patch, to remind you when you need to change your patch.
- There is enough medicine in each patch to last 3 days (72 hours).
- You should change your patch every third day, unless your doctor has told you differently. If the patch comes off before 3 days, a new patch of the same strength should be applied to a new spot of intact skin.
- Always remove the old patch before applying a new one.
- Always change your patch at the same time of day every 3 days (72 hours).
- You should not use more than one patch at a time, unless your doctor authorises otherwise (for example to obtain a dose that cannot be achieved with a single patch).
- If you are using more than one patch, change all your patches at the same time.
- The old patch should be removed before the new patch is applied.
Where to apply DUROGESIC
DUROGESIC should be applied to non-irritated and non-irradiated skin on a flat surface of the upper body or upper arms.
Do not apply the patch on:
- the same place twice in a row
- areas that you move a lot (joints)
- skin that is red, burnt or damaged
- hairy skin
How to apply DUROGESIC
Step 1: Preparing the skin
- Hair at the application site (a hairless area is preferable) should be trimmed with scissors (not shaved) prior to application. The skin should be healthy and undamaged. Do not place the patch onto skin that is red, burnt or damaged.
- If the site of DUROGESIC application needs to be cleaned before applying the patch, this should be done with clear water. Do not use soaps, oils, or any other cleaners, creams or moisturisers.
- Make sure your skin is completely dry before the patch is applied. Do not stick a patch on straight after a hot bath or shower. Patches should be inspected prior to use.
Step 2: Open the pouch
- DUROGESIC patch should be applied immediately upon removal from the sealed package.
- To remove the patch from the protective pouch, locate the precut notch (indicated by an arrow on the patch label) along the edge of the seal.
- Fold the pouch at the notch, then carefully tear the pouch material.
- Inspect the patch for any damage. Patches that are cut, divided, or damaged in any way should not be used.
- Further open the pouch along both sides, folding the pouch open like a book.

- The clear plastic protective (release) liner for the patch is slit.
- Fold the patch in the middle and remove each half of the liner separately.
Step 3: Peel and press
- Avoid touching the adhesive side of the patch.
- Apply the patch to the skin by applying light pressure with the palm of the hand for about 30 seconds.
- Make sure the entire patch is in contact with skin, the corners and the edges of the patch are adhering properly.
- Then wash hands with clean water.
Step 4: Disposing of the patch
- As soon as you take a patch off, fold it firmly in half so that the sticky side sticks to itself.
- Put it back in its original sachet and dispose of the sachet as instructed by your pharmacist.
- Unused patches should be returned to the pharmacy.
- Keep used patches out of sight and reach of children – even used patches contain some medicine which may harm children and may even be fatal.
Step 5: Wash
- Always wash your hands after you have handled the patch using clean water only.
If you do not understand the instructions provided with this medicine, ask your doctor or pharmacist for help.
If you forget to use DUROGESIC
If you forget to apply a patch, and are not sure what to do, check with your doctor or pharmacist.
If you have trouble remembering when to apply each patch, ask your pharmacist for some hints.
If you use too much DUROGESIC
If you think that you have used too much DUROGESIC, you may need urgent medical attention.
You should immediately remove the patch(es) and phone triple zero (000) for an ambulance. Keep the person awake by talking to them or gently shaking them every now and then.
Also,
- phone the Poisons Information Centre
(by calling 13 11 26) for advice, or - go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
Symptoms of an overdose with DUROGESIC may include:
- Slow, unusual or difficult breathing
- Drowsiness, dizziness or unconsciousness
- Slow or weak heart beat
- Nausea or vomiting
- Convulsions or fits
Other signs of overdose can also include problems with the 'nervous system' caused by damage to the white matter of the brain (known as toxic leukoencephalopathy).
When seeking medical attention, take this leaflet and remaining medicine with you to show the doctor. Also tell them about any other medicines or alcohol which have been taken.
5. What should I know while using DUROGESIC?
Things you should do
- Always follow your doctor's instructions carefully.
- If you are pregnant or plan to become pregnant, you should inform your doctor, who will decide whether you may use DUROGESIC.
- If your pain continues or returns, see your doctor. You may need additional medicines to control the pain or a change in the strength of the DUROGESIC patch.
- If you are about to start taking a new medicine, tell your doctor and pharmacist that you are using DUROGESIC.
Call your doctor straight away if you:
- develop a fever. At high temperatures, the amount of fentanyl absorbed by the skin increases. Your doctor may need to adjust your DUROGESIC dose.
Remind any doctor, dentist or pharmacist you visit that you are using DUROGESIC.
Things you should not do
- Do not stop using this medicine suddenly unless your doctor advises you to do so. If you have been using DUROGESIC for a long period of time but stop using it suddenly without your doctor's advice, you may experience withdrawal symptoms such as:
- trouble sleeping, nervousness, restlessness, agitation or anxiety
- body aches, weakness or stomach cramps
- loss of appetite, nausea, vomiting or diarrhoea
- increased heart rate, breathing rate or pupil size
- watery eyes, runny nose, chills or yawning
- increased sweating
Seek your doctor's advice if you experience these symptoms. - DO NOT expose the patch to direct heat from electric blankets, heat pads, heated water beds, heat or tanning lamps, intensive sunbathing, hot water bottles, long hot baths, saunas or hot spa baths while you are using DUROGESIC. Direct exposure to such heat may cause an increase in the amount of fentanyl absorbed by the skin, resulting in possible overdose and death.
- Do not cut, break, chew, crush, dissolve, snort or inject DUROGESIC. This can result in serious side effects and death.
- Do not change your dose without first checking with your doctor
- Do not give the patches to anyone else, even if their symptoms seem similar to yours as they could die from taking it.
Things to be careful of
- If the patch accidentally sticks to another person (for example a family member sharing the same bed) or is accidentally swallowed (for example by a child), remove the patch and phone triple zero (000). Do this even if there are no signs of discomfort or drowsiness.
- Different brands of fentanyl patches may vary in size, shape, colour or adhesiveness.
- DO NOT switch brands of fentanyl patches unless your doctor and pharmacist authorise it.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how DUROGESIC affects you.
DUROGESIC can affect your alertness and ability to drive and operate machinery. Do not drive or operate machinery until you know how this medicine affects you.
Drinking alcohol
Tell your doctor if you drink alcohol.
You must not drink alcohol while using DUROGESIC since their combined effect may cause severe drowsiness, decreased awareness, breathing problems, coma and death.
Looking after your medicine
- Keep the patches in a dry place where temperature stays below 30°C.
- Store this medicine securely, where other people cannot access it. It may harm people who may take this medicine by accident, or intentionally when it has not been prescribed for them.
- Keep DUROGESIC patches in the sealed pouch until it is time to apply them.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
The contents of DUROGESIC patches may be retrieved and abused or misused illegally.
Fold used patches so that the adhesive side of the patch sticks to itself, then wrap and dispose of it carefully.
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
Gastrointestinal-related:
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
Heart-related:
| REMOVE the DUROGESIC patch and phone triple zero (000) or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. Make sure that you are with someone who can keep you awake by talking to you or gently shaking you every now and then. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What DUROGESIC contains
| Active ingredient (main ingredient) | fentanyl |
| Other ingredients (inactive ingredients) | polyethylene terephalate ethylene/VA copolymer polyacrylate adhesive Duro-Tak 87-4287 |
Do not take this medicine if you are allergic to any of these ingredients.
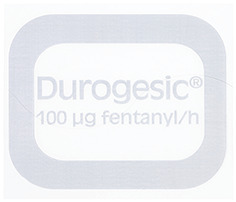
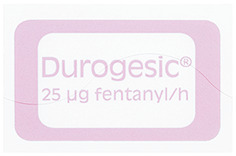
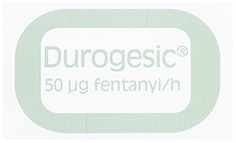
What DUROGESIC looks like
DUROGESIC packs each contain 5 patches and are available in five sizes. The number after the name DUROGESIC refers to the amount of fentanyl in micrograms (one thousandth of a milligram) released by the patch per hour:
- DUROGESIC 12 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 12 mcg fentanyl/h" in orange ink (AUST R 116828)
- DUROGESIC 25 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 25 mcg fentanyl/h" in red ink (AUST R 112368)
- DUROGESIC 50 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 50 mcg fentanyl/h" in green ink (AUST R 112369)
- DUROGESIC 75 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 75 mcg fentanyl/h" in blue ink (AUST R 112370)
- DUROGESIC 100 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 100 mcg fentanyl/h" in grey ink (AUST R 112371)
Who distributes DUROGESIC
Janssen-Cilag Pty Ltd
1-5 Khartoum Road
Macquarie Park NSW 2113 Australia
Telephone: 1800 226 334
This leaflet was prepared in November 2024.
Published by MIMS January 2025



 For a full list of excipients, see Section 6.1 List of Excipients.
For a full list of excipients, see Section 6.1 List of Excipients. Durogesic 12 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 12 mcg fentanyl/h" in orange ink.
Durogesic 12 micrograms/hour patches are rectangular shape with rounded corners, translucent system with printed border and "Durogesic 12 mcg fentanyl/h" in orange ink.

 The initial evaluation of the maximum analgesic effect of Durogesic should not be made before the patch has been worn for 24 hours. This is due to the gradual increase in serum fentanyl concentration in the 24 hours following initial application of the patch. Previous analgesic therapy should therefore be phased out gradually after the initial dose application until the analgesic efficacy with Durogesic is attained.
The initial evaluation of the maximum analgesic effect of Durogesic should not be made before the patch has been worn for 24 hours. This is due to the gradual increase in serum fentanyl concentration in the 24 hours following initial application of the patch. Previous analgesic therapy should therefore be phased out gradually after the initial dose application until the analgesic efficacy with Durogesic is attained.

 Adverse drug reactions not reported in Table 7 that were reported by ≥ 1% of Durogesic treated subjects (N = 1854) in 11 clinical trials of Durogesic used for the treatment of chronic malignant or nonmalignant pain (which includes trial FEN-EMA-1) are shown in Table 8. All subjects took at least one dose of Durogesic and provided safety data.
Adverse drug reactions not reported in Table 7 that were reported by ≥ 1% of Durogesic treated subjects (N = 1854) in 11 clinical trials of Durogesic used for the treatment of chronic malignant or nonmalignant pain (which includes trial FEN-EMA-1) are shown in Table 8. All subjects took at least one dose of Durogesic and provided safety data. Adverse drug reactions reported by < 1% of Durogesic treated subjects (N = 1854) in the above clinical trial dataset are shown in Table 9.
Adverse drug reactions reported by < 1% of Durogesic treated subjects (N = 1854) in the above clinical trial dataset are shown in Table 9.
 The release of fentanyl from the patch is sufficiently controlled by the skin stratum corneum. While the actual rate of fentanyl delivery to the skin varies over the 72-hour application period, each patch is labelled as the average amount of fentanyl delivered to the systemic circulation per hour across average skin.
The release of fentanyl from the patch is sufficiently controlled by the skin stratum corneum. While the actual rate of fentanyl delivery to the skin varies over the 72-hour application period, each patch is labelled as the average amount of fentanyl delivered to the systemic circulation per hour across average skin. N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl] propanamide. C22H28N2O. MW: 336.46.
N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl] propanamide. C22H28N2O. MW: 336.46.