What is in this leaflet
This leaflet answers some common questions about EDURANT tablets. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you being given EDURANT against the benefits this medicine is expected to have for you.
If you have any concerns about being given EDURANT ask your doctor.
Keep this leaflet while you are taking EDURANT. You may need to read it again.
What EDURANT is used for
EDURANT is a medicine used for the treatment of Human Immunodeficiency Virus (HIV) infection. It belongs to a group of anti-HIV medicines called non-nucleoside reverse transcriptase inhibitors (NNRTIs). EDURANT works by reducing the amount of HIV in your body. This will improve your immune system and reduce the risk of developing illnesses linked to HIV infection.
EDURANT is used to treat adults who are infected by HIV and who have not used other anti-HIV medicines before.
EDURANT must be taken in combination with other anti-HIV medicines. Your doctor will discuss with you which combination of medicines is best for you.
Ask your doctor if you have any questions about why EDURANT has been prescribed for you.
This medicine is available only with a doctor's prescription.
Before you take EDURANT
When you must not use it:
Do not take EDURANT:
- if you are allergic (hypersensitive) to rilpivirine, or other ingredients of EDURANT. See Product Description at the end of this leaflet for a list of ingredients.
Do not take EDURANT:
- if the packaging is torn or shows signs of tampering.
- if the expiry date (month and year) printed on the pack has passed. If you take EDURANT after the expiry date it may not work.
Do not combine EDURANT with any of the following medicines:
- carbamazepine, oxcarbazepine, phenobarbital, phenytoin (to treat epilepsy or prevent seizures)
- non-nucleoside reverse transcriptase inhibitors (NNRTIs) (HIV medicines)
- rifampicin, rifapentine (to treat some infections such as tuberculosis)
- products that contain St John's wort (Hypericum perforatum) (a herbal product used for depression)
- omeprazole, esomeprazole, lansoprazole, rabeprazole, pantoprazole (to treat gastrointestinal ulcers, heartburn or acid reflux disease)
- dexamethasone (a corticosteroid used in a variety of conditions such as inflammation and allergic reactions)
If you are taking any of these, ask your doctor for advice.
There are other medicines that you need to be careful of when taking EDURANT (see Taking other medicines).
Before you start to use it:
Take special care with EDURANT:
EDURANT is not a cure for HIV infection. It is part of a treatment reducing the amount of virus in the blood.
EDURANT does not reduce the risk of passing HIV to others through sexual contact or blood contamination. Therefore, you must continue to use appropriate precautions (a condom or other barrier method) to lower the chance of sexual contact with any body fluids such as semen, vaginal secretions or blood.
People taking EDURANT may still develop infections or other illnesses associated with HIV infection. You must keep in regular contact with your doctor to monitor your health while taking EDURANT.
EDURANT is not for use in children or adolescents, because it has not been sufficiently studied in patients under 18 years of age.
EDURANT has only been used in a limited number of patients aged 65 years or older. If you belong to this age group, discuss the use of EDURANT with your doctor.
Tell your doctor if you have or have had any medical conditions, especially the following:
- Problems with your liver.
Including hepatitis B and/or C. Your doctor may need to evaluate how severe your liver disease is before deciding if you can take EDURANT. - Symptoms of infection or inflammation.
In some patients with advanced HIV infection, signs and symptoms of infection or inflammation may occur after HIV treatment is started. It is believed that these symptoms are due to an improvement in the body's immune response. - Changes in body shape or fat.
Redistribution, accumulation or loss of body fat may occur in patients receiving a combination of antiretroviral medicines.
Tell your doctor immediately if you are pregnant or breast-feeding, or intend to become pregnant or breast-feed.
Pregnant women should discuss the use of EDURANT with their doctor.
During pregnancy you should not take EDURANT, unless it is specifically approved by your doctor.
HIV infected mothers must not breast-feed, as there is a possibility of infecting the baby with HIV.
If you have not told your doctor about any of the above, tell them before you start treatment with EDURANT.
Taking other medicines:
EDURANT might interact with other medicines. Tell your doctor if you are taking any other medicines, including medicines you can buy without a prescription from a pharmacy, supermarket or health food shop.
EDURANT can be combined with most other anti-HIV medicines belonging to another class. However, some combinations are not recommended. In other cases, increased monitoring and/or a change in the dose of the medicine may be needed. Therefore, always tell your doctor which other anti-HIV medicines you take. Carefully follow your doctor's instructions, on which medicines can be combined.
In addition to other anti-HIV medicines that you take, tell your doctor or pharmacist if you are taking any of the following:
- rifabutin (a medicine to treat some bacterial infections). If you take this medicine while taking EDURANT, please carefully read the section entitled 'Taking EDURANT'
- cimetidine, famotidine, nizatidine, ranitidine (antihistamines used to treat stomach or intestinal ulcers or used to relieve heartburn from acid reflux)
- antacids (for example, aluminium / magnesium hydroxide, calcium carbonate)
- clarithromycin, erythromycin, troleandomycin (antibiotics)
- methadone (strong pain killer also used in drug dependence programs)
Taking EDURANT
How much EDURANT to take:
Always take EDURANT exactly as your doctor has told you. You must check with your doctor if you are not sure.
The usual dose of EDURANT is one tablet taken once daily with a meal.
Instructions:
- It is important that you take EDURANT with a meal. A meal is important to get the right drug levels in your body. A protein drink alone does not replace a meal.
If you take rifabutin (a medicine to treat some bacterial infections), take two tablets of EDURANT once a day. When you stop taking rifabutin, take one tablet of EDURANT once a day. Talk to your doctor or pharmacist if you are not sure.
If you take an antacid (a medicine to treat diseases related to the acid in the stomach such as aluminium/magnesium hydroxide, calcium carbonate), take the antacid either at least 2 hours before or at least 4 hours after EDURANT. If you take an H2-receptor antagonist (medicines used for stomach ulcers, heartburn, or acid reflux disease (such as cimetidine, famotidine, nizatidine or ranitidine), take the H2-receptor antagonist at least 12 hours before or at least 4 hours after EDURANT. Importantly, proton pump inhibitors (such as omeprazole, lansoprazole, rabeprazole, pantoprazole, esomeprazole) also available for these conditions should not be taken with EDURANT.
Make sure that you always have enough EDURANT available so that you don't run out. For example in case you cannot return home, need to travel or stay in a hospital.
Removing the child resistant cap
The plastic bottle comes with a child resistant cap and should be opened as follows:
- Push the plastic screw cap down while turning it counter-clockwise.
- Remove the unscrewed cap

What do I do if I forget to take EDURANT?
If you notice within 12 hours of the time you usually take EDURANT, you must take the tablet as soon as possible. Always take the tablet with a meal. Then take the next dose as usual. If you notice after 12 hours, then skip the intake and take the next doses as usual. Do not take a double dose to make up for a forgotten dose.
What do I do if I take too much? (overdose):
If you think you or anybody else has taken too much EDURANT, contact your doctor, pharmacist or the Poisons Information Centre who will advise you what to do.
You can contact the Poisons Information Centre by dialling:
- Australia: 13 11 26
- New Zealand: 0800 POISON or 0800 764 766.
While you are taking EDURANT
Things you must do:
Do not stop taking EDURANT without talking to your doctor first. HIV therapy may increase your sense of well being. Even if you feel better, do not stop taking EDURANT or your other anti-HIV medicines. Doing so could increase the risk of the virus developing resistance. Talk to your doctor first.
Be sure to keep all your doctor's appointments so your progress can be checked. Your doctor will want to do some blood and other tests from time to time to check on your progress.
Be sure to follow up your doctor's instructions about other medicines you should take, and other things you should do. Ask your doctor or pharmacist if you have any questions.
Tell any other doctors and pharmacists who are treating you that you are taking EDURANT. If you are undergoing anaesthesia, tell your anaesthetist that you are taking EDURANT.
If you are about to be started on any new medicines, tell your doctor or pharmacist that you are taking EDURANT.
If you become pregnant while taking EDURANT, tell your doctor immediately. If you have any further questions on the use of this product, ask your doctor.
Things to be careful of
Driving and using machines
EDURANT has no or negligible influence on the ability to drive and use machines.
Side Effects
Like all medicines, EDURANT can have side effects. Some of these effects may be serious.
Tell your doctor or pharmacist if you do not feel well while you are being treated with EDURANT.
When treating HIV infection, it is not always easy to identify what side effects are caused by EDURANT, which are caused by other medicines you are taking, or which are caused by the HIV infection itself.
The most common side effects are:
- skin rash.
The rash is usually mild to moderate. In rare instances, rash can be potentially life-threatening. It is therefore important to contact your doctor immediately if you develop a rash. Your doctor will advise you how to deal with your symptoms or whether EDURANT must be stopped. - stomach pain, nausea
- depression, difficulty falling asleep (insomnia), abnormal dreams, sleep disorders
- decreased appetite
- tiredness
- changes in your routine liver tests
- headache
Uncommon side effects include:
- changes in your routine blood tests
- dizziness, drowsiness
- vomiting, stomach discomfort
Some side effects are typical for combination anti-HIV therapy. These are:
- change in body shape due to fat redistribution. This may include loss of fat from legs, arms and face, increased fat in the abdomen (belly) and other internal organs, breast enlargement and fatty lumps on the back of the neck (buffalo hump). The cause and long-term health effects of these conditions are not known at this time.
- immune reconstitution syndrome. In some patients with advanced HIV infection (AIDS) and a history of opportunistic infection, signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is started, including EDURANT. In addition to the opportunistic infections, autoimmune disorders (a condition that occurs when the immune system attacks healthy body tissue) may also occur after you start taking medicines for the treatment of your HIV infection. Autoimmune disorders may occur many months after the start of treatment. It is believed that these symptoms are due to an improvement in the body's immune response, enabling the body to fight infections that may have been present with no obvious symptoms.
If you experience any of these side effects and they worry you, or if you notice any side effects not listed in this leaflet, please tell your doctor.
Other side effects not listed above may also occur in some people.
Product Description
Storage
EDURANT tablets should be kept out of reach of children, in a location where the temperature stays below 30°C.
EDURANT tablets should be stored in the original bottle. Keep the bottle tightly closed in order to protect from moisture and light.
What it looks like:
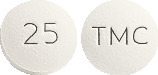
EDURANT tablets are white to off-white, film-coated, round, biconvex tablet, with "TMC" on one side and "25" on the other side.
Each plastic bottle contains 30 tablets.
Ingredients
Active ingredient:
- rilpivirine 25 mg
Other ingredients:
- glycerol triacetate
- silicified microcrystalline cellulose
- magnesium stearate
- hypromellose
- croscarmellose sodium
- lactose monohydrate
- povidone
- polysorbate 20
- titanium dioxide
- macrogol 3000
Sponsor
JANSSEN-CILAG Pty Ltd
1-5 Khartoum Rd
Macquarie Park NSW 2113 Australia
Telephone: 1800 226 334
NZ Office: Auckland, New Zealand
Telephone: 0800 800 806
Registration number
25 mg Tablet: AUST R 176666
This leaflet was prepared in June 2018.
Published by MIMS September 2018



 No new AR terms were identified in adult patients in the Phase III ECHO and THRIVE trials between 48 weeks and 96 weeks nor in the Phase IIb TMC278 C204 trial through 240 weeks.
No new AR terms were identified in adult patients in the Phase III ECHO and THRIVE trials between 48 weeks and 96 weeks nor in the Phase IIb TMC278 C204 trial through 240 weeks.

 Table 7 shows the efficacy results at 48 weeks and at 96 weeks for patients treated with Edurant and patients treated with efavirenz from the pooled data from the ECHO and THRIVE trials. Similar efficacy for rilpivirine was seen in each trial demonstrating non-inferiority to efavirenz, i.e. estimated treatment difference (95% CI) was -0.4 (-5.9; 5.2) and 3.5 (-1.7; 8.8) at week 48 (primary) and -3.2 (-9.4; 3.1) and 2.4 (-3.6; 8.4) at week 96, in ECHO and THRIVE respectively.
Table 7 shows the efficacy results at 48 weeks and at 96 weeks for patients treated with Edurant and patients treated with efavirenz from the pooled data from the ECHO and THRIVE trials. Similar efficacy for rilpivirine was seen in each trial demonstrating non-inferiority to efavirenz, i.e. estimated treatment difference (95% CI) was -0.4 (-5.9; 5.2) and 3.5 (-1.7; 8.8) at week 48 (primary) and -3.2 (-9.4; 3.1) and 2.4 (-3.6; 8.4) at week 96, in ECHO and THRIVE respectively. The mean change from baseline in CD4+ cell count was +192 x 106 cells/L in the rilpivirine arm and +176 x 106 cells/L in the efavirenz arm in the pooled analysis of the ECHO and THRIVE trials [estimated treatment difference (95% CI): 17.9 (2.1; 33.6)] at week 48. At week 96, the mean change from baseline in CD4+ cell count was +228 x 106 cells/L in the Edurant arm (n = 685) and +219 x 106 cells/L in the efavirenz arm (n = 682) in the pooled analysis of the ECHO and THRIVE trials [estimated treatment difference (95% CI): 11.3 (-6.8; 29.4)].
The mean change from baseline in CD4+ cell count was +192 x 106 cells/L in the rilpivirine arm and +176 x 106 cells/L in the efavirenz arm in the pooled analysis of the ECHO and THRIVE trials [estimated treatment difference (95% CI): 17.9 (2.1; 33.6)] at week 48. At week 96, the mean change from baseline in CD4+ cell count was +228 x 106 cells/L in the Edurant arm (n = 685) and +219 x 106 cells/L in the efavirenz arm (n = 682) in the pooled analysis of the ECHO and THRIVE trials [estimated treatment difference (95% CI): 11.3 (-6.8; 29.4)]. At week 96, response rates (< 50 copies/mL [TLOVR]) in the pooled Phase III trial population were 84.0% in the Edurant arm and 79.9% in the efavirenz arm in patients with a baseline viral load ≤ 100,000 copies/mL versus 70.1% and 75.4%, respectively, in patients with a baseline viral load > 100,000 copies/mL. The proportion of virologic failures according to TLOVR in the pooled Phase III trial population was 5.7% in the Edurant arm and 3.6% in the efavirenz arm, for patients with a baseline viral load ≤ 100,000 copies/mL. The proportion of virologic failures was higher for patients with a baseline viral load > 100,000 copies/mL, especially in the Edurant arm (18.2% Edurant-treated patients vs. 7.9% efavirenz-treated patients).
At week 96, response rates (< 50 copies/mL [TLOVR]) in the pooled Phase III trial population were 84.0% in the Edurant arm and 79.9% in the efavirenz arm in patients with a baseline viral load ≤ 100,000 copies/mL versus 70.1% and 75.4%, respectively, in patients with a baseline viral load > 100,000 copies/mL. The proportion of virologic failures according to TLOVR in the pooled Phase III trial population was 5.7% in the Edurant arm and 3.6% in the efavirenz arm, for patients with a baseline viral load ≤ 100,000 copies/mL. The proportion of virologic failures was higher for patients with a baseline viral load > 100,000 copies/mL, especially in the Edurant arm (18.2% Edurant-treated patients vs. 7.9% efavirenz-treated patients).

