What is in this leaflet
This leaflet answers some common questions about EMLA. It does not contain all the available information that is known about EMLA. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you or your child using EMLA against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What EMLA is used for
EMLA is a mixture of two local anaesthetics, lidocaine (lignocaine) and prilocaine.
These local anaesthetics are combined with special agents which allow the products to pass through the skin. Once through the skin the numbing effect they produce allows minor surgical procedures to be performed with a significant reduction in pain.
These procedures can include taking blood samples, vaccination, skin grafting, cleaning leg ulcers, inserting an intravenous catheter, minor superficial cosmetic procedures and procedures on genital skin.
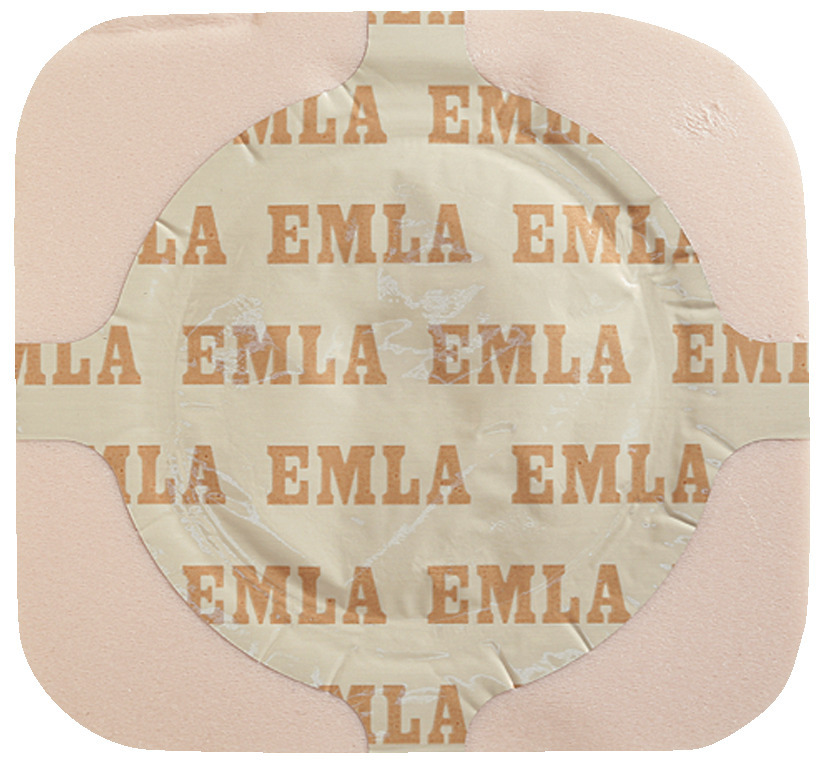
EMLA is available as a cream which is applied then covered with a dressing, or as a patch, which has the cream and dressing already to use.
Follow all directions given to you by your doctor carefully. They may differ from the information contained in this leaflet.
Your doctor or pharmacist may prescribe this medicine for another use. Ask your doctor or pharmacist if you want more information.
EMLA is not addictive.
Before you use EMLA
When you must not use it
Do not apply EMLA cream to any open wounds except leg ulcers.
Do not use EMLA if you are pregnant or breastfeeding unless your doctor says it is safe. The ingredients in EMLA have been used for many years and no ill effects have been shown if they are used while you are pregnant.
Only very small amounts of EMLA get into the blood so even though your baby can take in EMLA from breast milk if you are breastfeeding, it is unlikely to cause any problems.
Ask your doctor about the risks and benefits of using this medicine while you are pregnant or breastfeeding.
EMLA should not be used in premature babies. We do not have enough knowledge yet to be sure it is safe in premature babies.
Do not use after the use by (expiry) date printed on the pack or the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
Do not use it to treat any other complaints unless your doctor says it is safe.
Do not give this medicine to anyone else.
Before you start to use it
You must tell your doctor or pharmacist about any of these:
- allergies you or your child have to any
- ingredients listed at the end of this leaflet
- local anaesthetic, for example those used at the dentist
- adhesives or sticking plasters.
If you or your child have an allergic reaction, you may get a skin rash, hay fever or an asthma attack.
- any of these medical conditions
- dermatitis
- methaemoglobinaemia
- glucose-6-phosphate dehydrogenase deficiency
- mollusca contagiosa.
It may not be safe for you or your child to use EMLA if you have any of these conditions.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including
- a sulphonamide antibiotic eg sulfatrimoxazole
- medicines used to treat irregular heartbeat such as amiodarone
- medicines that you buy at your pharmacy, supermarket or health food shop
- other local anaesthetics.
These medicines may affect the way EMLA works or may cause adverse effects.
Your doctor or pharmacist can tell you what to do if you are taking any of these medicines.
How to use EMLA
How to use it
EMLA is available as a cream or a patch.
Instructions on how to use it are included in the box. Please read them carefully. The instructions also give maximum doses for adults and children. Do not exceed the maximum doses.
On intact skin
The most important thing to do is to be sure that you apply EMLA at least one hour before you are due to have the procedure except for skin grafting where a two hour application time is required or for procedures on male genital skin where only fifteen minutes is required.
Leg ulcers
If you are using EMLA on leg ulcers you only need to apply the cream 30 minutes before your ulcer is going to be cleaned.
EMLA can be left on for several hours and still work.
If you forget to use it
Apply EMLA as soon as you realise it if it is less than an hour until you are supposed to have the procedure. Tell your doctor exactly when you put EMLA on and they will decide when the procedure can take place.
If you have trouble remembering when to use your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Telephone your doctor or Poisons Information Centre (13 11 26), or go to Accident and Emergency at your nearest hospital immediately if you think that you or anyone else may have used too much EMLA even if there are no signs of discomfort or poisoning.
For most procedures, it is very difficult to use too much EMLA. Be careful not to use too much in procedures where larger amounts may be required, such as cosmetic hair removal (see Package Insert for maximum amounts). Using too much EMLA may cause unwanted side effects. Some of these can be serious, such as methaemoglobinaemia (a condition where the blood cannot take enough oxygen to your body) or cardiovascular effects (effects on your heart and lungs). If you use too much EMLA, you may notice the following:
- nervousness
- dizziness
- difficulty breathing
- numbness of the mouth
- your skin turning blue (a symptom of methaemoglobinaemia)
- blurred vision
- shaky hands
- a rash where EMLA has not been applied.
While you are using EMLA
Things you must do
Remember to apply EMLA on intact skin at least one hour before your procedure is due. For leg ulcers remember to apply EMLA 30 minutes before your ulcer is due to be cleaned. Apply EMLA two hours before split skin grafting and at least fifteen minutes before a procedure on male genital skin. If you do not, your or your child's appointment may have to be delayed, or the procedure may hurt more than it would otherwise.
If you or your child are using EMLA on leg ulcers, only use the tube once. Throw out any cream left in the tube after use.
Things to be careful of
Do not use EMLA cream on leg ulcers for longer than 2 months without checking with your doctor or pharmacist.
Be sure to follow the instructions in the pack on how to apply EMLA cream or patch carefully.
Make sure the patch or the dressing covering the cream is firmly fixed, especially on young children. If EMLA is not covered carefully it may not work effectively.
Be careful not to let EMLA get into the eyes. It may cause eye irritation. If EMLA does get into your eyes, immediately rinse them with large amounts of water and contact your doctor or pharmacist for advice.
Side effects
Tell your doctor or pharmacist as soon as possible if you or your child do not feel well while using EMLA. EMLA helps most people to undergo minor procedures without feeling pain, but it may have unwanted side-effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not.
You may need medical treatment if you or your child get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- any local reaction such as itching, swelling, paleness, redness or a burning sensation.
These are all mild side effects of EMLA.
If any of the following happen, remove EMLA and tell your doctor immediately or go to casualty at your nearest hospital.
- a rash at a spot where EMLA is not being used
- difficulty breathing
- dizziness
- shaky hands
- blurred vision
- areas of skin becoming blue
These are very serious side effects. If you or your child have them, you or your child may have had a serious reaction to EMLA and urgent medical attention or hospitalisation may be required.
All of these side effects are very rare.
Tell your doctor or pharmacist if you notice anything else that is making you or your child feel unwell. Some people may get other side effects while using EMLA.
After using EMLA
Storage
Keep your cream or patches in the pack until it is time to use them. If you squeeze EMLA out of the tube or open the patches it will not keep well.
Keep EMLA cream in a cool dry place where the temperature stays below 30°C. Do not let it freeze.
Keep EMLA patches in a cool dry place where the temperature stays below 25°C. Do not let them freeze.
Do not store EMLA or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where young children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
Ask your pharmacist what to do with any EMLA you have left over if your doctor tells you to stop using it, or you find that it has expired.
Product description
EMLA Cream and Patch contain as the active ingredients:
lidocaine (lignocaine) 25 mg/g and
prilocaine 25 mg/g
Plus,
carbomer 934P
polyoxyethylene hydrogenated castor oil
sodium hydroxide
EMLA Cream
5 x 5 g tubes (with 10 dressings)
1 x 5 g tube (with 2 dressings) or 30 g tube.
EMLA Patch
packs of 2 or 20 patches.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos St
St Leonards NSW 2065
Australia
This leaflet was revised in June 2025
Australian Registration Number (ARTG)
EMLA Cream
1 or 5 x 5 g - 12046
30 g - 12886
EMLA Patch - 60820
Published by MIMS August 2025



 A 1 g dose of EMLA cream is achieved by squeezing EMLA from the tube into a circular area with diameter of approximately 20 mm (the size of a 2 dollar coin) to a depth of approximately 4 mm. Keep the tube in close contact with the skin until the correct amount has been applied.
A 1 g dose of EMLA cream is achieved by squeezing EMLA from the tube into a circular area with diameter of approximately 20 mm (the size of a 2 dollar coin) to a depth of approximately 4 mm. Keep the tube in close contact with the skin until the correct amount has been applied.