What is in this leaflet
This leaflet answers some common questions about Enablex.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available.
You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on the medicine. You can also download the most up to date leaflet from
www.aspencmi.com.au
Those updates may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Enablex against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Enablex is used for
Enablex is used to decrease the urgency and the frequency of urination.
Enablex works by relaxing the bladder smooth muscle and helps to decrease muscle spasm. This delays the initial desire and the urge to urinate.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is available only with a doctor's prescription. It is not addictive.
Enablex is not recommended for use in children because there have been no studies of its effects in this age group.
Before you take Enablex
When you must not take it
Do not take Enablex if you have an allergy to darifenacin, the active ingredient, or to any of the other ingredients listed at the end of this leaflet. Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips and tongue or other parts of the body; rash itching or hives on the skin.
Do not take Enablex if you have any of the following medical conditions:
- a disorder of the eye called narrow angle glaucoma that is not being controlled with medicine
- a blockage in the stomach or intestine
- urinary tract blockage
Do not take Enablex after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. In that case, return it to your pharmacist.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, dyes or preservatives.
Tell your doctor if you are pregnant or intend to become pregnant. There is no information on the use of this medicine during pregnancy. Your doctor will discuss the possible risks and benefits involved.
Tell your doctor if you are breast-feeding or plan to breast-feed. It is not known if the active ingredient of Enablex passes into breast milk and could affect your baby. Your doctor will discuss the possible risks and benefits of breast-feeding while taking Enablex.
Tell your doctor if you have or have had any medical conditions, especially the following:
- heart problems
- liver problems
- narrow-angle glaucoma that is controlled with medicine
- stomach, intestinal or large bowel problems, including chronic constipation.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Enablex may interfere with each other. These include:
- some medicines used to treat fungal infections, such as ketoconazole, itraconazole and miconazole
- some medicines used to treat depression, such as paroxetine, fluoxetine, nefazodone and tricyclic antidepressants
- some medicines used to treat heart problems, such as digoxin and flecainide
- cimetidine, a medicine used to treat stomach ulcers
- ritonavir, a medicine used to treat HIV/AIDS
- thioridazine, a medicine used to treat schizophrenia
- a variety of other medicines that work in a similar way to Enablex.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking Enablex.
If you have not told your doctor about any of the above, tell him/her before you start taking Enablex.
How to take Enablex
Follow all directions given to you by your doctor and pharmacist carefully. These instructions may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
The usual starting dose is one 7.5 mg tablet once a day.
If necessary, your doctor may increase your dose to one 15 mg tablet once a day, as early as two weeks after starting therapy.
If you have a problem with your liver or are taking certain medicines, your doctor may limit your dose to one 7.5 mg tablet once a day.
How to take it
Swallow the tablet whole with a glass of water. Do not chew, crush or divide the tablet.
You can take the tablet with or without food.
When to take it
Take Enablex at about the same time each day. Taking your tablet at the same time each day will have the best effect. It will also help you remember when to take it.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
How long to take it
Continue taking this medicine for as long as your doctor tells you to. Enablex helps control your condition, but does not cure it. Therefore, you must take this medicine every day.
If you take too much (overdose)
Immediately telephone your doctor or pharmacist or the Poisons Information Centre (telephone 13 11 26), or go to accident and emergency at your nearest hospital, if you think that you or anyone else may have taken too much Enablex. Do this even if there are no signs of discomfort or poisoning.
Keep the telephone numbers for these places handy.
While you are taking Enablex
Things you must do
If you become pregnant while taking Enablex, tell your doctor. Your doctor can discuss with you the risks of taking it while you are pregnant.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are taking Enablex.
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking Enablex.
Things you must not do
Do not give this medicine to anyone else, even if their condition seems similar to yours.
Do not take it to treat any other complaints unless your doctor tells you to.
Things to be careful of
Be careful driving, operating machinery or doing jobs that require you to be alert while you are taking Enablex until you know how it affects you. This medicine may cause dizziness or blurred vision in some people.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Enablex, even if you do not think it is connected with the medicine.
This medicine helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist if you notice any of the following and they worry you:
- constipation
- diarrhoea
- stomach ache or indigestion
- nausea or vomiting
- nasal dryness
- flatulence
- dry or itchy skin
- dry eyes
- blurred or changed vision
- dryness of the mouth, nose and throat
- sore throat or cough
- change in taste
- mouth ulcers
- swelling of the hands, ankles or feet
- unusual tiredness, confusion or weakness
- difficulty sleeping
- dizziness
- pain in the joints
- discharge or itching in the vagina
- signs of a possible urinary tract infection, such as pain on urination
- urinary retention
- fast or irregular heart beats
- weight gain
- excessive sweating
- impotence
If any of the above symptoms are severe, tell your doctor immediately.
If any of the following happen, stop taking Enablex and tell your doctor immediately, or go to Accident and Emergency at your nearest hospital:
- sudden signs of allergy such as rash, itching or hives on the skin, swelling of the face, lips, tongue or other parts of the body, shortness of breath, wheezing or trouble breathing.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell. Other side effects not listed above may occur in some patients. Some side effects, such as raised blood pressure, may not give you any symptoms and can only be found when tests are done.
After using Enablex
Storage
- Keep your tablets in the original pack until it is time to take them.
- Store the tablets in a cool dry place at room temperature.
- Always keep the tablets away from direct sunlight and away from moisture.
- Do not store Enablex or any other medicine in the bathroom or near a sink.
- Do not leave it in the car or on window sills.
Keep the medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking Enablex or the tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
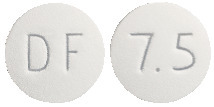
Enablex 7.5 mg tablets are round white tablets marked with "DF" on one side and "7.5" on the other side; packs of 28 tablets.
Enablex 15 mg tablets are round light-peach-coloured tablets marked with "DF" on one side and "15" on the other side; packs of 28 tablets.
Ingredients
Enablex contains 7.5 or 15 mg of the active ingredient, darifenacin (as the hydrobromide salt). The tablets also contain:
- calcium hydrogen phosphate anhydrous
- hypromellose
- magnesium stearate
The 7.5 mg tablets contain Opadry White (00F18296). The 15 mg tablets contain Opadry Yellow (00F12951) and Opadry Red (00F15613).
Enablex does not contain sucrose, gluten, tartrazine or any other azo dyes.
Sponsor
Enablex tablets are supplied in Australia by:
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Australia.
®= Registered Trademark
Enablex 7.5 mg AUST R 99418
Enablex 15 mg AUST R 99439
This leaflet was updated in May 2013.
Published by MIMS December 2025


 Discontinuations due to any adverse events occurred in 1.2% and 4.5% of 7.5 mg and 15 mg Enablex patients treated in fixed dose placebo controlled trials, respectively and in 1.3% of placebo subjects. There were no discontinuations due to laboratory test abnormalities.
Discontinuations due to any adverse events occurred in 1.2% and 4.5% of 7.5 mg and 15 mg Enablex patients treated in fixed dose placebo controlled trials, respectively and in 1.3% of placebo subjects. There were no discontinuations due to laboratory test abnormalities.
 In this study, darifenacin 15 mg and 75 mg doses demonstrated a mean heart rate change of 3.1 and 1.3 bpm, respectively, when compared to placebo. However, in the phase II/III clinical studies, the change in median heart rate following treatment with Enablex was no different from placebo.
In this study, darifenacin 15 mg and 75 mg doses demonstrated a mean heart rate change of 3.1 and 1.3 bpm, respectively, when compared to placebo. However, in the phase II/III clinical studies, the change in median heart rate following treatment with Enablex was no different from placebo.
 Incontinence responders (see Table 4) were defined as patients who achieved a 50% or greater reduction from baseline in the number of incontinence episodes per week. Frequency responders (see Table 6) were defined as the proportion of patients with ≥ 8 micturitions/day at baseline who achieved a normalisation of micturition, defined as a frequency of micturition of < 8 micturitions per day.
Incontinence responders (see Table 4) were defined as patients who achieved a 50% or greater reduction from baseline in the number of incontinence episodes per week. Frequency responders (see Table 6) were defined as the proportion of patients with ≥ 8 micturitions/day at baseline who achieved a normalisation of micturition, defined as a frequency of micturition of < 8 micturitions per day. As seen in Figure 1, significant improvement in the number of incontinence episodes per week was observed within the first 2 weeks in patients treated with Enablex 7.5 mg and 15 mg once daily compared to placebo. Further, these effects were sustained throughout the 12 week treatment period.
As seen in Figure 1, significant improvement in the number of incontinence episodes per week was observed within the first 2 weeks in patients treated with Enablex 7.5 mg and 15 mg once daily compared to placebo. Further, these effects were sustained throughout the 12 week treatment period. In a pooled analysis, significant improvements from baseline were also observed for key secondary efficacy endpoints, including the number of micturitions per day, the number and severity of urgency episodes, the average volume of urine passed per void and the number of incontinence episodes requiring a change of clothing or pads.
In a pooled analysis, significant improvements from baseline were also observed for key secondary efficacy endpoints, including the number of micturitions per day, the number and severity of urgency episodes, the average volume of urine passed per void and the number of incontinence episodes requiring a change of clothing or pads.
 Chemical name: (S)-2-{1-[2-(2,3- dihydrobenzofuran-5-yl) ethyl]-3-pyrrolidinyl}-2,2- diphenylacetamide hydrobromide.
Chemical name: (S)-2-{1-[2-(2,3- dihydrobenzofuran-5-yl) ethyl]-3-pyrrolidinyl}-2,2- diphenylacetamide hydrobromide.