What is in this leaflet
This leaflet answers some common questions about ENERZAIR BREEZHALER.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking ENERZAIR BREEZHALER against the benefits they expect it will have for you.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available.
You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on the medicine.
You can also download the most up to date leaflet from www.novartis.com.au Those updates may contain important information about the medicine and its use of which you should be aware.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What ENERZAIR Breezhaler is used for
Your doctor has prescribed this medicine to treat asthma in adults.
Asthma is a serious, long-term lung disease where the muscles surrounding the smaller airways become tight (bronchoconstriction), swollen and irritated (inflammation). Symptoms come and go, and include shortness of breath, wheezing, chest tightness and cough.
Enerzair capsules for inhalation contains three active substances called indacaterol, glycopyrronium and mometasone furoate.
Indacaterol and glycopyrronium belong to a group of medicines called bronchodilators. They relax the muscles of the small airways in the lungs. This helps to open the airways and makes it easier for air to get in and out of the lungs. When they are taken regularly, it helps the small airways to remain open.
Mometasone furoate belongs to a group of medicines called corticosteroids, often simply called steroids. Corticosteroids reduce inflammation. They reduce the swelling and irritation in the small airways in the lungs and so gradually ease breathing problems. Corticosteroids also help to prevent attacks of asthma.
The pack contains an inhaler (Breezhaler®) and capsules (in blister cards) that contain the medicine as inhalation powder. The inhaler enables you to inhale (breathe into the lungs) the medicine contained in a capsule. Only use the inhaler provided in the pack.
You should use ENERZAIR BREEZHALER every day as directed by your doctor and not only when you have breathing problems or other symptoms of asthma. This will make sure that it works properly in controlling your asthma. It should not be used to relieve a sudden attack of breathlessness or wheezing.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is not addictive.
This medicine is available only with a doctor's prescription.
Before you use ENERZAIR Breezhaler
When you must not use it
Do not use ENERZAIR BREEZHALER if you have an allergy (hypersensitive) to:
- lactose or milk protein
- indacaterol, glycopyrronium, mometasone furoate, or any other ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not give this medicine to a child or adolescent under the age of 18 years. Safety and effectiveness in children younger than 18 years have not been established.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to use it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- heart problems, including an irregular or fast heart beat
- thyroid gland problems
- diabetes or high blood sugar
- suffer from seizures or fits
- low potassium in your blood
- severe liver problems
- severe kidney problems
- eye problem called narrow-angle glaucoma
- difficulty passing urine
- tuberculosis
- chronic infections
Tell your doctor if you are pregnant or plan to become pregnant or are breast-feeding. Your doctor can discuss with you the risks and benefits involved.
ENERZAIR Breezhaler should only be used during pregnancy if the expected benefit to the patient justifies the potential risk to the fetus.
It is not known whether the active ingredients passes into breast milk. If you are breast-feeding, your doctor will help you decide whether you can use ENERZAIR Breezhaler.
If you have not told your doctor about any of the above, tell him/ her before you start taking ENERZAIR BREEZHALER.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Enerzair may interfere with each other. These include:
- medicines to treat depression (e.g. tricyclic antidepressants, monoamine oxidase inhibitors)
- medicines similar to ENERZAIR Breezhaler (contain similar active substances); these medicines may increase the risk of experiencing possible side effects
- medicines that decrease the level of potassium in your blood such as diuretics (also known as “water tablets” and used to treat high blood pressure, e.g. hydrochlorothiazide), other bronchodilators such as methylxanthines for breathing problems (e.g. theophylline) or steroids (e.g. prednisolone)
- medicine to treat high blood pressure or other heart problems (e.g. propranolol) or to treat glaucoma (e.g. timolol)
- medicine to treat fungal infections (e.g., ketoconazole or itraconazole)
- medicine to treat HIV infection (e.g., ritonavir, nelfinavir or cobicistat)
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to inhale ENERZAIR Breezhaler
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions in the user leaflet ask your doctor or pharmacist for help.
How much to inhale
There are two dose strengths of ENERZAIR Breezhaler, 114/46/68 micrograms and 114/46/136 micrograms. Your doctor will decide which dose strength is appropriate for you.
The usual dose is to inhale the content of one capsule each day. You only need to use this medicine once a day because its effect lasts for 24 hours. Do not use more than your doctor tells you to use.
You should inhale the content of one capsule of ENERZAIR Breezhaler every day and continue to use it even when you are not experiencing asthma symptoms.
How to use the Breezhaler
Carefully read the full Instructions for use provided in the package leaflet before use.
Only use the capsules with the inhaler provided in the pack. The capsules should remain in the blister until you need to use them.
Peel the backing away from the blister to open it; do not push the capsule through the foil.
Do not swallow the capsules.
Ensure you rinse your mouth out with water after each use.
Make sure you understand how to use the Breezhaler properly. If you are not sure, ask your doctor or pharmacist.
When to use it
Inhale ENERZAIR Breezhaler at the same time each day. This will help minimise your symptoms throughout the day and night. It will also help you to remember to use your medicine.
How long to use it
Keep using ENERZAIR Breezhaler for as long as your doctor tells you.
Don’t stop unless your doctor advises you to, even if you feel better, as your symptoms may get worse.
This medicine helps to control your condition, but does not cure it. Your asthma symptoms may come back if you stop using this medicine.
If you have questions about how long to continue your treatment with ENERZAIR Breezhaler, talk to your doctor or your pharmacist.
If you forget to take it
If you forget to inhale a dose, inhale the dose as soon as possible. Then inhale the next dose at the usual time. However, do not inhale two doses on the same day. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much Enerzair. Do this even if there are no signs of discomfort or poisoning.
While you are using ENERZAIR Breezhaler
Things you must do
Only use the inhaler contained in the pack.
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are using ENERZAIR Breezhaler.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
If you become pregnant while taking this medicine, tell your doctor immediately.
Keep all of your doctor's appointments so that your progress can be checked.
Stop taking ENERZAIR Breezhaler and seek medical help immediately if you experience any of the following:
- tightness of the chest, coughing, wheezing or breathlessness immediately after inhalation of ENERZAIR Breezhaler (signs of paradoxical bronchospasm).
- difficulty breathing or swallowing, swelling of the tongue, lips or face, skin rash, itching and hives (signs of allergic reaction)
- eye pain or discomfort, temporary blurring of vision, visual halos or coloured images in association with red eyes (signs of an acute attack of narrow-angle glaucoma).
Things you must not do
Do not use ENERZAIR Breezhaler to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how ENERZAIR Breezhaler affects you.
Side effects
As with all medicines, patients using ENERZAIR Breezhaler may experience side effects, although not everybody gets them.
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking ENERZAIR BREEZHALER.
This medicine helps most people with asthma, but it may have unwanted side effects in a few people. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Common side effects
- oral thrush (signs of candidiasis)
- a frequent urge to urinate and pain or burning when urinating (signs of urinary tract infection)
- fast heart beat
- headache
- sore throat
- cough
- voice alteration (hoarseness)
- diarrhoea, abdominal cramps, nausea, and vomiting (gastroenteritis)
- dry mouth
- rash
- muscle spasm
- pain in muscles, bones or joints (signs of musculoskeletal pain)
- fever
The above list may affect up to 1 in every 10 people.
Uncommon side effects
- high level of sugar in the blood
- skin itching
- difficulty and pain when passing urine (signs of dysuria)
The above list may affect up to 1 in every 100 people.
If these side effects become severe, tell your doctor or pharmacist.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After using ENERZAIR Breezhaler
Cleaning and Storage
Follow the instructions in the user leaflet on how to properly clean and take care of your ENERZAIR Breezhaler.
Keep your capsules in the original blister in order to protect from moisture and light, and do not remove until immediately before use.
Keep your capsules in a cool dry place where the temperature stays below 30°C.
Do not store ENERZAIR BREEZHALER or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
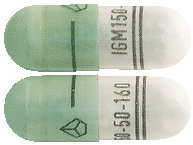
What it looks like
The pack contains a white plastic Breezhaler inhaler device together with capsules in blister cards.
ENERZAIR BREEZHALER registered pack sizes include:
- 114/46/68 micrograms
- 114/46/136 micrograms
Single pack containing 10 x 1 or 30 x 1 together with 1 inhaler.
Ingredients
ENERZAIR BREEZHALER contains the active ingredients: indacaterol acetate, glycopyrronium bromide (glycopyrrolate), and mometasone furoate.
Each capsule delivers:
114 micrograms of indacaterol,
46 micrograms of glycopyrronium,
68 or 136 micrograms of mometasone furoate, depending on which strength of Enerzair you have been given.
Enerzair capsules also contain:
- lactose monohydrate
- magnesium stearate
- hypromellose, purified water, carrageenan, potassium chloride (capsule shell)
This medicine does not contain sucrose, gluten, tartrazine or any other azo dyes.
Sponsor
ENERZAIR BREEZHALER is supplied in Australia by:
Novartis Pharmaceuticals Australia Pty Limited
ABN 18 004 244 160
54 Waterloo Road
Macquarie Park NSW 2113
Telephone: 1 800 671 203
Web site: www.novartis.com.au
® = Registered Trademark
This leaflet was prepared in December 2021.
Enerzair Breezhaler 114/46/68
AUST R 319002
Enerzair Breezhaler 114/46/136
AUST R 319001
(ene211221c based on PI ene211221i)
Published by MIMS August 2025