What is in this leaflet
This leaflet answers some common questions about Erlotinib ARX tablets. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Erlotinib ARX against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again
What Erlotinib ARX is used for
Erlotinib ARX contains the active ingredient erlotinib hydrochloride.
Erlotinib ARX is used for the treatment of non-small cell lung cancer (NSCLC).
It can be given before or after initial chemotherapy if your cancer has specific mutations in a protein called epidermal growth factor receptor (EGFR). It can also be given later on when initial chemotherapy has not worked.
Erlotinib ARX is also used in combination with gemcitabine for the treatment of pancreatic cancer.
Erlotinib ARX belongs to a group of medicines called anti-neoplastic (or anti-cancer) agents which are used to treat cancer.
Erlotinib ARX prevents the activity of the EGFR protein. This protein is known to be involved in the growth and spread of cancer cells.
Your doctor may have prescribed Erlotinib ARX for another purpose.
Ask your doctor if you have any questions about why Erlotinib ARX has been prescribed for you.
Erlotinib ARX is not addictive.
This medicine is available only with a doctor's prescription.
Before you take Erlotinib ARX
When you must not take it
Do not take Erlotinib ARX if:
- you have had an allergic reaction to erlotinib or any ingredients listed at the end of this leaflet
Some symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
- the package is torn or shows signs of tampering
- the expiry date (EXP) printed on the pack has passed
If you take this medicine after the expiry date has passed, it may not work as well.
If you are not sure if you should be taking Erlotinib ARX, talk to your doctor
Use in children
Do not give Erlotinib ARX to children. Safety and effectiveness in patients less than 18 years of age have not been established.
Use in elderly
Do not give Erlotinib ARX to children.
Reduction in dose is not required for elderly patients.
Before you start to take it
Your doctor must know about all the following before you start to take Erlotinib ARX.
Tell your doctor if:
- you are pregnant or plan to become pregnant.
Erlotinib ARX may be harmful to an unborn baby when taken by a pregnant woman. It is not recommended that you take Erlotinib ARX while you are pregnant.
If you are a woman who could become pregnant use adequate contraception during treatment, and for at least 2 weeks after taking the last tablet.
If you become pregnant while you are being treated with Erlotinib ARX, tell your doctor immediately.
- you are breast-feeding or plan to breast-feed.
It is not known whether Erlotinib ARX passes into breast milk. It is not recommended that you breastfeed while taking Erlotinib ARX and for at least 2 weeks after final dose.
If you have not told your doctor about any of the above, tell them before you start taking Erlotinib ARX.
- you have liver problems
It is not known whether Erlotinib ARX has a different effect if your liver is not functioning normally.
- you have kidney problems
- you have a history of stomach ulcers or inflammation of the bowel wall
- you are allergic to any other medicines, foods, dyes or preservatives
- you cannot tolerate lactose
If you have not told your doctor about any of the above, tell them before you start taking take Erlotinib ARX.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you have bought without a prescription from a pharmacy, supermarket or health food shop.
Some medicines interfere with Erlotinib ARX. These medicines include:
- medicines used to treat heartburn, indigestion and ulcers, such as antacids, H2 antagonists (e.g. ranitidine) and proton pump inhibitors (e.g. omeprazole)
- medicines used to treat HIV infection such as atazanavir, indinavir, ritonavir and saquinavir
- medicines used to treat epilepsy such as carbamazepine, phenobarbital (also known as phenobarbitone), phenytoin and midazolam
- medicines used to treat bacterial infections such as ciprofloxacin, clarithromycin, erythromycin, rifampicin and rifabutin
- corticosteroids, a group of medicines used to treat inflammation
- medicines used to treat fungal infections such as itraconazole, voriconazole and ketoconazole
- midazolam, a medicine used to cause drowsiness before an operation
- non-steroidal anti-inflammatory medicines (NSAIDs), medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis
- statins, a group of medicines used to lower cholesterol
- other medicines used to treat cancer
These medicines may be affected by Erlotinib ARX, or may affect how well it works. You may need to take different amounts of your medicine, or you may need to take different medicines. Your doctor will advise you.
There are some medicines that may still be taken with Erlotinib ARX but may require close supervision by your doctor. These medicines include:
- warfarin, a medicine used to prevent blood clots
Your doctor will need to regularly monitor you with blood tests.
Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking Erlotinib ARX.
How to take Erlotinib ARX
How much to take
Take Erlotinib ARX exactly as your doctor has prescribed.
Your doctor will tell you how many Erlotinib ARX tablets to take each day.
For non-small-cell lung cancer, the usual dose is one 150 mg tablet each day.
For pancreatic cancer, given in combination with gemcitabine, the usual dose is one 100 mg tablet each day.
How to take it
Swallow the tablets whole with a glass of water.
Do not chew the tablets.
When to take it
Take Erlotinib ARX tablets:
- at least 1 hour before you eat or
- at least 2 hours after you have eaten
Do not take Erlotinib ARX with food.
How long to take Erlotinib ARX
The duration of treatment with Erlotinib ARX varies, depending on the nature of your illness and your individual response to the treatment.
Continue taking Erlotinib ARX until your doctor tells you to stop.
If you forget to take it
Do not take an extra dose. Wait until the next dose and take your normal dose then.
Do not try to make up for the dose that you missed by taking more than one dose at a time.
If you are not sure what to do, ask your doctor or pharmacist.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (Australia telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much Erlotinib ARX. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep telephone numbers for these places handy.
If you are not sure what to do, contact your doctor or pharmacist.
While you are taking Erlotinib ARX
Things you must do:
Tell all doctors, dentists and pharmacists who are treating you that you are taking Erlotinib ARX.
Tell your doctor if you become pregnant while taking Erlotinib ARX.
Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed. Otherwise, your doctor may think that it was not effective and change your treatment unnecessarily.
Tell your doctor if you feel the tablets are not helping your condition.
Be sure to keep all of your appointments with your doctor so that your progress can be checked.
Things you must not do
Do not stop taking Erlotinib ARX or change the dose without first checking with your doctor.
Do not let yourself run out of medicine over the weekend or on holidays.
Do not give Erlotinib ARX to anyone else even if they have the same condition as you.
Do not take any other medicines whether they require a prescription or not without first telling your doctor or consulting with a pharmacist.
Smokers should stop smoking while taking Erlotinib ARX as blood levels of Erlotinib ARX may be reduced.
Things to be careful of
It is not known if Erlotinib ARX will affect your ability to drive or use machines.
Be careful driving or operating machinery until you know how Erlotinib ARX affects you.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Erlotinib ARX.
Erlotinib ARX helps people with non-small cell lung cancer and pancreatic cancer but it may have unwanted side effects.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- rash
- diarrhoea
your doctor may need to treat you with a medicine for this (e.g. loperamide) - tiredness
- loss of appetite
- weight loss
- difficulty in breathing
- cough
- infection
- nausea or vomiting
- dehydration. Signs of dehydration include dry skin, dark coloured urine, thirst, weakness or fatigue and loss of appetite
- stomach pain or discomfort or belching after eating
- itching
- dry skin
- acne
- tear in the skin
- folliculitis (infection of the hair roots)
- unusual hair loss or thinning
- conjunctivitis, discharge with itching of the eyes and crusty eyelid or swollen runny eyes
- irritation or feeling of having something in the eye
- inflammation of the eye, including pain or redness, sensitivity to light or reduced vision
- nose bleeds
- nail bed infection or swelling around the nails
- headache
- fever
- rigors or shaking
- depression
- numbness or weakness of the arms and legs
These are the more common side effects of Erlotinib ARX that you are likely to notice. Your doctor will tell you more about them. Your doctor may also recommend that you change the dose of Erlotinib ARX that you are taking if you experience any of the above side effects.
Tell your doctor immediately if you notice any of the following:
- mouth irritation, sore mouth, mouth ulcers or cold sores
- persistent cough
- infection, fever, chills
These may be serious side-effects. Your doctor may interrupt your Erlotinib ARX treatment.
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- shortness of breath or difficulty breathing with cough and/or fever.
- severe stomach pain or discomfort
- severe or persistent diarrhoea, nausea, vomiting or loss of appetite
- vomiting blood or material that looks like coffee grounds,
- bleeding from your back passage, black sticky bowel motions (stools), bloody diarrhoea
- tongue and/or facial swelling
- hives
- wheezing
- blisters on your skin, especially severe blisters and bleeding in the lips, eyes, mouth, nose and genitals
- painful red areas of skin, large blisters and/or peeling of layers of skin, accompanied by fever and chills, aching muscles and generally feeling unwell
- yellowing of the skin and eyes
- dark coloured urine
These may be very serious side effects. You may need urgent medical attention.
This is not a complete list of all possible side effects. Others may occur in some people and there may be some side effects not yet known.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell even if it is not on this list.
Ask your doctor or pharmacist if you don't understand anything in this list.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking Erlotinib ARX
Storage
Keep your tablets in their container until it is time to take them. If you take the tablets out of their container they may not keep well.
Keep Erlotinib ARX in a cool dry place where the temperature stays below 25°C.
Do not store it, or any other medicine, in a bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Keep Erlotinib ARX where young children cannot reach it. A locked cupboard at least one-and a- half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over. Do not throw out your medicine into the general household rubbish or flush it down the toilet.
Product description
Availability
Erlotinib ARX is available in three strengths, 25 mg, 100 mg and 150 mg.
Each tablet strength comes in packs of 30 tablets.
What Erlotinib ARX looks like
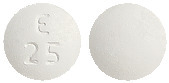
- Erlotinib ARX 25 mg film-coated tablets are white-coloured, round shaped, biconvex film-coated tablets, debossed with ‘E 25’ on one side and plain on the other side and free from physical defects.
- Erlotinib ARX 100 mg film-coated tablets are white coloured, round shaped, biconvex film-coated tablets debossed with ‘E 100’ on one side and plain on the other side and free from physical defects.
- Erlotinib ARX 150 mg film-coated tablets are white coloured, round shaped, biconvex film-coated tablets engraved with ‘E 150’ on one side and plain on the other side and free from physical defects.
Ingredients
Active ingredient
- Erlotinib hydrochloride
Inactive ingredients
- Lactose monohydrate
- microcrystalline cellulose
- sodium starch glycolate
- sodium lauryl sulfate
- magnesium stearate
The tablets have a film-coating which contains:
- hypromellose
- hyprolose
- propylene glycol
- titanium dioxide
Erlotinib ARX tablets are gluten free.
Sponsor
In Australia Erlotinib ARX is sponsored by:
Accelagen Pty Ltd
Suite 2.02
785 Toorak Road
Hawthorn East
Victoria 3123
Australia
This leaflet was prepared on January 2023.
Published by MIMS November 2025



 In two other double-blind, randomised, placebo-controlled Phase III studies (BO18192 and BO25460) conducted in a total of 1532 patients with advanced, recurrent or metastatic NSCLC following first-line standard platinum-based chemotherapy, no new safety signals were identified in the safety analysis population.
In two other double-blind, randomised, placebo-controlled Phase III studies (BO18192 and BO25460) conducted in a total of 1532 patients with advanced, recurrent or metastatic NSCLC following first-line standard platinum-based chemotherapy, no new safety signals were identified in the safety analysis population. In the open-label, randomised phase III study ML 20650, conducted in 154 patients, the safety of erlotinib for first-line treatment of NSCLC patients with EGFR activating mutations was assessed in 75 patients; no new safety signals were observed in these patients. The most frequent adverse reactions seen in patients treated with erlotinib in study ML 20650 were rash and diarrhoea (any Grade 80% and 57%, respectively), most were Grade 1 - 2 in severity and manageable without intervention. Grade 3 rash and diarrhoea occurred in 9% and 4% of patients, respectively. No Grade 4 rash or diarrhoea was observed. Both rash and diarrhoea resulted in discontinuation of erlotinib in 1% of patients. Dose modifications (interruptions or reductions) for rash and diarrhoea were needed in 11% and 7% of patients, respectively.
In the open-label, randomised phase III study ML 20650, conducted in 154 patients, the safety of erlotinib for first-line treatment of NSCLC patients with EGFR activating mutations was assessed in 75 patients; no new safety signals were observed in these patients. The most frequent adverse reactions seen in patients treated with erlotinib in study ML 20650 were rash and diarrhoea (any Grade 80% and 57%, respectively), most were Grade 1 - 2 in severity and manageable without intervention. Grade 3 rash and diarrhoea occurred in 9% and 4% of patients, respectively. No Grade 4 rash or diarrhoea was observed. Both rash and diarrhoea resulted in discontinuation of erlotinib in 1% of patients. Dose modifications (interruptions or reductions) for rash and diarrhoea were needed in 11% and 7% of patients, respectively.
 Survival was evaluated in the intent-to-treat population. The median overall survival improved by 42.5% and was 6.7 months in the erlotinib group compared with 4.7 months in the placebo group (see Figure 1). The primary survival analysis was adjusted for the stratification factors as reported at the time of randomisation (ECOG PS, best response to prior therapy, number of prior regimens and exposure to prior platinum) and HER1/EGFR status. In this primary analysis, the adjusted HR for death in the erlotinib group relative to the placebo group was 0.73 (95% CI: 0.60 - 0.87; p = 0.001). The percent of patients alive at 12 months was 31.2% and 21.5%, for the erlotinib and placebo groups respectively.
Survival was evaluated in the intent-to-treat population. The median overall survival improved by 42.5% and was 6.7 months in the erlotinib group compared with 4.7 months in the placebo group (see Figure 1). The primary survival analysis was adjusted for the stratification factors as reported at the time of randomisation (ECOG PS, best response to prior therapy, number of prior regimens and exposure to prior platinum) and HER1/EGFR status. In this primary analysis, the adjusted HR for death in the erlotinib group relative to the placebo group was 0.73 (95% CI: 0.60 - 0.87; p = 0.001). The percent of patients alive at 12 months was 31.2% and 21.5%, for the erlotinib and placebo groups respectively. The robustness of the overall survival result was examined in exploratory univariate analyses of a number of patient subsets formed according to stratification factors. The survival benefit with erlotinib treatment was seen across patient subsets including prior exposure to taxanes, smoking history, gender, age, histology, prior weight loss, time between initial diagnosis and randomisation and geographic location. The HR in the erlotinib group relative to the placebo group were less than 1.0, suggesting that the survival benefit from erlotinib was robust across subsets. Of note, the survival benefit of erlotinib was comparable in patients with a baseline ECOG PS of 2 - 3 (HR = 0.77) or a PS of 0 - 1 (HR = 0.73) and patients who had received one chemotherapy regimen (HR = 0.76) or two or more regimens (HR = 0.76).
The robustness of the overall survival result was examined in exploratory univariate analyses of a number of patient subsets formed according to stratification factors. The survival benefit with erlotinib treatment was seen across patient subsets including prior exposure to taxanes, smoking history, gender, age, histology, prior weight loss, time between initial diagnosis and randomisation and geographic location. The HR in the erlotinib group relative to the placebo group were less than 1.0, suggesting that the survival benefit from erlotinib was robust across subsets. Of note, the survival benefit of erlotinib was comparable in patients with a baseline ECOG PS of 2 - 3 (HR = 0.77) or a PS of 0 - 1 (HR = 0.73) and patients who had received one chemotherapy regimen (HR = 0.76) or two or more regimens (HR = 0.76). Symptom deterioration was measured using the EORTC QLQ-C30 and QLQ-LC13 quality of life questionnaires. Baseline scores of cough, dyspnoea and pain were similar in the two treatment groups. Erlotinib resulted in symptom benefits by significantly prolonging time to deterioration in cough (HR = 0.75), dyspnoea (HR = 0.72) and pain (HR = 0.77) versus placebo. These symptom benefits were not due to an increased use of palliative radiotherapy or concomitant medications in the erlotinib group.
Symptom deterioration was measured using the EORTC QLQ-C30 and QLQ-LC13 quality of life questionnaires. Baseline scores of cough, dyspnoea and pain were similar in the two treatment groups. Erlotinib resulted in symptom benefits by significantly prolonging time to deterioration in cough (HR = 0.75), dyspnoea (HR = 0.72) and pain (HR = 0.77) versus placebo. These symptom benefits were not due to an increased use of palliative radiotherapy or concomitant medications in the erlotinib group.
 The median PFS was 3.81 months (16.5 weeks) in the erlotinib group (95% CI; 3.58 - 4.93) compared with 3.55 months (15.2 weeks) in the placebo group (95% CI; 3.29 - 3.75; p = 0.006).
The median PFS was 3.81 months (16.5 weeks) in the erlotinib group (95% CI; 3.58 - 4.93) compared with 3.55 months (15.2 weeks) in the placebo group (95% CI; 3.29 - 3.75; p = 0.006). Erlotinib (erlotinib hydrochloride) is an epidermal growth factor receptor/human epidermal growth factor receptor type 1 (EGFR, also known as HER1) tyrosine kinase inhibitor. Erlotinib hydrochloride, the active ingredient of Erlotinib ARX, is a quinazolinamine with the chemical name N-(3-ethynylphenyl)-6,7- bis(2- methoxyethoxy)-4- quinazolinamine hydrochloride.
Erlotinib (erlotinib hydrochloride) is an epidermal growth factor receptor/human epidermal growth factor receptor type 1 (EGFR, also known as HER1) tyrosine kinase inhibitor. Erlotinib hydrochloride, the active ingredient of Erlotinib ARX, is a quinazolinamine with the chemical name N-(3-ethynylphenyl)-6,7- bis(2- methoxyethoxy)-4- quinazolinamine hydrochloride.