What is in this leaflet
This leaflet answers some common questions about FAMVIR® for Cold Sores.
It does not contain all the available information. It does not take the place of talking to your pharmacist or doctor.
The information in this leaflet was last updated on the date listed on the final page. Some more recent information on the medicine may be available.
You should speak to your pharmacist or doctor to obtain the most up to date information on the medicine.
You can also download the most up to date leaflet from www.novartis.com.au. Those updates may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your pharmacist or doctor has weighed the risks of you taking FAMVIR for Cold Sores against the benefits it can provide.
If you have any concerns about this medicine, ask your pharmacist or doctor.
Keep this leaflet with the medicine. You may need to read it again.
What FAMVIR for Cold Sores is used for
FAMVIR for Cold Sores is an antiviral medicine used to treat recurrent outbreaks of cold sores in adults 18 years of age and over who have a normal immune system (the body system which fights against harmful bacteria, viruses and fungi).
Cold sores are an infection caused by a virus called herpes simplex type 1 (HSV-1). The infection is most commonly acquired as a baby or child from contact with parents or relatives, often from kissing.
Cold sores usually begin on or around the lips, mouth, and nose as small red bumps that turn into fluid-filled blisters. Cold sores can be tender and painful. Many people who get cold sores know when one is coming by a tingling, burning, itchy or painful sensation or redness in the area. This can happen very rapidly.
After redness and swelling develop, blisters form. The blisters may weep or burst and this can be painful. Then a shallow ulcer and yellow crust form as the cold sore dries. The crust eventually falls off, exposing new pink-coloured skin. Generally the sores heal without scarring. After the initial infection has healed, the virus becomes dormant in nerve cells.
Cold sores can be unpredictable. The virus can become active again in the body, even after many years, resulting in recurrent outbreaks.
Even after many years, some people may experience recurring cold sores due to viral reactivation.
Some common triggers to a cold sore may include:
- sun exposure
- stress
- fatigue
- menstrual periods
- fever
- illness
- dry chapped lips
- skin trauma
- a cold.
Although FAMVIR for Cold Sores does not cure the viral infection, it helps to relieve the symptoms and shorten the duration of an outbreak.
The best results are obtained if the medicine is started as soon as possible after the onset of symptoms of a cold sore, such as tingling, itching or burning, or the appearance of the first signs, such as redness or swelling. This is when the virus is reproducing rapidly.
Ask your pharmacist or doctor if you have any questions about why this medicine has been recommended to you.
FAMVIR for Cold Sores is only available from your pharmacist and does not require a prescription. It is not addictive.
This medicine is not recommended for use in infants, children or adolescents under 18 years of age.
Before you take FAMVIR for Cold Sores
When you must not take it
Do not take FAMVIR for Cold Sores if you have a problem with your body's immune system, which helps to fight off infections. Your pharmacist will refer you to your doctor in that case.
Do not take FAMVIR for Cold Sores if you have an allergy to:
- famciclovir, the active ingredient
- penciclovir, a related antiviral medicine
- any of the other ingredients of FAMVIR for Cold Sores listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine after the expiry date printed on the pack, or if the packaging is torn or shows signs of tampering. In that case, return it to your pharmacist.
Before you start to take it
Tell your pharmacist or doctor if you are over 50 years of age, or if you have:
- a problem with your body's immune system, which helps to fight off infections
- a problem with your kidneys
- diabetes, high blood pressure, heart problems, liver problems or other medical conditions
- signs of an infection other than your cold sore.
Your pharmacist may want to take extra precautions or refer you to a doctor to determine if this medicine is suitable for you.
Tell your pharmacist or doctor if you are pregnant, intend to become pregnant or if you are breast-feeding.
FAMVIR for Cold Sores should not be used during pregnancy unless necessary. Your pharmacist or doctor will discuss with you the potential risks of taking FAMVIR for Cold Sores during pregnancy, and will also advise you if you should take FAMVIR for Cold Sores while breast-feeding, based on the benefits and risks of your personal situation.
Tell your pharmacist or doctor if you are allergic to any other medicines, foods, dyes or preservatives.
He/she will want to know if you are prone to allergies.
If you experience an allergic reaction, inform your pharmacist or doctor immediately.
Taking other medicines
Tell your pharmacist or doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines and FAMVIR for Cold Sores may interfere with each other. These include:
- probenecid, a prescription medicine used to treat gout (a disease with painful, swollen joints, caused by uric acid crystals) and to increase blood levels of penicillin-type antibiotics
- raloxifene, a medicine used to treat osteoporosis (a disease which causes bones to become less dense, gradually making them weaker, more brittle and likely to break)
- medicines that can affect your immune system
- medicines that can affect your kidneys.
You may need to take different amounts of these medicines or you may need to take different medicines. Your pharmacist and doctor have more information.
If you have not told your pharmacist or doctor about any of these things, tell him/her before you start taking this medicine.
How to take FAMVIR for Cold Sores
Follow all directions given to you by your pharmacist or doctor carefully. These instructions may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your pharmacist or doctor for help.
How much to take
The usual dose is three 500 mg tablets taken together as a single dose.
However, if you have problems with your kidneys and your pharmacist has referred you to your doctor to see if this medicine is suitable for you, your doctor may have recommended a different dose.
Ask your pharmacist or doctor if you are unsure of the correct dose for you. He/she will tell you exactly how much to take.
When to take it
Take FAMVIR for Cold Sores as soon as possible after the first symptoms (e.g. tingling, itching or burning) or signs (e.g. redness or swelling) of a cold sore appear.
Do not take the tablets if a hard crust has already formed on the cold sore.
Keep the tablets for the next episode.
How to take it
Swallow the tablets whole with a full glass of water.
They may be taken with or without food. It is not necessary to chew or crush the tablet.
How long to take it
A single dose of FAMVIR for Cold Sores is all that is necessary for treating each episode of cold sores. Each pack of FAMVIR for Cold Sores contains enough medicine for one dose. A repeat dose during this episode is not recommended. If another episode of cold sores recurs, another dose may be taken. However, treatment should not be repeated within 7 days.
If you take too much (Overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone number 13 11 26), or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much FAMVIR for Cold Sores. Show them your pack of tablets. Do this even if there are no signs of discomfort or poisoning. Keep the telephone numbers for these places handy.
Taking too much FAMVIR for Cold Sores may affect your kidneys. In people who already have kidney problems it may, rarely, lead to kidney failure if their dose is not correctly lowered.
While you are taking FAMVIR for Cold Sores
Things you must do
Tell your pharmacist or doctor if your cold sore symptoms do not improve within a few days, or if they become worse.
If you become pregnant while taking FAMVIR for Cold Sores, tell your pharmacist or doctor.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you periodically take this medicine to treat recurring episodes of cold sores.
Tell any other doctor, dentist or pharmacist who treats you that you periodically take this medicine.
Things you must not do
Do not take less than the recommended dose of 3 tablets, unless advised by your doctor.
Do not give this medicine to anyone else even if their condition seems to be the same as yours.
Do not use it to treat any other complaints unless your doctor tells you to.
Things to be careful of
If you are pregnant or breast-feeding, ask your doctor or pharmacist for advice before taking any medicine.
Be careful driving, operating machinery or doing jobs that require you to be alert until you know how FAMVIR for Cold Sores affects you.
This medicine can cause dizziness, sleepiness or confusion.
Things that may help your condition
Cold sores are contagious and the virus can be passed on from person to person through close physical contact or saliva, even when blisters are not present. The risk is much higher when the cold sore is visible, as the virus can be shed, making it easy to infect other people.
Take the following precautions to avoid spreading the virus:
- Keep the areas affected by the virus as clean and dry as possible
- Avoid touching or scratching the sore area as you may spread the virus on your fingers
- Do not share any objects that have been in contact with a cold sore (e.g. drinking glasses, eating utensils, or towels)
- Avoid direct skin-to-skin contact of the area with other people (e.g. kissing) until the cold sore has healed.
Side effects
Tell your pharmacist or doctor as soon as possible if you do not feel well while you are taking FAMVIR for Cold Sores.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by these lists of possible side effects. You may not experience any of them. Ask your pharmacist or doctor to answer any questions you may have.
Tell your pharmacist or doctor if you notice any of the following and they worry you:
- headache
- dizziness
- nausea (feeling sick) or vomiting
- abdominal pain
- diarrhoea
- itching or an itchy rash (urticaria)
The above side effects are usually mild.
Tell your pharmacist or doctor as soon as possible if you notice any of the following:
- a rash elsewhere on the body, that is separate from the cold sore
- extreme sleepiness or confusion, usually in older people
- hallucinations (seeing or hearing things that are not really there)
- painful or swollen joints
- aching muscles or muscle tenderness or weakness that is not caused by exercise.
- yellowing of the skin or eyes (signs of jaundice)
- palpitations (signs of abnormal heart beat)
The above side effects may need medical attention.
Tell your pharmacist or doctor immediately or go to Accident and Emergency at your nearest hospital if any of the following side effects happen:
- swelling below the surface of the skin (e.g. swelling around the face, eye, eyelid or throat)
- unexplained bruising, reddish or purplish patches on the skin or bleeding more easily than usual, as it may indicate that the number of platelets (a type of blood cell responsible for blood clotting) in your blood are reduced
- severe blistering of the skin or mucous membranes of the lips, eyes, mouth, nasal passages or genitals (signs of a serious skin reaction)
- purple patches, itching, burning of the skin (signs of inflamed blood vessels)
- seizures or fits
- difficulty breathing or swallowing, wheezing or cough, light-headedness, changes in alertness, skin reddening, facial/throat swelling, blue discoloration of the lips, tongue or skin (signs of severe allergic reaction).
The above side effects are very rare.
Tell your pharmacist or doctor if you notice anything else that is making you feel unwell. Other side effects not listed here or not yet known may happen in some people.
After using FAMVIR for Cold Sores
Storage
Keep your medicine in the original container until it is time to take it.
Store your tablets in a dry place where the temperature stays below 30°C.
Do not store your medicines in the bathroom or near a sink.
Do not leave the tablets in the car or on window sills. Heat and dampness can destroy some medicines. FAMVIR for Cold Sores tablets will keep best if they are stored cool and dry.
Keep the medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your pharmacist or doctor recommended that you take less than the full dose in this pack, ask your pharmacist what to do with any tablets that you may have left over.
Product description
What it looks like
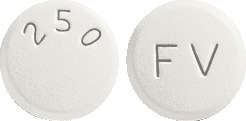
FAMVIR for Cold Sores are white, oval, film-coated tablets with "FV 500" on one side. Each carton contains 3 tablets in a blister pack with 'FAMVIR famciclovir 500mg' printed on the foil backing.
Ingredients
FAMVIR for Cold Sores contain 500 mg famciclovir per tablet as the active ingredient. Each tablet also contains the following inactive ingredients:
- hypromellose
- hydroxypropylcellulose
- macrogol
- magnesium stearate
- sodium starch glycollate
- titanium dioxide
The tablets do not contain lactose, sucrose, gluten, tartrazine or any other azo dyes.
Sponsor
FAMVIR for Cold Sores is supplied in Australia by:
NOVARTIS Pharmaceuticals Australia Pty Limited
ABN 18 004 244 160
54 Waterloo Road
Macquarie Park NSW 2113
Telephone 1 800 671 203
Web site: www.novartis.com.au
® = Registered Trademark
This leaflet was prepared in August 2016
Australian Registration Number
FAMVIR for Cold Sores AUST R 201264
(famcs160816c.doc) based on PI (fam160816i.doc)
Published by MIMS February 2017







 As these recommendations are not based on repeated dose data, patients with impaired renal function should be closely monitored for adverse effects. There are insufficient data to recommend a dosage for patients with creatinine clearance less than 10 mL/min/1.73 m2.
As these recommendations are not based on repeated dose data, patients with impaired renal function should be closely monitored for adverse effects. There are insufficient data to recommend a dosage for patients with creatinine clearance less than 10 mL/min/1.73 m2.



 Famciclovir has also been well tolerated in immunocompromised patients. Adverse effects reported from clinical studies were similar to those reported in the immunocompetent population.
Famciclovir has also been well tolerated in immunocompromised patients. Adverse effects reported from clinical studies were similar to those reported in the immunocompetent population.
 Plasma concentration time curves of penciclovir are similar following single and repeat (b.i.d. and t.i.d.) dosing and there is no accumulation of penciclovir on repeated dosing. Penciclovir and its 6-deoxy precursor are poorly (< 20%) bound to plasma proteins.
Plasma concentration time curves of penciclovir are similar following single and repeat (b.i.d. and t.i.d.) dosing and there is no accumulation of penciclovir on repeated dosing. Penciclovir and its 6-deoxy precursor are poorly (< 20%) bound to plasma proteins.
