What is in this leaflet
This leaflet answers some common questions about FINNACAR.
It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking FINNACAR against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What FINNACAR is used for
FINNACAR is for use in men only. It must not be taken by women.
FINNACAR is used to treat benign prostatic hyperplasia (BPH). BPH is a condition where your prostate gland (which is near your bladder) has become bigger making it difficult to pass urine. This can cause symptoms such as:
- a weak or interrupted stream of urine
- the feeling that you cannot completely empty your bladder
- a delay before you start to pass urine
- the need to pass urine often, especially at night
- the urgent feeling that you need to pass urine right away.
BPH occurs only in men and is common over the age of 50 years. In some men, BPH can lead to serious problems, including urinary tract infections and the sudden inability to pass urine at all. BPH can also lead to the need for surgery such as procedures to improve the flow of urine.
The prostate gland takes years to grow so the symptoms of BPH can take a long time to develop.
FINNACAR works by slowly reducing the size of your prostate gland. This may lead to gradual improvement in your urine flow and other symptoms over several months. FINNACAR also helps reduce the risk of developing a sudden inability to pass urine (acute urinary retention) and the need for surgery. This may happen whether or not you notice any improvement or change in your symptoms.
Your doctor may have prescribed FINNACAR for another reason. Ask your doctor if you have any questions about why FINNACAR has been prescribed for you.
FINNACAR is available only with a doctor's prescription.
FINNACAR is not addictive.
Before you take it
When you must not take it
Do not take FINNACAR if you are allergic to medicines containing finasteride or any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include skin rash or swelling of the lips or face.
Do not take FINNACAR if the expiry date (Exp.) printed on the pack has passed.
Do not take FINNACAR if the packaging is torn or shows signs of tampering.
Women who are pregnant must not take FINNACAR or handle crushed or broken tablets. If the active ingredient in FINNACAR is absorbed after swallowing the tablet or through the skin by a woman who is pregnant with a male baby, it may cause the male baby to be born with abnormalities of the sex organs. The tablets are coated and will prevent contact with the active ingredient during normal handling, provided the tablets are not broken or crushed.
If a pregnant woman swallows FINNACAR or handles crushed or broken tablets, her doctor must be consulted immediately.
Do not give your medicine to children or women. The condition for which this medicine is prescribed occurs only in men.
Before you start to take it
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have any medical conditions.
If you have not told your doctor about any of the above, tell them before you start taking FINNACAR.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines affect how other medicines work. FINNACAR has not been shown to interfere with other medicines.
How to take it
How much to take
The usual dose is one tablet taken once a day.
Follow all directions given to you by your doctor and pharmacist carefully.
How to take FINNACAR
Swallow the tablets with a glass of water.
This medicine can be taken before or after food.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember, and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
How long to take FINNACAR for
FINNACAR shrinks the prostate gland slowly. Therefore, you may need to take this medicine for 6 months or longer to see whether it helps you.
If it does help your symptoms, you may need to take it every day.
Continue taking it for as long as your doctor recommends. If you stop taking the medicine the prostate gland is likely to grow again.
If you take too much (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at the nearest hospital, if you think you or anyone else may have taken too much FINNACAR. Do this even if there are no signs of discomfort or poisoning.
While you are taking it
Things you must do
Visit your doctor regularly so they can check on your progress and conduct a physical check for prostate cancer once a year when you are over 50.
While BPH is not cancer and does not lead to cancer, the two conditions can exist at the same time. FINNACAR is used to treat BPH, not prostate cancer.
If you have to have a blood test to measure your SA (prostate specific antigen) levels, tell your doctor that you are taking FINNACAR. FINNACAR can affect the results of some tests.
Before starting any new medicine, tell your doctor or pharmacist that you are taking FINNACAR.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking FINNACAR.
Things you must not do
Do not use FINNACAR to treat any other conditions unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking FINNACAR.
Like all other medicines, FINNACAR may have unwanted side effects in some people. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- impotence (inability to have an erection)
- less desire for sex
- changes or problems with ejaculation, such as a decreased amount of semen released (this decrease does not appear to interfere with normal function).
These are the more common side effects of FINNACAR. For the most part these have been mild. In some cases, these side effects disappeared while the patient continued to take this medicine. If symptoms persisted, they are usually resolved on stopping the tablets.
Tell your doctor immediately if you notice any of the following:
- breast swelling and/or tenderness
- breast lumps, pain or discharge from the nipples
- skin rash, itchiness
- hives or nettlerash (pinkish, itchy swellings on the skin)
- testicle pain
- irregular heart beats
- increased liver enzyme laboratory results
- blood in semen
- depressions (feelings of severe sadness and unworthiness) including suicidal thoughts
Tell your doctor immediately or go to Accident and Emergency at the nearest hospital if you notice any of the following:
- swelling of the lips or face
- male breast cancer
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything that is making you feel unwell.
After using it
Storage
Keep FINNACAR where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store FINNACAR or any other medicine in the bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking FINNACAR, or your tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
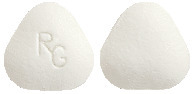
FINNACAR is a rounded triangle white tablet marked RG on one side.
Each pack contains 30 tablets.
Ingredients
The active ingredient in FINNACAR is finasteride. Each tablet contains 5 mg of finasteride.
The tablets also contain:
- lactose monohydrate
- microcrystalline cellulose
- pregelatinised maize starch
- sodium starch glycollate
- purified talc
- magnesium stearate
- hyprolose
- hypromellose
- macrogol 6000
- titanium dioxide.
Contains sugars as lactose.
The tablets do not contain gluten, sucrose, tartrazine or any other azo dyes.
Supplier
Arrotex Pharmaceuticals
15-17 Chapel Street
Cremorne VIC 3121
Australia
Ph: 1800 195 055
Australian registration number:
AUST R 143402
This leaflet was revised in October 2022
Published by MIMS November 2022



 C23H36N2O2. Molecular weight: 372.5.
C23H36N2O2. Molecular weight: 372.5.