What is in this leaflet
This leaflet answers some common questions about GyMiso® tablets. It does not contain all the available information. It does not take the place of talking to your doctor.
All medicines have risks and benefits. Your doctor has weighed the risks of you being given GyMiso® tablets against the expected benefits it will have for you.
If you have any concerns about being given this medicine, ask your doctor.
Keep this leaflet. You may need to read it again.
What GyMiso® is used for
GyMiso® contains misoprostol. It belongs to a group of medicines called prostaglandins. It acts like prostaglandin E1. GyMiso® induces contractions of the smooth muscle and relaxation of the cervix. These properties help open the cervix and push out the contents of the uterus.
GyMiso® can therefore be used to terminate a pregnancy.
GyMiso® is recommended for the medical termination of pregnancy. It is recommended for use up to 49 days after your last menstrual period. It is given in combination with another medicine called mifepristone, which blocks progesterone, a hormone that is needed for pregnancy to continue.
Ask your doctor if you have any questions about why GyMiso® has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is available only with a doctor’s prescription.
Before you are given GyMiso®
When you must not be given it
You should not be given GyMiso® if:
- you are pregnant and wish to carry your pregnancy to term
- you have any allergies to misoprostol, or any other prostaglandins or any of the other ingredients listed at the end of this leaflet
You should not be given a mifepristone tablet and GyMiso® tablets if:
- you cannot take mifepristone or have any allergies to mifepristone
- you suffer from chronic adrenal failure
- you suffer from severe disease where it is necessary to take steroids (e.g. asthma uncontrolled by treatment)
- you have known or suspected hypocoagulation diseases
- you are on anticoagulant therapy
You should not be given a mifepristone tablet and GyMiso® tablets for termination of pregnancy up to 49 days since your last period if:
- your pregnancy has not been confirmed by a pregnancy test or an ultrasound scan
- the first day of your last period was more than 49 days ago
- your doctor suspects an ectopic pregnancy (the egg is implanted outside the womb)
You should not use this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If this medicine is used after the expiry date it may not work as well.
If you are under 18 years of age, you should only take GyMiso® if advised to do so by your doctor. There is limited information on the use of GyMiso® in adolescents less than 18 years of age.
If you are not sure whether you should be given this medicine, talk to your doctor.
Before you take GyMiso®
Tell your doctor if you have allergies to any other medicines, foods preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- heart or cardiovascular disease
- epilepsy
- asthma
- kidney problems
- liver problems
- malnutrition
- problems with your adrenal glands
- anaemia
- blood disorders which lead to difficulty in clotting
- if you are taking anticoagulants
- if you are taking corticosteroids including inhaled corticosteroids for the treatment of asthma
- if you have an intra-uterine device (IUD), as this needs to be removed.
If you have not told your doctor about any of the above, tell him/her before you take mifepristone and GyMiso®.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket, health food shop, naturopath or herbalist. Some medicines and GyMiso® may interfere with each other.
Different medicines may be affected by GyMiso®, or may affect how well it works. You may need to be given different amounts of your medicines, or you may need to be given different medicines.
Your doctor and pharmacist may have more information on medicines to be careful with or avoid while being treated with GyMiso®.
How GyMiso® is given
How much to take
Your doctor will tell you how many tablets you need to take and when to take them.
GyMiso® is usually taken 36 to 48 hours after you have taken mifepristone.. You will need to take four GyMiso® tablets (misoprostol 800 micrograms). These are taken either as four tablets in one dose, or as two tablets followed two hours later by another two tablets.
How to take GyMiso®
GyMiso® should be swallowed with water.
GyMiso® can also be taken by holding the tablet in your mouth, between the cheek and gum, for 30 minutes before swallowing any fragments with water.
It is recommended that GyMiso® should be taken on an empty stomach - 2 hours before or after a meal.
After you take GyMiso® tablets, you should stay at home and rest for 3 hours. Vaginal bleeding will occur and the pregnancy may be expelled within a few hours of taking GyMiso® or during the next few days. The bleeding lasts on average for 10 to 16 days and may be heavy.
It is very important that you have follow up with your doctor 14 to 21 days after you take mifepristone and GyMiso®, to ensure that the termination was complete, because incomplete termination will increase the risk of serious infection or bleeding.
It is recommended that you do not travel away from home during the time that you are bleeding so that you can visit your doctor or clinic if necessary.
In case of heavy and prolonged bleeding, you should contact your doctor immediately in order to schedule an appointment.
In rare cases, a termination can occur after you take mifepristone but before you take GyMiso®. It is essential that you are checked to confirm that a complete termination has occurred. If this occurs, you should contact your doctor immediately in order to schedule an appointment.
If you forget to take your dose of GyMiso®
Contact your doctor immediately if you forget to take GyMiso® tablets and it is greater than 48 hours after you have taken a mifepristone 200 mg tablet.
If you are given too much (overdose)
GyMiso® is given to you by your doctor. An overdose is not likely to occur. Ask your doctor if you have any concerns.
While you are being given GyMiso®
Things you must do
If you are pregnant
In some cases treatment with mifepristone and GyMiso® may not result in a termination of pregnancy.
You must keep all of your doctor’s appointments so that your progress can be checked. This is very important.
If treatment with mifepristone and GyMiso® does not work, a termination can be arranged using another method.
If treatment with mifepristone and GyMiso® does not work and you wish to keep your pregnancy, it is not known if mifepristone can cause harm to your baby. It is believed, though, that GyMiso® can cause harm to your baby. You need to tell your doctor or nurse about mifepristone and GyMiso® so that they can carefully monitor your pregnancy.
If you are Rhesus negative, the use of mifepristone and GyMiso® requires that your doctor will take measures to prevent Rhesus factor sensitization, along with the general measures taken during any pregnancy termination.
If you are breastfeeding
GyMiso® should not be taken if you are breastfeeding.
If you are taking other medicines
If you are about to be started on any new medicines, remind your doctor or pharmacist that you have recently been given mifepristone and GyMiso®. Ask your doctor or pharmacist for advice before taking any medicine.
Tell any other doctors, dentists, and pharmacists who treat you that you have recently been given these medicines.
If you plan to become pregnant, tell your doctor that you have been given this medicine. Your doctor can discuss with you the risks and benefits involved.
Side effects
Tell your doctor or nurse as soon as possible if you do not feel well while you are being given mifepristone and GyMiso®.
Do not be alarmed by the following list of side effects, you may not experience any of them.
Tell your doctor if you notice any of the following and they worry you:
- headache
- vaginal bleeding which may be heavy or prolonged
- spotting
- cramps
- breast tenderness
- fainting
- hot flushes, skin rashes or itching
- side effects related to GyMiso® such as nausea, vomiting, diarrhoea, dizziness, abdominal discomfort, abdominal pain, cramps, fatigue and chills and/or fever.
Tell your doctor if you notice anything that is making you feel unwell.
Infection
Serious infections are very rare in a medical termination of pregnancy and can be potentially life threatening. If you have symptoms occurring more than 24 hours after taking misoprostol of ongoing abdominal pain, or feeling unwell, or feeling weak, with or without a fever you should contact your doctor without delay.
Bleeding
Vaginal bleeding usually starts a few hours after taking misoprostol tablets. Bleeding can occur for 10 to 16 days and it is usual for bleeding to be heavier than a normal period for 2 to 3 days. Contact your doctor immediately if you find you have very heavy bleeding and have soaked more than 2 pads per hour over 2 hours.
Other side effects not listed above may also occur in some people.
After being given GyMiso®
Storage
GyMiso® should be kept in a cool, dry place where the temperature stays below 25 degrees C. Store GyMiso® in the original packaging.
Keep GyMiso® where children cannot reach it.
GyMiso® should not be used after the expiry date printed on the pack. If this medicine is used after the expiry date it may not work as well.
Disposal
Any GyMiso® which is not used will be disposed of in a safe manner by your doctor or pharmacist.
Using contraceptives
It is possible for you to become pregnant again immediately after the pregnancy termination is completed. As some effects of mifepristone and GyMiso® may still be present, it is recommended that you avoid getting pregnant again before your next menstrual period after taking these medicines.
Product description
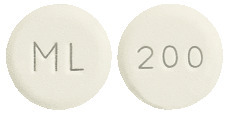
What it looks like
GyMiso® is presented in a box containing a blister pack of 4 white, round, flat tablets with ML on one side and 200 on the other. Each tablet contains 200 micrograms of misoprostol.
Ingredients
GyMiso® contains the active ingredient misoprostol plus hypromellose, microcrystalline cellulose, sodium starch glycollate, and hydrogenated castor oil.
The tablets do not contain gluten, lactose, tartrazine or any azo dyes.
Supplier
GyMiso® is supplied in Australia by:
MS Health
Suite 129, 135 Cardigan Street, Carlton
VIC 3053, Australia
MS Health Nurse After-care Telephone Service: 1300 515 883 (24 hours)
Licensed from Linepharma (France)
Australian registration number:
AUST R 188015
This leaflet was prepared on 21 January 2013.
Copyright. All rights reserved.
Published by MIMS August 2013


 Adverse events reported with mifepristone, classified as uncommon (≥ 1/1000 to < 1/100) are summarized as shown below.
Adverse events reported with mifepristone, classified as uncommon (≥ 1/1000 to < 1/100) are summarized as shown below.