What is in this leaflet
This leaflet answers some of the common questions about Invega. It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
If you have any concerns about using Invega, ask your doctor or pharmacist. Your doctor and pharmacist have more information.
Keep this leaflet with your medicine. You may need to read it again.
What Invega is used for
Invega belongs to a group of medicines called antipsychotic agents which improve the symptoms of certain types of mental illness.
It is used to treat symptoms of schizophrenia, a mental illness with disturbances in thinking, feelings and behaviour. It is also used to treat other types of related psychoses. Invega helps to correct a chemical imbalance in the brain associated with these conditions.
Invega tablets are formulated with a special shell that controls the release of the active ingredient gradually throughout the day. The tablet shell does not dissolve completely after all the drug has been released and sometimes the tablet shell may be seen in your stool. This is normal.
Your doctor, however, may prescribe this medicine for another use.
Ask your doctor if you have any questions about why it has been prescribed to you.
Invega is not addictive.
Before you take it
When you must not take it
Do not take Invega if you know you are allergic to any of its ingredients listed at the end of this leaflet or medicines containing risperidone (e.g. RISPERDAL). Signs of allergy may include skin rash, itching, shortness of breath, and/or swollen face or tongue.
Do not take it after the expiry date printed on the pack. If you take it after the expiry date has passed, it may not work as well.
Do not take it if the packaging is torn or shows signs of being tampered with.
Do not take it if the tablets appearance has changed.
Do not take it to treat any other complaints unless your doctor says it is safe to do so.
Before you start to take it
Invega should be used with caution in some people, particularly those who have been diagnosed with more than one medical condition.
- Before you start taking Invega, make sure you tell your doctor if you have, or have ever had, the following:
- Neuroleptic Malignant Syndrome (a serious reaction to some medicines that causes a sudden increase in body temperature, very fast heartbeat, extremely high or low blood pressure and severe muscle stiffness or fits)
- Tardive dyskinesia (a reaction to some medicines with involuntary movements of the tongue, face, mouth, jaws, arms, legs or trunk)
- irregular heart rhythm, high or low blood pressure or you've had a heart attack or stroke in the past
- you are prone to dizziness when standing up from a lying or sitting position
- unusual, excessive sweating or diarrhoea, dehydration or problems with your body temperature regulation
- epilepsy, fits, seizures
- involuntary movements or unusual restlessness or difficulty sitting still
- Parkinson's Disease (a progressive movement and thinking disorder that tends to affect older people)
- suicidal thoughts or past suicide attempts
- inflammation of the lungs due to aspiration (the inhalation of food particles or fluids into the lungs).
- any problems with swallowing, or stomach or intestinal disorders that reduces your ability to keep food down and/or pass normal bowel movements
- kidney or liver problems
- any problems with confusion or unsteadiness
- dementia or Lewy body dementia.
Older people suffering dementia may be at an increased risk of stroke or death with Invega. - Sugar diabetes
- unusual thirst, tiredness, blurred vision, upset stomach or need to urinate - common signs of high blood sugars
- stroke or other brain blood vessel problems
- continuous and/or painful erections (called 'priapism')
- low white blood cell count
If you have low numbers of some white blood cells, your risk of contracting an infection or developing a fever is increased with Invega. - blood clots
Tell your doctor if you or someone else in your family has a history of blood clots. Blood clots in the lungs and legs can occur with Invega. Blood clots in the lungs can result in death.
- Tell your doctor if:
- you have any eye surgery planned.
Your doctor will need to assess whether you are at increased risk of a surgical complication (called 'Intraoperative Floppy Iris Syndrome'. You may be recommended to stop Invega temporarily leading up to your eye surgery - you are pregnant or are planning to become pregnant.
Your doctor will advise you whether you should take Invega.
Newborn babies of mothers taking Invega in their last trimester may be at risk of having difficulty feeding or breathing, shaking, muscle stiffness and/or weakness, sleepiness or agitation. - you are breast feeding.
As Invega is excreted in breast milk. It is recommended that you do not breast-feed while taking it.
- Other medicines and alcohol
You should not drink alcohol while taking Invega.
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
In particular tell your doctor if you are taking:
- sleeping tablets, tranquillisers, pain-killers, or some allergy medications called antihistamines
- medicines to treat epilepsy
- medicines to treat depression, panic disorder, anxiety or obsessive-compulsive disorder
- medicines that increase the activity of the central nervous system (psychostimulants such as methylphenidate)
- any medicines to treat irregular heart rhythms or heart failure
- any medicines to treat high blood pressure, including water tablets (diuretics)
- other medicines to treat mental illnesses or psychotic conditions
- medicines to relieve nausea or vomiting, indigestion, reflux or other stomach problems
- some medicines to treat malaria.
Your doctor will need to consider whether any of the above medicines will affect your Invega.
- Older People
Your doctor may adjust your dose based on your kidney function.
Taking it for the first time
At the start of treatment you may have a fall in blood pressure making you feel dizzy on standing up, or your heart may beat faster. These should go away after a few days. Tell your doctor if these symptoms continue or worry you.
How to take it
Your doctor will decide the Invega strength and dose most suitable for you.
Invega should be taken once daily, in the morning, at about the same time each day.
You should decide whether you will always take Invega on an empty stomach before breakfast, or always with food at breakfast. You must not switch between taking Invega on an empty stomach and taking it with food.
The tablet should be swallowed whole with water or other liquid. Invega tablets must not be chewed, split or crushed.
Your doctor will decide the dose of Invega that is suitable for you, based on your condition and kidney function.
The usual dosage for Invega is between 3 mg and 12 mg once daily.
For people with severe kidney problems the starting dose may be as low as 3 mg every other day. Your doctor may later decide to increase the dose as required for best symptoms control.
Follow your doctor's instructions carefully and do not change or stop your dosage without consulting your doctor first.
Invega is not recommended for children under 18 years.
If you forget to take it
- If you forget to take it, take the missed dose as soon as you remember. Then resume taking Invega as you normally would the following morning.
- Do not take a double dose to make up for the one you missed.
- If you forget to take it for a number of days or more, tell your doctor before starting your medicine again.
If you have problems remembering when to take your medicine, ask your pharmacist for some hints.
Overdose
If you think you or anybody else has taken too much Invega, contact your doctor, pharmacist or the Poisons Information Centre who will advise you what to do.
You can contact the Poisons Information Centre by dialling:
- Australia: 13 11 26
- New Zealand: 0800 POISON or 0800 764 766
Signs of overdose may include drowsiness, dizziness, sleepiness, excessive trembling, nausea, excessive muscle stiffness, increased heart rate, shortness of breath, very low blood pressure causing fainting or unconsciousness.
While you are using it
Things you must do
Follow your doctor's instructions carefully.
Always seek your doctor's advice before changing or stopping treatment. Your doctor will be happy to discuss any questions you may have with your treatment.
Tell your doctor if you are pregnant or planning to become pregnant.
Tell your doctor immediately if you notice any involuntary movements of the tongue, mouth, cheeks or jaw. These may be symptoms of a condition called tardive dyskinesia, which can develop in people taking antipsychotic medicines, including Invega. This condition is more likely to occur during longer term treatment and in older women. In very rare cases, these symptoms may be permanent. However, if detected early, these symptoms are usually reversible.
If any doctors, dentists or pharmacists want to start you on any new medicines listed under point 3 of 'Before you start to take it' (above), tell them you are taking Invega. Your doctor, dentist or pharmacist will need to consider whether any new medicines will affect your Invega.
Things you must not do
Do not use Invega to treat any other complaint unless your doctor says so.
Do not give this medicine to anyone else, even if their symptoms seem similar.
Do not change your dose or stop taking Invega without first checking with your doctor.
Do not drink alcohol. Invega can increase the effects of alcohol.
Things to be careful of
Ask your doctor before taking any other medicines.
Invega can increase the effects of medicines which slow your reactions. Always ask your doctor or pharmacist before taking other medicines including herbal treatments and medicines that can be bought in a pharmacy or supermarket.
Avoid driving or operating machinery until you are sure that Invega does not affect your alertness. Invega may cause dizziness, drowsiness or light-headedness in some people, especially after the first dose. Make sure you know how you react to Invega before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy.
Avoid excessive eating. There is a possibility of weight gain when taking Invega. Your doctor may monitor your body weight or recommend strategies to assist with weight management.
Side Effects
All medicines may have some unwanted side effects. Sometimes they are serious, but most of the time they are not. Your doctor has weighed the risks of using this medicine against the benefits they expect it will have for you.
All medicines can have side effects. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Invega.
It helps most people with symptoms of schizophrenia or other types of related psychoses, but it may have unwanted side effects in a few people.
Tell your doctor if you notice any of the following and they worry you:
- difficulty thinking, working or carrying out your usual daily activities because of:
- nausea
- headache
- trembling, muscle weakness, unsteadiness on your feet or lack of coordination
- sleeplessness, drowsiness, tiredness, lack of energy or difficulty in concentrating - behavioural changes such as:
- unexplained confusion or agitation
- unusual anxiety or depression
- elated mood
- lack of emotion - joint or movement changes such as:
- muscle tightness or stiffness, writhing movements, spasm or muscle pain
- unusual restlessness, repetitive or involuntary movements
- unusual facial movements or a sustained upwards stare - other changes such as:
- unexplained increased appetite or weight gain
- diarrhoea, indigestion, heartburn, abdominal pain, constipation
- "flu-like" symptoms, cough, stuffy nose
- inability to or pain when passing urine
- dry mouth, distorted taste sensation, unexplained salivation or drooling
- acne
- dry skin
- reddening or discolouration of skin
- nose bleeds
- unusual thirst, tiredness, upset stomach or need to urinate
- unusual secretion of breast milk, breast swelling, missed or irregular menstrual periods
- decreased libido
- difficulty getting or maintaining an erection; or having continuous and/or painful erections
These are mild side effects of Invega but may require medical attention.
Tell your doctor immediately, or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- Signs of heart or blood pressure problems including:
- fainting, blurry vision, light-headedness or dizziness, particularly on standing, that persists despite sitting or lying down
- very fast heart rate or heart rhythm irregularities - signs of high blood sugar or diabetes such as:
- unusual thirst, tiredness, upset stomach or need to urinate more often than usual - body temperature changes such as:
- fever
- unexplained high body temperature, excessive sweating or rapid breathing - involuntary movement of the tongue, mouth, cheeks or jaw
- severe or life-threatening rash with blisters and peeling skin that may start in and around the mouth, nose, eyes, and genitals and spread to other areas of the body (Stevens-Johnson syndrome or toxic epidermal necrolysis).
These may be serious side effects of Invega. You may need urgent medical attention.
Serious side effects are uncommon.
If any of the following happen, stop taking Invega and tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- rash, itching or hives on the skin; shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body. If you have them, you may have had a serious allergic reaction to Invega
- sudden weakness or numbness of the face, arms, or legs, especially on one side, or instances of slurred speech (these are called mini-strokes)
These are very serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some people.
Do not hesitate to report any other side effects to your doctor or pharmacist.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After using it
Storage
Keep the tablets in a dry place where the temperature stays below 25°C.
Do not store it or any medicines in the bathroom or near a sink. Heat and dampness can destroy some medicines.
Keep it where young children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Do not use it beyond the expiry date (month and year) printed on the pack. Medicines cannot be stored indefinitely, even if stored properly.
Disposal
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
Product Description
What it looks like
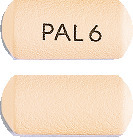
You can identify Invega tablets by their colour and shape. This is important because each type of tablets, contains a different amount of the active paliperidone:
- 3 mg: White, capsule shaped tablets imprinted with "PAL 3".
- 6 mg: Beige, capsule shaped tablets imprinted with "PAL 6".
- 9 mg: Pink, capsule shaped tablets imprinted with "PAL 9".
All tablets come in blister packs of 28 tablets.
Ingredients
The active ingredient in Invega is paliperidone.
The tablets contain either 3 mg, 6 mg or 9 mg of paliperidone.
Inactive ingredients are carnauba wax, cellulose acetate, hyetellose, macrogol, polyethylene oxide, povidone, sodium chloride, stearic acid, butylated hydroxytoluene, hypromellose, titanium dioxide, and iron oxides. The 3 mg tablets also contain lactose monohydrate and triacetin.
Sponsor
Janssen-Cilag Pty Ltd
1-5 Khartoum Road
Macquarie Park NSW 2113
Telephone: 1800 226 334
NZ Office: Auckland New Zealand
Telephone: 0800 800 806
Registration Numbers
3 mg prolonged release tablet blister pack - AUST R 130502
6 mg prolonged release tablet blister pack - AUST R 130714
9 mg prolonged release tablet blister pack - AUST R 130717
This leaflet was prepared in July 2020.
Published by MIMS October 2020





 ADRs reported with paliperidone and/or risperidone by < 2% of Invega-treated subjects in a pooled dataset of the 9 double blind, placebo controlled schizophrenia, schizoaffective disorder, and other unapproved indication trials are shown in Table 4.
ADRs reported with paliperidone and/or risperidone by < 2% of Invega-treated subjects in a pooled dataset of the 9 double blind, placebo controlled schizophrenia, schizoaffective disorder, and other unapproved indication trials are shown in Table 4. ADRs reported with paliperidone and/or risperidone in other clinical trials but not reported by Invega (3-12 mg) treated subjects in a pooled dataset of the 9 double blind, placebo controlled schizophrenia, schizoaffective disorder, and other unapproved indication trials are shown in Table 5.
ADRs reported with paliperidone and/or risperidone in other clinical trials but not reported by Invega (3-12 mg) treated subjects in a pooled dataset of the 9 double blind, placebo controlled schizophrenia, schizoaffective disorder, and other unapproved indication trials are shown in Table 5.

 Table 8 shows the EPS data from the pooled schizoaffective disorder trials.
Table 8 shows the EPS data from the pooled schizoaffective disorder trials. Compared to data from the studies in schizophrenia, pooled data from the two placebo controlled 6 week studies in subjects with schizoaffective disorder showed similar types and frequencies of EPS as measured by rating scales, anticholinergic medication use, and spontaneous reports of EPS related adverse events. For subjects with schizoaffective disorder, there was no dose related increase in EPS observed for Parkinsonism with the Simpson-Angus scale or akathisia with the Barnes Akathisia Rating Scale. There was a dose related increase observed with spontaneous EPS reports of hyperkinesia and dystonia and in the use of anticholinergic medications.
Compared to data from the studies in schizophrenia, pooled data from the two placebo controlled 6 week studies in subjects with schizoaffective disorder showed similar types and frequencies of EPS as measured by rating scales, anticholinergic medication use, and spontaneous reports of EPS related adverse events. For subjects with schizoaffective disorder, there was no dose related increase in EPS observed for Parkinsonism with the Simpson-Angus scale or akathisia with the Barnes Akathisia Rating Scale. There was a dose related increase observed with spontaneous EPS reports of hyperkinesia and dystonia and in the use of anticholinergic medications.
 In a long-term trial designed to assess the maintenance of effect, Invega was significantly more effective than placebo in maintaining symptom control and preventing recurrence of schizophrenia symptoms. After having been treated for an acute episode for six weeks and stabilised for an additional eight weeks with Invega (doses ranging from 3 to 15 mg, flexible dosage regimen), patients were then randomised in a double blind manner to either continue on Invega or placebo until they experienced a recurrence of schizophrenia symptoms. Relapse was predefined as significant increase in PANSS (or predefined PANSS subscales), hospitalisation, clinically significant suicidal or homicidal ideation, or deliberate injury to self or others. The trial was stopped early for efficacy reasons by showing a significantly longer time to recurrence in patients treated with Invega compared to placebo (p < 0.001) (see Figure 1). Invega was also significantly more effective than placebo in maintaining personal and social performance.
In a long-term trial designed to assess the maintenance of effect, Invega was significantly more effective than placebo in maintaining symptom control and preventing recurrence of schizophrenia symptoms. After having been treated for an acute episode for six weeks and stabilised for an additional eight weeks with Invega (doses ranging from 3 to 15 mg, flexible dosage regimen), patients were then randomised in a double blind manner to either continue on Invega or placebo until they experienced a recurrence of schizophrenia symptoms. Relapse was predefined as significant increase in PANSS (or predefined PANSS subscales), hospitalisation, clinically significant suicidal or homicidal ideation, or deliberate injury to self or others. The trial was stopped early for efficacy reasons by showing a significantly longer time to recurrence in patients treated with Invega compared to placebo (p < 0.001) (see Figure 1). Invega was also significantly more effective than placebo in maintaining personal and social performance.
 The Invega group in the study permitting dose adjustment for the first two weeks, followed by fixed dosing (in a range of 3-12 mg/day; mean modal dose of 8.6 mg/day) and the higher dose group of Invega in the 2 dose level study (12 mg with option to reduce to 9 mg daily), were each superior to placebo in the PANSS. In the lower dose group of the 2 dose level study (6 mg with option to reduce to 3 mg daily), Invega was not significantly different from placebo as measured by the PANSS.
The Invega group in the study permitting dose adjustment for the first two weeks, followed by fixed dosing (in a range of 3-12 mg/day; mean modal dose of 8.6 mg/day) and the higher dose group of Invega in the 2 dose level study (12 mg with option to reduce to 9 mg daily), were each superior to placebo in the PANSS. In the lower dose group of the 2 dose level study (6 mg with option to reduce to 3 mg daily), Invega was not significantly different from placebo as measured by the PANSS. Following administration of Invega, the (+) and (-) enantiomers of paliperidone interconvert, reaching an AUC (+) to (-) ratio of approximately 1.6 at steady state.
Following administration of Invega, the (+) and (-) enantiomers of paliperidone interconvert, reaching an AUC (+) to (-) ratio of approximately 1.6 at steady state. C23H27FN4O3. MW = 426.49.
C23H27FN4O3. MW = 426.49.