SUMMARY CMI
Irbesartan GH
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I taking Irbesartan GH?
Irbesartan GH contains the active ingredient irbesartan. Irbesartan GH is used to treat high blood pressure and is also used in the treatment of kidney disease in patients with high blood pressure and type 2 diabetes. For more information, see Section 1. Why am I taking Irbesartan GH? in the full CMI.
2. What should I know before I take Irbesartan GH?
Do not use if you have ever had an allergic reaction to Irbesartan GH or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding. For more information, see Section 2. What should I know before I take Irbesartan GH? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with Irbesartan GH and affect how it works. A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I take Irbesartan GH?
- Your doctor will tell you how many tablets to take each day. The standard dose is one 150 mg tablet per day. This dose may be increased to a 300 mg once per day.
- Swallow the table whole with a glass of water and take Irbesartan GH at about the same time each day.
More instructions can be found in Section 4. How do I take Irbesartan GH? in the full CMI.
5. What should I know while taking Irbesartan GH?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while taking Irbesartan GH? in the full CMI.
6. Are there any side effects?
Common side effects: headache, dizziness or light-headedness, unusual tiredness or weakness, fatigue, nausea/vomiting. Serious side effects: swelling of the face, lips, tongue or throat which may cause difficulty in swallowing or breathing; severe and sudden onset of pinkish, itchy swellings on the skin (hives or nettle rash). Common side effects: headache; dizziness or light-headedness (vertigo); unusual tiredness or weakness, fatigue; nausea/vomiting.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
Irbesartan GH
Active ingredient(s): irbesartan
Consumer Medicine Information (CMI)
This leaflet provides important information about taking Irbesartan GH. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about taking Irbesartan GH.
Where to find information in this leaflet:
1. Why am I taking Irbesartan GH?
2. What should I know before I take Irbesartan GH?
3. What if I am taking other medicines?
4. How do I take Irbesartan GH?
5. What should I know while taking Irbesartan GH?
6. Are there any side effects?
7. Product details
1. Why am I taking Irbesartan GH?
Irbesartan GH contains the active ingredient irbesartan. Irbesartan GH belongs to a group of medicines known as angiotensin-II receptor antagonists. Angiotensin II is a substance produced in the body that causes blood vessels to narrow. Irbesartan GH blocks angiotensin-II and therefore widens your blood vessels, making it easier for your heart to pump blood throughout your body. This helps to lower your blood pressure. Irbesartan GH also slows the decrease of kidney function in patients with high blood pressure and type 2 diabetes.
Irbesartan GH is used to treat high blood pressure, which doctors call hypertension. Irbesartan GH is also used in the treatment of kidney disease in patients with high blood pressure and type 2 diabetes.
2. What should I know before I take Irbesartan GH?
Warnings
Do not take Irbesartan GH if:
- you are allergic to irbesartan, or any of the ingredients listed at the end of this leaflet.
Always check the ingredients to make sure you can use this medicine.
- you are pregnant, think you may be pregnant or are planning to become pregnant.
- you are breastfeeding. It is not known if Irbesartan GH passes into breast milk, therefore it is recommended that you not take it while you are breastfeeding.
- you have diabetes or have kidney problems and are being treated with medicines that lower blood pressure such as an ACE inhibitor, any medicines containing aliskiren or medicines that belong to a group of medicines known as angiotensin-II receptor antagonists (medicines also used to treat high blood pressure).
Check with your doctor if you:
- have any other medical conditions;
- have had recent excessive vomiting or diarrhoea;
- have kidney problems, or you have had a kidney transplant or dialysis;
- have heart problems;
- have liver problems, or have had liver problems in the past;
- have diabetes;
- have high levels of potassium in your blood;
- are strictly restricting your salt intake;
- take any medicines for any other condition;
- are pregnant or intend to become pregnant;
- are breastfeeding or plan to breastfeed;
- plan to have surgery (even at the dentist) that needs a general anaesthetic;
- have allergies to any substances, such as foods, preservatives, or dyes.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Use in children
Irbesartan GH should not be given to children.
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant. Do not take Irbesartan GH if you are pregnant or intend to become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed. Do not take Irbesartan GH if you are breastfeeding.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Tell your doctor if you are taking or plan to take any of the following:
- other medicines to treat high blood pressure;
- potassium supplements or, potassium-containing salt substitutes (you may need to have regular blood tests);
- diuretics;
- medicines containing lithium (you may need to have regular blood tests);
- non-steroidal anti-inflammatory medicines (such as diclofenac or ibuprofen) or COX-2 inhibitors (for example celecoxib). These medicines may be used to relieve pain, swelling and other symptoms of inflammation including arthritis. Taking Irbesartan GH and an anti-inflammatory medicine alone or with a thiazide diuretic (fluid tablet) may damage your kidneys. It may also reduce the effect Irbesartan GH has on lowering blood pressure;
- medicines taken to treat diabetes such as repaglinide. Irbesartan GH might lower your blood glucose levels.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Irbesartan GH.
4. How do I take Irbesartan GH?
How much to take
- The usual starting dose is 150 mg tablet once a day. However, some patients may need a lower starting dose. Your doctor will tell you if this is necessary. The full blood pressure lowering effect of Irbesartan GH should be reached about 4 to 6 weeks after starting treatment.
- Depending on how your blood pressure responds, your daily dose of Irbesartan GH may need to be increased. Most patients take either 150 mg or 300 mg once a day.
- In patients with high blood pressure and type 2 diabetes, 300 mg once a day is the preferred maintenance dose for slowing the progression of associated kidney disease.
- Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
- Follow the instructions provided and use Irbesartan GH until your doctor tells you to stop.
When to take Irbesartan GH
- Take Irbesartan GH at about the same time each day.
How to take Irbesartan GH
- Swallow the tablet whole with a glass of water.
- It does not matter whether you take Irbesartan GH tablets before or after food.
- Continue taking Irbesartan GH until your doctor tells you to stop.
If you forget to take Irbesartan GH
Irbesartan GH should be used regularly at the same time each day.
If you miss your dose at the usual time and it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you take much Irbesartan GH
If you think that you have taken too much Irbesartan GH, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26); or - contact your doctor; or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
If you take too many Irbesartan GH tablets you will probably feel lightheaded or dizzy.
5. What should I know while taking Irbesartan GH?
Things you should do
- Tell any other doctors, dentists, and pharmacists who are treating you that you are taking Irbesartan GH.
- Tell your doctor immediately if you become pregnant while taking Irbesartan GH.
- Have your blood pressure checked when your doctor tells you to, to make sure Irbesartan GH is working.
- If you are about to be started on any new medicine, tell your doctor and pharmacist that you are taking Irbesartan GH.
- If you plan to have surgery that needs a general anaesthetic, tell your doctor or dentist that you are taking Irbesartan GH. Your blood pressure may drop suddenly.
- Make sure you drink enough water during exercise and hot weather when you are taking Irbesartan GH, especially if you sweat a lot. If you do not drink enough water while taking Irbesartan GH, you may faint or feel light-headed or sick. This is because your body does not have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
- Tell your doctor if you have excessive vomiting and/or diarrhoea while taking Irbesartan GH. You may lose too much water and salt and your blood pressure may drop too much.
- Tell your doctor immediately If you feel light-headed or dizzy after taking your first dose of Irbesartan GH, or when your dose is increased.
Things you should not do
- Do not give Irbesartan GH tablets to anyone else, even if they have the same condition as you.
- Do not take Irbesartan GH to treat any other complaints unless your doctor or pharmacist tells you to.
- Do not stop taking Irbesartan GH, or lower the dosage, without checking with your doctor.
Things to be careful of
- If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly.
- Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Irbesartan GH affects you.
As with many other medicines used to treat high blood pressure, Irbesartan GH may cause dizziness or light-headedness in some people. If this occurs do not drive.
Make sure you know how you react to Irbesartan GH before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed.
Drinking alcohol
Tell your doctor if you drink alcohol.
If you drink alcohol, dizziness or light-headedness may be worse.
Looking after your medicine
- Keep Irbesartan GH tablets in a cool dry place where the temperature stays below 25°C.
- Keep your tablets in the blister pack until it is time to take them.
Follow the instructions on the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight. For example, do not store it:
- in the bathroom or near a sink; or
- in the car or on window sills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Allergy-related symptoms:
| Stop taking Irbesartan GH and call your doctor straight away or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Irbesartan GH contains
| Active ingredient (main ingredient) | Irbesartan |
| Other ingredients (inactive ingredients) | Colloidal anhydrous silica Crospovidone Magnesium stearate Mannitol Povidone Purified water Sodium lauryl sulfate Opadry complete film-coating system 03B28796 White |
Do not take this medicine if you are allergic to any of these ingredients.
What Irbesartan GH looks like
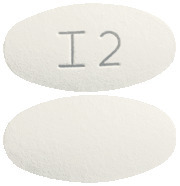
Irbesartan GH 75 mg tablets are white to off-white, oval-shaped, film-coated tablets embossed with “I1” on one side and plain on the other side (AUST R 191408).
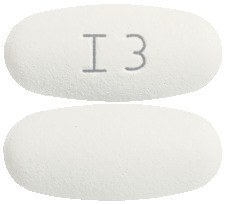
Irbesartan GH 150 mg tablets are white to off-white, oval-shaped, film-coated tablets embossed with “I2” on one side and plain on the other side (AUST R 191404).
Irbesartan GH 300 mg tablets are white to off-white, oval-shaped, film-coated tablets embossed with “I3” on one side and plain on the other side (AUST R 191084).
Who distributes Irbesartan GH
Generic Health Pty Ltd
Suite 2, Level 2
19-23 Prospect Street
Box Hill, VIC, 3128
Australia
 +61 3 9809 7900
+61 3 9809 7900
This leaflet was prepared in April 2021.
Published by MIMS July 2021




 Adverse reactions that occurred in 2 or more hypertensive patients in clinical trials involving 3,396 patients have been classified using standard terminology and in the following listing are categorised by body system and listed in order of decreasing frequency according to the following definitions: common adverse reactions are those occurring on one or more occasions in at least 1/100 but less than 1/10 patients; uncommon adverse reactions are those occurring in at least 1/1,000 but less than 1/100 patients; rare adverse reactions are those occurring in less than 1/1,000 patients.
Adverse reactions that occurred in 2 or more hypertensive patients in clinical trials involving 3,396 patients have been classified using standard terminology and in the following listing are categorised by body system and listed in order of decreasing frequency according to the following definitions: common adverse reactions are those occurring on one or more occasions in at least 1/100 but less than 1/10 patients; uncommon adverse reactions are those occurring in at least 1/1,000 but less than 1/100 patients; rare adverse reactions are those occurring in less than 1/1,000 patients. Chemical Name: 2-butyl-3-[(2'-(1H-tetrazol-5-yl) biphenyl-4-yl) methyl]-1, 3-diazaspiro [4, 4] non-1-en-4-one.
Chemical Name: 2-butyl-3-[(2'-(1H-tetrazol-5-yl) biphenyl-4-yl) methyl]-1, 3-diazaspiro [4, 4] non-1-en-4-one.