WHAT IS IN THIS LEAFLET
This leaflet answers some common questions about Irbesartan/HCT Sandoz.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
WHAT IRBESARTAN/HCT SANDOZ IS USED FOR
This medicine is used to lower high blood pressure, which doctors call hypertension.
Your doctor measured your blood pressure and found it to be too high. Everyone has blood pressure. This pressure helps get your blood all around your body. Your blood pressure may be different at different times of the day, depending on how busy or worried you are. You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
There are often no symptoms of high blood pressure. The only way of knowing that you have high blood pressure is to have your blood pressure checked on a regular basis.
If high blood pressure is not treated, it can damage blood vessels in several organs such as the heart, kidneys, brain and eyes. This may lead to serious health problems, such as blindness, stroke, heart disease and kidney failure. There are usually no symptoms of high blood pressure before damage occurs, so your doctor needs to measure your blood pressure to see if it is too high.
High blood pressure can be treated and controlled with medicines such as Irbesartan/HCT Sandoz. Your doctor may also have recommended that you adjust your lifestyle to help to lower your high blood pressure (losing weight, avoiding smoking, reducing alcohol consumption and restricting the amount of salt in the diet). Your doctor may also have encouraged the practice of regular, mild (not strenuous) exercise such as walking, swimming, etc.
This medicine contains the active ingredients irbesartan and hydrochlorothiazide. Both medicines reduce blood pressure in different ways.
Irbesartan belongs to a group of medicines known as angiotensin-II receptor antagonists. Angiotensin II is a substance produced in the body that causes blood vessels to narrow. Irbesartan blocks angiotensin-II and therefore relaxes your blood vessels. This helps to lower your blood pressure.
Hydrochlorothiazide belongs to the class of medicines known as diuretics. Diuretics cause an increase in the volume of urine. They also help with lowering blood pressure particularly when combined with other blood pressure reducing medicines.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is available only with a doctor's prescription.
There is no evidence that this medicine is addictive.
BEFORE YOU TAKE IRBESARTAN/HCT SANDOZ
When you must not take it
Do not take this medicine if you have an allergy to:
- irbesartan or hydrochlorothiazide, the active ingredients, or to any of the other ingredients listed at the end of this leaflet under Product Description
- sulfonamide derived medicines (commonly known as sulfur drugs)
- any other similar medicines.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Do not take this medicine if you are pregnant or are planning to become pregnant. It may affect your developing baby if you take it during pregnancy.
Do not breastfeed if you are taking this medicine. It is not known if the active ingredient in Irbesartan/HCT Sandoz passes into breast milk, therefore it is recommended that you do not take it while you are breastfeeding.
Do not give this medicine to children. Safety and effectiveness in children have not been established.
Do not take this medicine if you are not producing urine.
Do not take this medicine if you are diabetic or have kidney problems and are being treated with an ACE inhibitor, any aliskiren-containing medicines or a group of medicines known as AIIRAs (medicines also used to treat high blood pressure).
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- kidney problems, or have had a kidney transplant or dialysis
- heart problems
- liver problems, or have had liver problems in the past
- diabetes
- gout or have had gout in the past
- lupus erythematosus
- high or low levels of potassium or sodium or other electrolytes in your blood
- primary aldosteronism.
Tell your doctor if you:
- are strictly restricting your salt intake
- plan to have surgery (even at the dentist) that needs a general anaesthetic
- have recently had excessive vomiting or diarrhoea or think you are dehydrated
- are lactose intolerant
- have had a sympathectomy
- have been taking diuretics
- have a history of allergy or asthma.
- you have had skin cancer or you develop an unexpected skin lesion during the treatment. Treatment with hydrochlorothiazide, particularly long term use with high doses, may increase the risk of some types of skin and lip cancer (nonmelanoma skin cancer). Protect your skin from sun exposure and UV rays while taking Irbesartan/HCT Sandoz.
Tell your doctor if you are pregnant or plan to become pregnant or are breastfeeding. Your doctor can discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell him/her before you start taking Irbesartan/HCT Sandoz.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Irbesartan/HCT Sandoz may interfere with each other. These include:
- other medicines for high blood pressure
- other fluid tablets or diuretics
- lithium or lithium-containing medicines (for example lithium carbonate)
- potassium tablets
- potassium containing salt substitutes
- anti-inflammatory medicines, used to relieve pain, swelling and other symptoms of inflammation, including arthritis and nonsteroidal anti-inflammatory agents - NSAIDS (for example diclofenac, ibuprofen) and COX-2 inhibitors (for example celecoxib). Taking a combination of Irbesartan/HCT Sandoz and an anti-inflammatory medicine, alone or with a thiazide diuretic (fluid tablet) may damage your kidneys. It may also reduce the effect Irbesartan/HCT Sandoz has on reducing blood pressure.
- a medicine containing aliskiren. Taking Irbesartan/HCT Sandoz with aliskiren may affect your blood pressure, electrolyte balance and your kidney function
- alcoholic drinks
- sleeping tablets
- codeine or morphine, strong pain killing medicines
- medicines for diabetes (oral tablets or capsules or insulins)
- calcium supplements, medicines containing calcium
- Vitamin D
- medicines for gout
- powder or granule medicines, used to help reduce cholesterol (cholestyramine or colestipol hydrochloride)
- heart medicines such as digoxin or antiarrhythmic medicines (for example sotalol hydrochloride)
- corticosteroid medicines such as prednisone, cortisone or ACTH
- medicines used to treat cancer (cytotoxic medicines)
- amantadine, a medicine used to treat Parkinson's disease or to prevent influenza
- anticholinergic medicines, used to treat Parkinson's disease, to relieve stomach cramps or spasms or used to prevent travel sickness
- carbamazepine, anticonvulsant medication
- medicines used during surgery
- medicines used in an emergency situation such as adrenaline.
These medicines may be affected by Irbesartan/HCT Sandoz or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
HOW TO TAKE IRBESARTAN/HCT SANDOZ
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions, ask your doctor or pharmacist for help.
How much to take
Irbesartan/HCT Sandoz will usually be prescribed by your doctor if previous treatment does not produce a sufficient drop in your blood pressure. Your doctor will tell you how to switch from your previous treatment to Irbesartan/HCT Sandoz.
The usual dose of Irbesartan/HCT Sandoz is one tablet a day. The full blood pressure lowering effect should be reached 6-8 weeks after beginning treatment. If your blood pressure is not satisfactorily reduced with Irbesartan/HCT Sandoz, your doctor may prescribe another medicine to be taken with Irbesartan/HCT Sandoz.
Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
Follow the instructions they give you.
If you take the wrong dose, Irbesartan/HCT Sandoz may not work as well and your problem may not improve.
How to take it
The tablets should be taken regularly as directed by your doctor. The tablets should be swallowed whole with a full glass of water.
It does not matter whether you take the tablets before or after food.
When to take Irbesartan/HCT Sandoz
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
How long to take Irbesartan/HCT Sandoz
Continue taking your medicine for as long as your doctor tells you.
This medicine helps to control your high blood pressure, but it does not cure it. Therefore Irbesartan/HCT Sandoz must be taken every day. Continue taking Irbesartan/HCT Sandoz until your doctor tells you to stop.
If you forget to take it
Take your dose as soon as you remember, and continue to take it as you would normally.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 POISON or 0800 764766) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much Irbesartan/HCT Sandoz. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of an overdose may include light-headedness or dizziness.
WHILE YOU ARE TAKING IRBESARTAN/HCT SANDOZ
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking Irbesartan/HCT Sandoz.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
If you become pregnant while taking this medicine, tell your doctor immediately.
Have your blood pressure checked when your doctor tells you to, to make sure this medicine is working.
If you plan to have surgery or other treatment (even at the dentist) that needs a general anaesthetic, tell your doctor or dentist that you are taking this medicine. Your blood pressure may drop suddenly.
Make sure you drink enough water during exercise and hot weather when you are taking this medicine, especially if you sweat a lot. If you do not drink enough water while taking this medicine, you may faint or feel light-headed or sick. This is because your body does not have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
If you have excessive vomiting and/or diarrhoea while taking this medicine, tell your doctor. You may lose too much water and salt and your blood pressure may drop too much.
Get up slowly when getting out of bed or standing up. You may feel light-headed or dizzy while taking Irbesartan/HCT Sandoz. This may become worse if you stand up quickly as your blood pressure may fall. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If you get dizzy or lightheaded talk to your doctor.
Tell your doctor if you experience an increased sensitivity of the skin to the sun with symptoms of sunburn (such as redness, itching, swelling, blistering) occurring more quickly than normal.
Things you must not do
Do not take Irbesartan/HCT Sandoz to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how Irbesartan/HCT Sandoz affects you. This medicine may cause dizziness or light-headedness in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Be careful when drinking alcohol while you are taking this medicine. If you drink alcohol, dizziness or light-headedness may be worse.
The hydrochlorothiazide contained in this medicine could produce a positive analytical result in an antidoping test.
SIDE EFFECTS
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Irbesartan/HCT Sandoz.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- headache
- dizziness or light-headedness (vertigo)
- unusual tiredness or weakness, fatigue
- pain in the stomach or gout; nausea and/or vomiting
- sexual problems.
These are common side effects. They are generally mild and do not normally require treatment to be interrupted.
Tell your doctor immediately if you notice any of the following:
- skin rash or itchiness (symptoms of an allergic reaction)
- aching muscles or aching joints (not caused by exercise)
- muscle pain, weakness or paralysis of muscles
- buzzing, ringing or other persistent noise in the ear
- changes in heart rhythm
- not urinating (passing water) as much as normal
- numbness or tingling in fingers or toes
- painful, swollen joints which may be symptoms of gout
- fainting
- yellowing of the skin and/or eyes, also known as jaundice
- symptoms that may occur if you have developed diabetes, such as excessive thirst, passing greatly increased amounts of urine, increased appetite with weight loss, feeling tired, drowsy, weak, depressed, irritable and generally unwell
- symptoms that may indicate kidney disease, such as passing little or no urine, drowsiness, nausea, vomiting, breathlessness, loss of appetite and weakness
- symptoms that may indicate high potassium levels in the blood, such as nausea, diarrhoea, muscle weakness, change in heart rhythm
- symptoms that may indicate liver disease such as nausea, vomiting, loss of appetite, feeling generally unwell, fever, itching, yellowing of the skin and eyes and dark coloured urine
- symptoms that may indicate low platelet count such as easy or excessive bruising, bleeding from gums or nose, prolonged bleeding from cuts and blood in urine or stools
- disturbances in your vision (such as blurred vision and seeing haloes around lights) and eye pain.
The above list includes serious side effects that may require medical attention. Serious side effects are not common.
If any of the following happen, stop taking this medicine and tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- swelling of the face, lips, tongue or throat which may cause difficulty in swallowing or breathing
- severe and sudden onset of pinkish, itchy swellings on the skin, also called hives or nettle rash.
The above list includes serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may also occur in some people.
AFTER TAKING IRBESARTAN/HCT SANDOZ
Storage
Keep your medicine in the original container.
If you take it out of its original container it may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C.
Keep your medicine where it is protected from moisture.
Do not store Irbesartan/HCT Sandoz or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car.
Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
PRODUCT DESCRIPTION
What it looks like
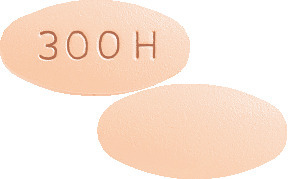
Irbesartan/HCT Sandoz 150 mg/12.5 mg - apricot, oval biconvex film-coated tablet, debossed with 150H on one side.
Irbesartan/HCT Sandoz 300 mg/12.5 mg - apricot, oval biconvex film-coated tablet, debossed with 300H on one side.
Irbesartan/HCT Sandoz 300 mg/25 mg - dark pink, oval biconvex film-coated tablet, debossed with 300 on one side and 25H on the other side.
Available in bottles and blister packs of 30 tablets.
Not all strengths or presentations may be marketed.
Ingredients
Active ingredients:
- Irbesartan/HCT Sandoz 300 mg/25 mg - 300 mg irbesartan and 25 mg hydrochlorothiazide
- Irbesartan/HCT Sandoz 150 mg/12.5 mg - 150 mg irbesartan and 12.5 mg hydrochlorothiazide
- Irbesartan/HCT Sandoz 300 mg/12.5 mg - 300 mg irbesartan and 12.5 mg hydrochlorothiazide.
Inactive ingredients:
- microcrystalline cellulose
- lactose monohydrate
- croscarmellose sodium
- colloidal anhydrous silica
- hypromellose
- magnesium stearate
- hyprolose
- macrogol 6000
- titanium dioxide
- talc
- iron oxide red (CI77491)
- iron oxide yellow (CI77492) - Irbesartan/HCT Sandoz 150 mg/12.5 mg and 300 mg/12.5 mg only
- iron oxide black (CI77499) - Irbesartan/HCT Sandoz 300 mg/25 mg only.
This medicine does not contain sucrose or gluten.
Supplier
Sandoz Pty Ltd
ABN 60 075 449 553
54 Waterloo Road
Macquarie Park NSW 2113
Tel: 1800 726 369
Novartis New Zealand Ltd
PO Box 99102
Newmarket, Auckland 1149
New Zealand
Tel: 0800 354 335
This leaflet was prepared in November 2019.
Australian Register Number(s)
150 mg/12.5 mg tablets: AUST R 174729 (blister)
300 mg/12.5 mg tablets: AUST R 174724 (blister)
300 mg/25 mg tablets: AUST R 174731 (blister)
Published by MIMS January 2020



 Adverse effects (clinical events probably or possibly related to therapy as determined by the clinical investigator) that occurred in more than 2 hypertensive patients when they were taking irbesartan/ hydrochlorothiazide and no additional study medications in premarketing clinical trials involving 2700 subjects, and that were not reported in the above tabulation of adverse events, are listed in the following section.
Adverse effects (clinical events probably or possibly related to therapy as determined by the clinical investigator) that occurred in more than 2 hypertensive patients when they were taking irbesartan/ hydrochlorothiazide and no additional study medications in premarketing clinical trials involving 2700 subjects, and that were not reported in the above tabulation of adverse events, are listed in the following section. Chemical name: 2-butyl-3-[(2'-(1H-tetrazol-5-yl) biphenyl-4-yl)methyl]-1,3-diazaspiro[4,4] non-1-en-4-one.
Chemical name: 2-butyl-3-[(2'-(1H-tetrazol-5-yl) biphenyl-4-yl)methyl]-1,3-diazaspiro[4,4] non-1-en-4-one. Chemical name: 6-chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1- dioxide.
Chemical name: 6-chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1- dioxide.