What is in this leaflet
This leaflet answers some common questions about Largactil.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor or pharmacist has weighed the risks of you taking Largactil against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with this medicine. You may need to read it again.
What Largactil is used for
The active ingredient of Largactil is chlorpromazine hydrochloride, one of a group of medicines called phenothiazines.
Largactil is used to treat a number of conditions and may be used either for a short time or for a long time. Largactil is used to treat various problems such as severe depression or behavioural disturbances. Largactil can also be used to treat nausea, vomiting, severe pain and unstoppable hiccups. Your doctor may have prescribed Largactil for another reason.
Ask your doctor if you have any questions about why Largactil has been prescribed for you.
Largactil is available only with a doctor's prescription.
Before you take it
When you must not take it
Do not take Largactil if you have an allergy or any other reaction to Largactil or any of the ingredients listed at the end of this leaflet.
Do not take Largactil if you have taken any other 'phenothiazine' medicine before, which caused your face, lips, tongue, throat, hands or feet to swell up, or made it hard for you to breathe. If you have had an allergic reaction to a phenothiazine before, you may be allergic to Largactil.
Do not take Largactil if you have any of the following:
- circulatory, blood or bone marrow problems
- high blood pressure
- phaeochromocytoma - a rare tumour of the adrenal gland which sits near the kidneys
- liver problems
- CNS depression, e.g. coma or drug intoxication
Do not take Largactil after the expiry date (EXP) printed on the pack. If you take this medicine after the expiry date has passed, it may not work as well.
Do not take Largactil if the packaging is torn or shows signs of tampering or if the tablet, syrup or ampoule doesn't look quite right.
If you are not sure whether you should start taking Largactil, contact your doctor or pharmacist.
Before you start to take it
Tell your doctor or pharmacist if you have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes
Tell your doctor or pharmacist if you are pregnant or intend to become pregnant. Your doctor or pharmacist will discuss the possible risks and benefits of using Largactil during pregnancy.
Tell your doctor or pharmacist if you are breast-feeding or plan to breast-feed. Your doctor or pharmacist will discuss the possible risks and benefits of using Largactil during breastfeeding.
Tell your doctor or pharmacist if you have or have had any medical conditions, especially the following:
- asthma
- chronic respiratory disorders
- kidney or liver disease
- heart disease
- blood clots
- decreased parathyroid activity
- low blood calcium levels
- Parkinson's disease
- prostate problems
- epilepsy - fits and seizures
- glaucoma - high pressure in the eye
- muscle weakness (myasthenia gravis)
- diabetes
- dementia
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking Largactil.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Largactil may interfere with each other. These include:
- benztropine and levodopa - drugs used to treat Parkinson's disease
- antacid - used to treat stomach upsets
- lithium - used to treat mood disorders
- barbiturates - a group of drugs used as sedatives
- tricyclic antidepressants
- benzodiazepines - a group of drugs used to treat anxiety and muscle spasms
- other antipsychotics
- medicines that are CYP1A2 inhibitors e.g. ciprofloxacin, fluvoxamine, oral contraceptives, vemurafenib
- medicines used to treat a fast or irregular heart beat e.g. amiodarone, quinidine, disopyramide
- medicines that can slow your heart beat e.g. diltiazem, verapamil, propranolol
- medicines that can reduce potassium levels in the blood e.g. diuretics, laxatives
- other medicines that can affect your heart rate e.g. methadone, pentamidine
- anaesthetics
- opioids - a group of pain killing drugs
- antidiabetic agents - a group of drugs used to treat diabetes
- amphetamines
- anticoagulants
- anticholinergics
- guanethidine
- clonidine
- thiazides - diuretics (fluid tablets)
- MAOI - a group of drugs used to treat depression
- adrenaline
- suxamethonium, atropine and organophosphorous insecticides
- anticonvulsants - a group of drugs used to treat epilepsy e.g. phenytoin, valproic acid
- prochlorperazine - a drug used to treat nausea and vomiting
- desferrioxamine - a drug used to treat iron poisoning
These medicines may be affected by Largactil, or they may affect how well it works. You may need different amounts of your medicine, or you may need to use different medicines. Your doctor or pharmacist will advise you.
Your doctor and pharmacist may have more information on medicines to be careful with or to avoid while taking Largactil.
How to take it
How much to take
Your doctor or pharmacist will tell you how many tablets or how much syrup you will need to take each day. This depends on your condition and whether or not you are taking any other medicines.
Follow all directions given to you by your doctor and pharmacist carefully.
If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
How to take it
Swallow the prescribed dose of Largactil tablets whole with a full glass of water. Do not chew the tablets.
Swallow the prescribed dose of Largactil syrup and follow with a glass of water.
Largactil may be given as an injection into a muscle or as a slow injection into a vein. Largactil injections should only be given by a doctor, nurse or other trained person.
When to take it
Take Largactil at about the same time each day. Taking your tablets or syrup at the same time each day will have the best effect. It will also help you remember when to take the tablets or syrup.
If you forget to take it
If you miss a dose, simply continue to take Largactil as advised by your doctor or pharmacist. You do not need to make up for the missed dose.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist. If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
How long to take it
Continue taking Largactil until your doctor or pharmacist tells you to stop. Do not stop using it unless your doctor or pharmacist tells you to, even if you feel better.
If you take too much (overdose)
Immediately telephone your doctor or pharmacist or the Poisons Information Centre (telephone Australia 13 11 26, New Zealand 0800 POISON or 0800 764766), or go to accident and emergency at your nearest hospital, if you think that you or anyone else may have taken too much Largactil. Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention. If you take too much Largactil, you may experience:
- drowsiness
- confusion
- restlessness
- excitement
- breathing difficulties
- fast heart rate
- muscle twitching
While you are using it
Things you must do
Tell your doctor immediately if you notice any worm-like movements of the tongue, or other uncontrolled movements of the tongue, mouth, cheeks or jaw which may progress to the arms and legs.
These are symptoms of a condition called tardive dyskinesia, which may develop in people taking phenothiazine medicines, including Largactil.
This condition is more likely to occur during long term treatment with Largactil, especially in elderly women. In very rare cases, this may be permanent. However, if detected early, these symptoms are usually reversible.
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking Largactil.
If you plan to have surgery that needs a general anaesthetic, tell your doctor or dentist that you are taking Largactil.
If you become pregnant while taking Largactil, tell your doctor or pharmacist.
You should avoid very cold or very hot environments. Largactil may make it difficult for your body to regulate its temperature.
You should avoid exposure to strong sunlight while you are taking Largactil. Do not use a sunlamp or tanning bed or booth. Largactil may cause your skin to be much more sensitive to sunlight than it is normally. Exposure to sunlight may cause a skin rash, itching, redness or severe sunburn. If your skin does appear to be burning, tell your doctor. If exposure to strong sunlight is unavoidable, suitable clothing, including a hat, should be worn. A sunscreen with a high level of protection should also be used.
Things you must not do
Do not give Largactil to anyone else, even if they have the same condition as you.
Do not take Largactil to treat any other complaints unless your doctor or pharmacist tells you to.
Things to be careful of
Be careful when drinking alcohol while taking Largactil. Combining Largactil and alcohol can make you more sleepy, dizzy or light headed. Your doctor may suggest you avoid alcohol while you are being treated with Largactil.
Be careful driving or operating machinery until you know how Largactil affects you. Largactil may cause drowsiness in some people. Make sure you know how you react to Largactil before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed. If this occurs, do not drive. If you drink alcohol, dizziness or light-headedness may be worse.
If Largactil makes you feel light-headed, dizzy or faint, be careful when getting up from a sitting or lying position. Getting up slowly may help.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Largactil.
Largactil helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
If you are over 65 years of age, you may have an increased chance of getting side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- dizziness or light headedness
- skin problems or discolouration
- agitation
- drowsiness or tiredness
- headache
- constipation
- nausea
- dry mouth
- nasal congestion
- difficulty in urinating
- blurred vision
- impotence
- weight gain
These are the more common side effects of Largactil. Mostly these are mild and short-lived.
If any of the following happen, stop taking Largactil and tell your doctor or pharmacist immediately or go to casualty at your nearest hospital:
- sore throat, fever or any sign of infection
- breathing difficulty
- seizures or fits
- unwanted muscle movements of the mouth, tongue, jaw, cheeks or arms and legs.
- hardness or rigidity of the muscles.
- fast heartbeat
- uncontrolled bleeding or bruising more easily than usual
These are very serious side effects. You may need urgent medical attention or hospitalisation.
Other side effects not listed above may occur in some patients. Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Storage
Largactil ampoules for injection will be stored in the pharmacy or on the ward. The injection is kept in a cool dry place, protected from light.
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they will not keep as well.
Keep your tablets or syrup in a cool dry place. Do not store Largactil or any other medicine in the bathroom or near a sink. Do not leave it in the car on hot days or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking Largactil or the tablets or syrup has passed the expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
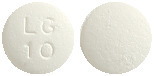
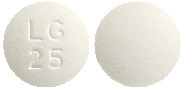
Largactil tablets are white film coated tablets with embossing on one side:
10mg tablet: LG / 10
25mg tablet: LG / 25
100mg tablet: LG / 100
Tablets are available in blister packs of 100.
Largactil syrup* is a dark orange syrupy liquid with the odour of spearmint / peppermint, and is slightly fruity. Syrup is available in an amber glass 100mL bottle with a childproof cap.
Largactil for injection is a clear liquid in a 2mL glass ampoule, in a pack of 10 ampoules.
Ingredients
Largactil tablets contain:
- chlorpromazine hydrochloride 10mg, 25mg, or 100mg (active ingredient)
- lactose monohydrate
- maize starch
- colloidal anhydrous silica
- magnesium stearate
- hypromellose
- macrogol 200
- titanium dioxide
Largactil syrup* contains:
- chlorpromazine hydrochloride 25mg/5mL (active ingredient)
- sucrose
- caramel
- citric acid
- polysorbate 20
- peppermint oil
- spearmint oil
- sodium citrate dihydrate
- ascorbic acid
- sodium sulphite
- sodium metabisulphite
- sodium benzoate
- fruit cup essence
- purified water
Largactil ampoules contain:
- chlorpromazine hydrochloride 50mg/2mL (active ingredient)
- sodium sulfite
- sodium metabisulphite
- sodium chloride
- sodium citrate dihydrate
- water for injections
Sponsor
- sanofi-aventis australia pty ltd
12-24 Talavera Road
Macquarie Park NSW 2113
Toll Free Number (medical information): 1800 818 806
Email: [email protected] - sanofi-aventis new zealand limited
Level 8, 56 Cawley Street Ellerslie
Auckland, New Zealand
Toll Free Number (medical information): 0800 283 684
Email: [email protected]
Largactil® is a registered trademark.
Australian Registration Numbers:
10mg tablet AUST R 51620
25mg tablet AUST R 51618
100mg tablet AUST R 51619
25mg/5mL syrup AUST R 118128
50mg/2mL ampoule AUST R 27511
This leaflet was prepared in December 2019.
* Largactil Syrup not available in New Zealand
largactil-ccdsv4-cmiv8-17dec19
Published by MIMS March 2020


 Chlorpromazine is 10-(3-dimethyl-aminopropyl)-2-chlorophenothiazine, a dimethylamine derivative of phenothiazine. Chlorpromazine 100 mg is approximately equivalent to 111 mg of chlorpromazine hydrochloride.
Chlorpromazine is 10-(3-dimethyl-aminopropyl)-2-chlorophenothiazine, a dimethylamine derivative of phenothiazine. Chlorpromazine 100 mg is approximately equivalent to 111 mg of chlorpromazine hydrochloride.