What is in this leaflet
This leaflet answers some common questions about MersynoNight Night Time Pain Relief. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits.
Your doctor or pharmacist has weighed the risks of you using MersynoNight Night Time Pain Relief against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What MersynoNight Night Time Pain Relief is used for
MersynoNight Night Time Pain Relief is used to give temporary relief of pain when associated with sleeping difficulty.
It is useful for headache, migraine, backache, arthritis, rheumatic and muscle pain, neuralgia, toothache or period pain.
Paracetamol is an analgesic. It works to stop the pain messages from getting through to the brain. It also acts in the brain to reduce fever.
Diphenhydramine hydrochloride is an antihistamine that helps you sleep.
Ask your doctor or pharmacist if you have any questions about why this medicine has been prescribed for you.
Your pharmacist or doctor may have given you this for another reason.
This medicine is only available from your pharmacist.
Before you use MersynoNight Night Time Pain Relief
When you must not use it
Do not take MersynoNight Night Time Pain Relief if you have an allergy to:
- any medicine containing paracetamol or diphenhydramine hydrochloride
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take MersynoNight Night Time Pain Relief if you have or had any of the following medical conditions:
- glaucoma (high pressure in the eyes)
- stomach or duodenal ulcer or other stomach problems
- prostate problems
- bladder problems
Do not take MersynoNight Night Time Pain Relief:
- if you are taking monoamine oxidase inhibitors (MAOIs), a type of
- medicine used to treat depression.
- if you have taken other medicine containing paracetamol in the last 4 hours.
- if you are breastfeeding or plan to breastfeed. It passes into the breast milk and there is a possibility that the baby may be affected.
Do not give MersynoNight Night Time Pain Relief:
- to newborn or premature babies.
- to children under 12 years of age.
Do not take this medicine after the expiry date (EXP) printed on the pack.
If you take it after the expiry has passed, it may not work as well.
Do not take this medicine if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to use it
Tell your doctor if you have or have had any of the following medical conditions:
- Liver or kidney disease
- Epilepsy
- Myasthenia gravis (a muscle dysfunction)
- Prostate gland enlargement or difficulty urinating
- Glaucoma
- Asthma
- Bronchitis or chronic lung disease
- Underweight or malnourished
- You regularly drink alcohol; you may need to avoid using this product altogether or limit the amount of paracetamol you take
- You have a severe infection as this may increase the risk of metabolic acidosis. Signs of metabolic acidosis include deep rapid difficult breathing, nausea or vomiting. Loss of appetite. Contact a doctor immediately if you get a combination of these symptoms
Tell your pharmacist or doctor if you take sedatives.
Tell your doctor if you are pregnant or plan to become pregnant. Your pharmacist or doctor will discuss the benefits and possible risks of taking the medicine during pregnancy.
If you have not told your pharmacist or doctor about any of the above, tell him/her before you start taking MersynoNight Night Time Pain Relief.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and MersynoNight Night Time Pain Relief may interfere with each other.
These include:
- Warfarin, a medicine used to prevent blood clots
- Metoclopramide, a medicine used to control nausea and vomiting
- Medicines used to treat epilepsy or fits
- Chloramphenicol, an antibiotic used to treat ear and eye infections
- Alcohol
- Probenecid
- Cholestyramine
- Medicines used to treat depression, especially monoamine oxidase inhibitors and tricyclic antidepressants
- Medicines used to help you sleep or relax (sedatives and hypnotics)
- Opioid analgesics, medicines used to treat pain
- Other antihistamine medicines including cough and cold medicines and those you use on your skin.
- Medicines which make you drowsy or give you a dry mouth (sometimes called anticholinergics). Taking such medicines while you are taking this medicine may increase the chances of side effects.
These medicines may be affected by MersynoNight Night Time Pain Relief or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your pharmacist or doctor will have more information on these and other medicines to be careful with or avoid while taking this medicine.
This product contains paracetamol. If you are taking any other medicine containing paracetamol, you must make sure you do not take more than 4000mg paracetamol (including this product) in any 24 hour period.
If in doubt, consult your doctor or pharmacist.
How to USE MersynoNight Night Time Pain Relief
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to use
Take one or two tablets.
Do not take more than the stated dose.
If you are over 65 years of age, talk to your pharmacist or doctor about how much to use. Elderly patients are more likely to have side effects from taking this medicine. Carers should be aware that this medicine should not be given to elderly patients with confusion.
How to use it
Take with water or other fluid. Take the tablets at bedtime.
How long to use it for
Adults should not take this medicine for more than a few days at a time unless your doctor tells you to take it for longer.
Children aged 12 to 17 years should not take this medicine for more than 48 hours unless on the advice of a doctor.
Children under 12 years of age should not be given MersynoNight Night Time Pain Relief.
If you forget to use it
If you forget to take MersynoNight Night Time Pain Relief at bedtime, you may take it through the night.
Do not take a second dose.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much MersynoNight Night Time Pain Relief. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep telephone numbers of these places handy.
While you are using MersynoNight Night Time Pain Relief
Things you must do
Talk to your pharmacist or doctor if your symptoms do not improve. Your pharmacist or doctor will assess your condition and decide if you should continue to take the medicine.
Use MersynoNight Night Time Pain Relief exactly as your pharmacist or doctor has told you to.
Tell all your doctors, dentists and pharmacists that you are using MersynoNight Night Time Pain Relief.
Things you must not do
Children 12 to 17 years:
Do not give paracetamol for more than 48 hours unless a doctor has told you to.
Adults:
Do not take for more than a few days at a time unless your doctor tells you to.
Do not use this medicine to treat any other complaints unless your pharmacist or doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not take more than the stated dose unless your doctor tells you to.
Do not drink alcohol while taking MersynoNight Night Time Pain Relief. The sedation effects of alcohol may be increased.
Things to be careful of
This product may cause dizziness, drowsiness, difficulty concentrating or blurred vision.
Be careful driving or operating machinery until you know how the medicine affects you.
Please see your doctor if your symptoms do not improve.
Keep out of sight and reach of children.
This medicine may cause sleepiness in some people.
If this happens, do not drive or operate machinery.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking MersynoNight Night Time Pain Relief.
This medicine helps most people with pain when associated with sleeping difficulty, but it may have unwanted side effects in a few people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Tell your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- nausea or dyspepsia
- drowsiness or sleepiness
- dry mouth, nose and throat
- constipation
- nervousness and irritability
- anxiety
- hallucinations
- twitching or jerking muscles
- fast heart beat
- tiredness
- dizziness
- difficulty concentrating
- unsteadiness
The above list includes the more common side effects of your medicine. They are usually mild.
Tell your doctor as soon as possible if you notice any of the following:
- difficult or painful urination
- seizures (fits)
The above list includes serious side effects that may require medical attention. These side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
- previous breathing problems with aspirin or non-steroidal anti-inflammatories, and you experience a similar reaction with this product.
- unexplained bruising or bleeding
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After using MersynoNight Night Time Pain Relief
Storage
Keep your medicine in the original pack until it is time to take it. If you keep the tablets out of their packaging, they may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C. Protect from moisture.
Do not store MersynoNight Night Time Pain Relief or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
Ask your pharmacist what to do with any medicine that is left over, or if the expiry date has passed.
Product description
What it looks like
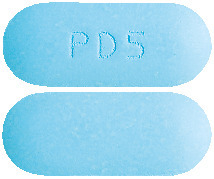
MersynoNight Night Time Pain Relief is a blue, capsule shaped, film coated tablet debossed with "PD5" on one side and plain on the other side, supplied in blister packs of 20 tablets.
Ingredients
Each MersynoNight Night Time Pain Relief tablet contains 500 mg paracetamol and 25 mg diphenhydramine hydrochloride as active ingredients.
It also contains:
- Maize starch
- Potassium sorbate
- Povidone
- Croscarmellose sodium
- Purified talc
- Stearic acid
- Opadry complete film coating system 03F505035 Blue
Supplier
Sanofi Consumer Healthcare
87 Yarraman Place Virgina QLD 4014
Australia
AUST R 301428
This leaflet was prepared: 28 March 2018
™ = Trademark
Published by MIMS February 2019