What Is In This Leaflet
This leaflet answers some common questions about Nerlynx Tablets.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Nerlynx against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may want to read it again.
What Nerlynx Is Used For
Nerlynx contains the active substance neratinib. Neratinib belongs to a group of medicines called ‘tyrosine kinase inhibitors’ used to block cancer cells and treat breast cancer.
Nerlynx is used for patients who have early stage breast cancer which:
- is human epidermal growth factor receptor 2-positive (HER2-positive) and
- has previously been treated with another medicine called ‘trastuzumab’ and
- within one year of trastuzumab therapy.
The ‘HER2 receptor’ is a protein found on the surface of healthy breast cells in the body. It helps control how healthy breast cells grow. HER2 is found in large amounts on the surface of cancer cells. When Nerlynx binds to HER2, it stops the growth and spread of cancer cells.
Before Nerlynx is used, your cancer must have been tested to show it is HER2-positive. You must also have previously been treated with trastuzumab.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
This medicine is only available with a prescription from a doctor experienced with chemotherapy treatment.
There is no evidence that this medicine is addictive.
Before you take it
When you should not take it
You should not take this medicine if you have an allergy to:
- neratinib
- any of the other ingredients of this medicine, listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
You should not take this medicine if you have:
- Severe liver disease, or
- Are taking the following medicines:
- carbamazepine, phenobarbital, phenytoin (antiepileptic medicines)
- St John’s wort (Hypericum perforatum) (herbal product)
- rifampin (antimycobacterial)
- fluconazole (antifungal)
- diltiazem, verapamil (calcium-channel blockers)
- erythromycin (antibiotic)
You should not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering.
If you are not sure whether you should take this medicine, talk to your doctor.
Before you take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you:
- Are pregnant or plan to become pregnant
Nerlynx is not recommended for use during pregnancy. There is no information about the safety of this medicine in pregnant women. However if there is a need to take this medicine when you are pregnant, your doctor will discuss the risks and benefits to you and the unborn baby.
If you become pregnant while taking this medicine, the doctor will assess the potential benefit to you and the risk to the unborn baby, of continuing this medicine.
Women who can become pregnant must use an effective method of contraception, including a barrier method:
- while taking Nerlynx and
- for one month after treatment has finished.
Men must use an effective barrier method of contraception such as a condom:
- while taking Nerlynx and
- for three months after treatment has finished.
- Are breast-feeding or plan to breastfeed
It is not known whether Nerlynx passes into breast milk. Talk to your doctor before taking this medicine if you are breast-feeding or plan to breast-feed because small amounts of this medicine may pass into your breast milk. Your doctor will discuss with you the benefits and risks of taking Nerlynx during this time.
- Have any gastrointestinal problems
Nerlynx can cause diarrhoea when you first start taking it. You should take an anti-diarrhoea medicine called loperamide so that your diarrhoea does not become severe, and to prevent you from getting dehydrated during treatment with Nerlynx.
Talk to your doctor if you cannot take loperamide.
- Have any liver problems
Nerlynx can cause changes in liver function – these are shown in blood tests. Your doctor will do blood tests before and during your treatment with this medicine. Your doctor will stop your treatment with Nerlynx if your liver tests show severe problems.
Use in Children
Unless you are advised by your doctor that it is necessary to take Nerlynx, you should not take this medicine if you are a child or adolescent under 18. The safety of Nerlynx and how effective it is have not been studied in this age group.
Nerlynx with Food and Drink
Do not take grapefruit while you are taking Nerlynx – this includes eating them, drinking the juice or taking a supplement that might contain them.
You should also avoid eating Star fruit, Pomelos and Seville Oranges.
This is because these foods may interact with Nerlynx and can affect how the medicine works.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines. This is because Nerlynx can affect the way some other medicines work. Also some other medicines can affect the way Nerlynx works.
In particular tell your doctor or pharmacist if you are taking any of the following medicines:
- ketoconazole, itraconazole, voriconazole - medicines for fungal infections
- St John’s Wort – a medicine for depression
- carbamazepine – a medicine for seizures
- rifampin - a medicine for tuberculosis (TB)
- digoxin - a medicine for heart problems
- medicines for stomach problems such as:
- lansoprazole, omeprazole or similar medicines called ‘proton pump inhibitors’ or PPIs and ranitidine, cimetidine or similar medicines called ‘H2 receptor antagonists’ are not recommended.
- antacid medicines - the dose of these medicines and Nerlynx should be separated by at least 3 hours.
If any of the above applies to you (or you are not sure), talk to your doctor or pharmacist before taking Nerlynx.
How Nerlynx is taken
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
How much is taken
The recommended dose of Nerlynx is six 40 mg tablets once a day (a total of 240 mg).
How it is taken
Take the tablets whole with food and a glass of water. Do not crush or dissolve. Do not swallow the desiccant (a drying agent used to keep the tablets from becoming moist).
Take all the tablets at about the same time each day, preferably in the morning.
You need to take an anti-diarrhoea medicine when you start Nerlynx.
Nerlynx can cause diarrhoea when you first start taking it. Diarrhoea may be severe, causing you to get dehydrated, unless loperamide is taken to prevent or reduce the diarrhoea.
- Start taking loperamide with the first dose of Nerlynx.
- Your doctor will tell you how to take loperamide.
- Keep taking loperamide during the first two months of Nerlynx treatment. Your doctor will tell you if you need to keep taking loperamide after the first two months to control your diarrhoea.
- While taking loperamide, you and your doctor should try to keep the number of bowel movements that you have at 1 or 2 bowel movements each day
- Your doctor will also tell you if you need to change the dose of Nerlynx because of diarrhoea.
How long it will be taken
The course of treatment is one year.
If too much is taken (overdose)
Immediately telephone your doctor or the Poisons Information Centre (Australia - telephone 13 11 26) for advice or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have used too much Nerlynx, even if there are no signs of discomfort or poisoning.
Some side effects associated with taking more Nerlynx than you should are: diarrhoea, nausea, vomiting and dehydration.
If you forget to take it
- If you forget a dose, wait until the next day before you take the next dose.
- Do not take a double dose to make up for a forgotten dose.
Do not stop taking Nerlynx without talking to your doctor.
If you have any further questions on the use of this medicine, ask your doctor, nurse, or pharmacist.
While You Are Taking Nerlynx
Things you must do
Take Nerlynx for as long as your doctor recommends.
Don't stop taking this medicine unless your doctor advises you to.
If you are about to be started on any new medicine, remind your doctor that you are taking Nerlynx.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
Use a contraceptive to prevent pregnancy during treatment with Nerlynx and for at least one month after your last dose of Nerlynx.
If you become pregnant while taking this medicine, tell your doctor immediately.
Things you must not do
Be careful driving or operating machinery until you know how Nerlynx affects you. Nerlynx has minor or moderate influence on the ability to drive and use machines. The side effects of Nerlynx (for example, dehydration and dizziness resulting from diarrhoea, fatigue, and fainting) may affect how tasks that require judgment, motor or cognitive skills are carried out.
Possible Side Effects
Tell your doctor as soon as possible if you do not feel well while you are taking Nerlynx.
All medicines may have some unwanted side effects, although not everybody gets them. Sometimes they are serious, most of the time they are not. Your doctor has weighed the risks of taking this medicine against the benefits they expect it will have for you.
You may need medical attention if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if you get any of the following side effects:
Symptoms of an allergic reaction which may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin.
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
Diarrhoea
Nerlynx can cause diarrhoea during treatment, which may be reduced or prevented if taken with loperamide or other anti-diarrhoeal medicines. The diarrhoea may be severe, and you may get dehydrated. See the section on How it is taken for more information about the anti-diarrhoea medicine you need to take at the same time as Nerlynx.
Talk to your doctor if:
- you have more than 2 bowel movements in 1 day or you are having diarrhoea that does not go away - they can advise how to control your diarrhoea.
- you feel dizzy or weak from diarrhoea - alternatively go to the hospital immediately.
Liver problems
Nerlynx can cause changes in liver function - these are shown in blood tests. You may or may not have signs or symptoms of liver problems (e.g., yellow skin and/or eyes, dark urine, or light-colour stools). Your doctor will do blood tests before and during your treatment with Nerlynx. Your doctor will stop your treatment with Nerlynx if your liver tests show severe problems.
Tell your doctor if you notice any of the following side effects and they worry you:
Very common side effects – (may affect more than 1 in 10 people):
- stomach pain, feeling or being sick, low appetite
- dry or inflamed mouth, including blisters or mouth ulcers
- rash
- muscle spasms or cramps
- feeling very tired
The above list includes the most common side effects of your medicine.
Common side effects (may affect up to 1 in 10 people):
- burning sensation during urination, and frequent and urgent need to urinate, (may be symptoms of urinary tract infection)
- dehydration
- nosebleed
- mild stomach upset
- dry mouth
- changes in liver blood test results
- nail problems including nail splitting or colour change
- dry skin including cracked skin
- changes in kidney function test
- weight loss
This is not a complete list of side effects. For any unexpected effects while taking Nerlynx, contact your doctor immediately.
If you receive Nerlynx and feel any of the symptoms mentioned above during the treatment, your doctor has to be informed. In case you suffer these symptoms, the Nerlynx dose may be stopped or reduced depending on the severity.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may also occur in some people.
By reporting side effects, you can help provide more information on the safety of this medicine.
After Taking Nerlynx
Storage
Keep your medicine in a cool dry place where the temperature stays below 25°C. Store in the original container and keep the bottle tightly closed in order to protect from moisture.
Do not store Nerlynx or any other medicine in the bathroom or near a sink. Do not leave it on a windowsill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres (about 5 feet) above the ground is a good place to store medicines.
Disposal
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
Product Description
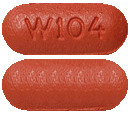
What it looks like
Red film-coated tablet. The tablet is oval shaped and debossed with ‘W104’ on one side and plain on the other side.
Nerlynx film-coated tablets are packaged in a white, high-density polyethylene (HDPE) round bottle with child-resistant, polypropylene closure, and foil induction inner seal for a tamper-evident seal.
An HDPE desiccant canister with 1 g silica gel is enclosed with the tablets in each bottle.
Each bottle contains 133 or 180 film-coated tablets. Not all packs may be marketed.
Ingredients
The active substance is neratinib.
Each film-coated tablet contains neratinib maleate, equivalent to 40 mg neratinib.
The other ingredients are:
- Tablet core: mannitol, microcrystalline cellulose, crospovidone, povidone, colloidal anhydrous silica, magnesium stearate
- Tablet coating: polyvinyl alcohol, titanium dioxide, macrogol 3350, purified talc, iron oxide red
Sponsor
Specialised Therapeutics PM Pty Ltd
Level 2, 17 Cotham Road,
Kew, Victoria, 3101
Ph: 1300 798 820
Fax: 1800 798 829
www.stbiopharma.com
Please check with your pharmacist for the latest Consumer Medicine Information (CMI).
Australian Register Number
1 single pack containing 1 bottle of 133 or 180 tablets:
AUST R 301129
This leaflet was prepared by Specialised Therapeutics PM Pty Ltd
Last revised: 18 October 2021
Published by MIMS March 2022

 If diarrhoea occurs despite prophylaxis, treat with additional anti-diarrhoeals, fluids and electrolytes as clinically indicated. Nerlynx dose interruptions and dose reductions may also be required to manage diarrhoea (see Table 3).
If diarrhoea occurs despite prophylaxis, treat with additional anti-diarrhoeals, fluids and electrolytes as clinically indicated. Nerlynx dose interruptions and dose reductions may also be required to manage diarrhoea (see Table 3). If diarrhoea occurs, treat with anti-diarrhoeals, fluids and electrolytes as clinically indicated. Nerlynx dose interruptions and dose reductions may also be required to manage diarrhoea.
If diarrhoea occurs, treat with anti-diarrhoeals, fluids and electrolytes as clinically indicated. Nerlynx dose interruptions and dose reductions may also be required to manage diarrhoea.





 Figure 1 shows the Kaplan-Meier plots for iDFS for the ITT population of study ExteNET (3004).
Figure 1 shows the Kaplan-Meier plots for iDFS for the ITT population of study ExteNET (3004). Figure 2 shows the Forrest Plot for iDFS by pre-specified patient subgroup.
Figure 2 shows the Forrest Plot for iDFS by pre-specified patient subgroup. Approximately 75% of patients were re-consented for extended follow-up beyond 24 months. This exploratory analysis confirms that the iDFS results at 5 years are durable and consistent with the 2-year iDFS results.
Approximately 75% of patients were re-consented for extended follow-up beyond 24 months. This exploratory analysis confirms that the iDFS results at 5 years are durable and consistent with the 2-year iDFS results. Of the 2840 women in the ITT population (Nerlynx, n = 1420; placebo, n = 1420), 1334 had HR+ tumours and were randomised to start study treatment within 1 year of completing trastuzumab (Nerlynx, n = 670; placebo, n = 664).
Of the 2840 women in the ITT population (Nerlynx, n = 1420; placebo, n = 1420), 1334 had HR+ tumours and were randomised to start study treatment within 1 year of completing trastuzumab (Nerlynx, n = 670; placebo, n = 664). Chemical name: (E)-N-{4-[3-chloro-4-(pyridin-2-yl methoxy) anilino]-3-cyano-7-ethoxyquinolin-6-yl}-4-(dimethylamino)but-2-enamide maleate.
Chemical name: (E)-N-{4-[3-chloro-4-(pyridin-2-yl methoxy) anilino]-3-cyano-7-ethoxyquinolin-6-yl}-4-(dimethylamino)but-2-enamide maleate.