What is in this leaflet
This leaflet answers some common questions about Neulactil.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor or pharmacist has weighed the risks of you taking Neulactil against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Neulactil is used for
The active ingredient of Neulactil is periciazine, one of a group of medicines called phenothiazines.
Neulactil is used to treat patients who feel very anxious and/or tense.
It is used in patients to control symptoms such as impulsiveness and aggression.
It is also used in patients with severe mental conditions when a person loses contact with reality and is unable to think and judge clearly.
Your doctor may have prescribed Neulactil for another reason.
Use in children aged below 1 is contraindicated and is not recommended in children aged below 3. In children aged between 3-6 it should be used only in exceptional circumstances.
Ask your doctor or pharmacist if you have any questions about why Neulactil has been prescribed for you.
Before you take it
When you must not take it
Do not take Neulactil if you have an allergy to Neulactil, any other drugs from the phenothiazine family, and/or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include:
- asthma, wheezing or shortness of breath
- swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing
- hives, itching or skin rash
- fainting
Do not take Neulactil if you have any of the following-
- circulatory disorders
- blood or bone marrow disorders
- a history of high pressure in the eyes (certain types of glaucoma)
- if you are receiving local anaesthetics around the spinal cord
- uncontrolled fitting disorders
- liver problems
- phaeochromocytoma (rare tumour of the adrenal gland)
- difficulty passing urine or prostate problems
- If you are taking medicines used to treat Parkinson's disease (disease of the brain that affects movement)
Do not take Neulactil after the expiry date (EXP) printed on the pack. If you take this medicine after the expiry date has passed, it may not work (as well).
Do not take Neulactil if the packaging is torn or shows signs of tampering.
Do not give Neulactil to a child under the age of 1. There is a possible link to Sudden Infant Death Syndrome (SIDS)
If you are not sure whether you should start taking Neulactil, contact your doctor or pharmacist.
Before you start to take it
Tell your doctor if you have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes
Tell your doctor if you are breast feeding, pregnant or trying to become pregnant. Your doctor will discuss the possible risks and benefits of using Neulactil during pregnancy and lactation.
Tell your doctor if you have or have had any medical conditions, especially the following:
- kidney problems
- epilepsy fits
- Parkinson's disease
- decreased thyroid activity
- heart failure, other problems with the heart or blood vessels
- blood clots or a history of blood clots
- bowel problems
- dementia
- diabetes
- tumour of the adrenal gland
- muscle weakness (myasthenia gravis)
- certain types of glaucoma- high pressure in the eyes
- prostate problems
- low potassium levels
- brain damage
If you have not told your doctor about any of the above, tell them before you start taking Neulactil.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Neulactil may interfere with each other.
These include:
- sedatives, medicines to help you sleep or to calm you down.
- sedative antihistamines (medicines used to prevent or relieve the symptoms of allergy)
- medicines used to treat high blood pressure.
- medicines used to treat mental illness.
- medicines used to treat a fast or irregular heart beat e.g. amiodarone, quinidine, disopyramide.
- medicines that can slow your heart beat e.g. diltiazem, verapamil.
- medicines that can reduce potassium levels in the blood e.g. diuretics, laxatives.
- other medicines that can affect your heart rate e.g. methadone, pentamidine.
- adrenaline (epinephrine) (sends more oxygen to brain and muscles)
- desferrioxamine (a medicine used to remove excess iron from the body)
- lithium (a medicine used to treat mood swings and some types of depression)
- medicines metabolised by CYP2D6 enzymes such as amitriptyline.
- anticholinergics, medicines used to relieve stomach cramps or spasms, to prevent travel sickness and to treat Parkinson's disease.
These medicines may be affected by Neulactil or may affect how well it works. You may need different amounts of your medicine, or you may need to take different medicines. Your doctor or pharmacist will advise you.
How to take it
How much to take
Your doctor or pharmacist will tell you how many tablets you will need to take each day. This depends on your condition and whether or not you are taking any other medicines.
Follow all directions given to you by your doctor and pharmacist carefully. These directions may differ from the information contained in this leaflet.
If you do not understand the instructions given to you, ask your doctor or pharmacist for help.
How to take it
Swallow the tablets with a glass of water.
When to take it
Take Neulactil at about the same time each day. Taking your tablets at the same time each day will have the best effect. It will also help you remember when to take the tablets.
It does not matter if you take Neulactil before or after food.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
How long to take it
Neulactil helps control your condition, but does not cure it. Therefore you must take Neulactil every day. Continue taking the tablets for as long as your doctor or pharmacist tells you.
Do not stop using it unless your doctor or pharmacist tells you to - even if you feel better.
If you take too much (overdose)
If you take too much Neulactil you are more likely to experience side effects listed below.
Immediately telephone your doctor or pharmacist or the Poisons Information Centre (telephone Australia 13 11 26, New Zealand 0800 POISON or 0800 764 766), or go to accident and emergency at your nearest hospital, if you think that you or anyone else may have taken too much Neulactil.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking Neulactil.
If you become pregnant while taking Neulactil, tell your doctor.
Things you must not do
Do not give Neulactil to anyone else, even if they have the same condition as you.
Do not take Neulactil to treat any other complaints unless your doctor tells you to.
Do not stop taking Neulactil, or lower or raise the dosage, without checking with your doctor.
Things to be careful of
Neulactil may cause you to become extra sensitive to sunlight. Make sure you avoid exposure and protect your eyes from strong sunlight.
Neulactil may put you at risk of hyperthermia or hypothermia particularly during hot or very cold weather if you are over the age of 65 years.
Be careful driving or operating machinery until you know how Neulactil affects you. As with other medicines of this kind, Neulactil may cause dizziness, light-headedness, and drowsiness in some people. Make sure you know how you react to Neulactil before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed. If this occurs do not drive.
Alcohol should be avoided while on treatment with Neulactil. If you drink alcohol, dizziness or light-headedness may be worse.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Neulactil.
Neulactil helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects. If you are over 65 years of age you may have an increased chance of getting side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- drowsiness
- agitation or aggressiveness
- insomnia
- vomiting
- nausea
- constipation
- diarrhoea
- dizziness, especially on standing up from a sit down or lying position
- nasal stuffiness
- dry mouth (sometimes with mouth infections)
- difficulty passing urine
- sweating
- symptoms of sunburn (such as redness, itching, swelling, blistering) which may occur more quickly than normal
- unusual secretion of breast milk
- growth of breasts in males
- absence or irregular menstrual periods
- impotence
- false positive pregnancy tests
- changes in libido
- inability to ejaculate
- swelling of hands, ankles, feet
- increased appetite and weight gain
- mood changes or feeling anxious
Tell your doctor or pharmacist immediately if you notice any of the following:
- fever
- severe confusion
- skin rash
- severe pain in the stomach with bloating, gut cramps and vomiting
- yellowing of the skin and or the eyes
- changes in the way the heart beats
- shallow breathing
- frequent infections such as fever, severe chills, sore throat, mouth ulcers
- distortion of the body
- uncontrollable twitching, jerking or writhing movements
- restlessness
- lack of normal muscle movement
- stiffness or tightness in the arms or legs
- blurred vision
- aggravation of glaucoma
- abnormal pigmentation on certain areas of the eye
- difficulty breathing
- altered consciousness
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty breathing or swallowing
These may be serious side effects. You may need urgent medical attention. Serious side effects are rare.
Other side effects not listed above may occur in some patients. Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Neulactil tablets should not be frequently handled. Care should be taken to minimise contact of Neulactil tablets with the skin.
After taking it
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they will not keep as well.
Keep your tablets in a cool dry place protected from light where the temperature stays below 25°C.
Do not store Neulactil or any other medicine in the bathroom or near a sink.
Do not leave it in the car on hot days or on windowsills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking Neulactil or the tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
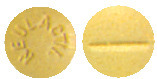
What it looks like
Neulactil 2.5mg tablets are yellow, scored, and marked 'NEULACTIL'. They are available in packs of 100 tablets.
Neulactil 10mg tablets are yellow, scored, and marked '10'. They are available in packs of 100.
Neulactil tablets contain:
- periciazine 2.5 or 10mg (active ingredient)
- cellulose microcrystalline
- lactose monohydrate
- wheat starch
- colloidal anhydrous silica
- magnesium stearate
Distributor
sanofi-aventis australia pty ltd
12-24 Talavera Road,
Macquarie Park, NSW 2113
sanofi-aventis new zealand limited
Level 8, 56 Cawley Street Ellerslie
Auckland
Australian Registration Numbers-
Neulactil 2.5mg AUST R 27524
Neulactil 10mg AUST R 27523
This leaflet was updated in August 2017
neulactil-ccdsv3-cmiv10-aug17
Published by MIMS October 2017