What is in this leaflet
This leaflet answers some common questions about NITYR tablets.
It does not contain all of the available information. Some of the information it contains may not apply to you. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. In deciding to give you NITYR, your doctor has weighed the risks of you taking NITYR against the expected benefits it will have for you.
Always follow the instructions that your doctor and pharmacist give you about NITYR.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
What NITYR are used for
NITYR contains the medicine Nitisinone. Nitisinone belongs to a group of medicines called ‘other alimentary and metabolism products’.
NITYR is used for the treatment of a disease called hereditary tyrosinaemia type 1. In this disease the body is unable to completely break down the amino acid tyrosine. Harmful substances will be formed and accumulated in the body.
NITYR block the breakdown of tyrosine and by doing so the harmful substances are not formed. However, tyrosine will remain in the body and therefore a special diet (with low tyrosine and phenylalanine content) must be followed when taking NITYR.
Your doctor may have prescribed this medicine for another use. If you want more information, ask your doctor.
NITYR is not addictive.
NITYR is only available on a doctor's prescription
Before you take NITYR
You should not take NITYR if:
- you are allergic to Nitisinone or any of the ingredients listed under 'Product Description' at the end of this leaflet. Signs of allergic reactions may include itchy skin, rash, shortness of breath and swelling of the face or tongue.
- you are breastfeeding
- the packaging shows signs of tampering.
- the expiry date on the pack has passed.
Before you start to take NITYR
You must tell your doctor if:
You are pregnant or intend to become pregnant. Your doctor will discuss the possible risks and benefits of taking NITYR during pregnancy.
- The use of NITYR during breast feeding has not been investigated. Ask your doctor for advice about breast feeding.
- Hypersensitive to the active substance or to any of the excipients
If you have not told your doctor about any of the above, tell him/her before you start taking NITYR.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food store.
If you are unsure about any medicine you are taking you should check with your doctor or pharmacist. They will have more information on medicines to be careful with or avoid while taking NITYR.
How to take NITYR
It is important to follow the directions that your doctor has given to you.
How much to take
Your doctor will tell you how many tablets to take each day.
Take NITYR only as prescribed by your doctor and follow his or her directions carefully. They may differ from the information contained in this leaflet.
When to take it
The usual daily dose is 1 mg/kg body weight per day divided in morning and evening administrations.
Take your first dose in the morning. Take your second dose in the evening.
Swallow the tablets whole with a full glass of water.
NITYR may be taken with or without food.
If you have problems with swallowing the tablets, tablets may be disintegrated in water inside an oral syringe or crushed between two spoons and mixed with applesauce. Your doctor will tell you if and how you can disintegrate or crush NITYR and how many tablets you should use.
Instructions for this process are provided at the end of this leaflet.
How long to take it
Continue taking NITYR for as long as your doctor tells you.
If you forget to take it
Do not take a double dose to make up for the dose that you missed.
If you take too much (overdose)
Telephone your doctor or Poisons Information Centre (13 11 26) if you think that you have taken more than you should.
While you are taking NITYR
Things you must do
It is very important that you stay on the special diet, with low tyrosine and phenylalanine content, that your doctor recommends. If you do not understand the instructions on your diet, ask your doctor for help.
Make sure that all of your doctors and pharmacists know about your use of NITYR. Remind them if any new medicines are about to be started.
If you become pregnant while taking this medicine, tell your doctor immediately.
Be sure to keep all of your doctor’s appointments so your progress can be checked.
- Your Doctor will test your blood to check if the amounts of NITYR given are enough and to make sure that there are no possible side effects causing blood disorders.
- Your doctor will also check your liver regularly as the disease can affect the liver.
- Your doctor will also check on your general development.
Things you must not do
Do not use NITYR to treat any complaint other than that directed by your doctor. It may not be safe to use NITYR for another complaint.
Do not give NITYR to someone else even if their symptoms are the same. It may not be safe for another person to use NITYR.
Things to be careful of
Be careful driving, operating machinery or doing jobs that require you to be alert until you know how this medicine affects you.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking NITYR.
Like other medicines NITYR can cause some side effects. Most are likely to be minor and temporary. However, some may be serious and need medical attention.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor immediately if you notice any of the following:
- different eye symptoms as listed below:
- opacity in the cornea
- inflammation in the cornea
- inflammation in the eye
- inflammation in the eyelid
- sensitivity to light
- eye pain
- rash, itching or other skin disorders
- headache, abdominal pain, constipation, diarrhoea
There may be other side effects that your doctor will carefully monitor by taking blood samples. These are:
- reduced number of platelets and white blood cells
- shortage of certain white blood cells (granulocytopenia)
- increased number of white blood cells
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything else that is making you feel unwell. Do not be alarmed by this list of possible side effects. You may not experience any of them.
After using NITYR
Storage
- Keep NITYR in their bottle until it is time to take your dose. If you take them out of their container, they may not keep well.
- Keep NITYR in a dry place at room temperature below 25°C. Store the tablets in the original bottle. Protect from light.
- Do not leave it in the car on hot or cold days. Heat and dampness can destroy some medicines.
- Keep NITYR where children cannot reach it.
Do not use after the expiry date which is stated on the carton and bottle label after “EXP’’.
Disposal
If your doctor tells you to stop taking NITYR, ask your pharmacist what to do with any tablets that are left over.
Product description
What it looks like
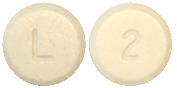
NITYR are white to beige, round, flat tablets, which may display light yellow to brown speckles, marked with “L” on one side and the strength “2”, “5” or “10” on the other side.
NITYR are available in plastic square bottles with a childresistant tamper-evident closure. Each bottle contains 60 tablets. Each pack (carton) contains 1 bottle.
AUST R 288126, 288127, 288128
Active Ingredient:
Each NITYR (nitisinone) tablet contains 2 mg, 5 mg or 10 mg nitisinone.
Other Ingredients:
Glyceryl dibehenate
Lactose monohydrate.
Manufacturer
NITYR™ is supplied in Australia by:
Orpharma Pty Ltd
Level 1,
530 Little Collins St
Melbourne VIC 3000
This leaflet was prepared in September, 2024.
Instructions for administration of the product
The following instructions explain how to take NITYR tablets using an oral syringe if you are unable to swallow the tablet/s.
PLEASE READ ALL THE INSTRUCTIONS CAREFULLY BEFORE YOU START TAKING NITYR TABLETS USING AN ORAL SYRINGE.
- Only 1 or 2 NITYR tablets can be prepared in an oral syringe at one time.
- Use a 5 mL oral syringe with a cap to prepare NITYR tablets in an oral syringe. Ask your pharmacist for your oral syringe. You may need more than one 5 mL oral syringe if you take more than 2 NITYR tablets for your prescribed dose.
- Clean your hands well before preparing NITYR tablets using an oral syringe.

How to prepare and take 1 NITYR and 2 NITYR tablets using a 5 mL oral syringe:
- Remove the plunger and cap from the 5-mL oral syringe, insert one OR two tablets according to your doctor’s advice and replace the plunger.

- Draw up 2.6 mL for one tablet OR 5 mL for two tablets of room temperature water.

- Cap the oral syringe and leave it for at least 60 minutes.

- After 60 minutes, turn the oral syringe up and down for at least 30 seconds.

- Inspect the syringe to ensure the tablet/s has/have disintegrated before administration to the patient. Administer immediately, but only if the tablet/s has/have fully disintegrated.
- If the tablet/s is/are not fully disintegrated, leave the oral syringe for an additional 10 minutes. Before administration to the patient, turn the oral syringe up and down for 30 seconds to re-suspend the particles. Inspect the syringe again to ensure the tablet/s has/have disintegrated prior to administration to the patient. Do not administer unless the tablet/s has/have fully disintegrated.
- Administer immediately. However, if this is not possible, the suspension can be stored at room temperature in the capped oral syringe, protected from direct sunlight for up to 24 hours after adding water to the tablet. Discard after 24 hours.
- Uncap the oral syringe and administer the suspension in the patient’s mouth. To facilitate full administration, avoid pressing the plunger to the end of the oral syringe and leave a gap between the plunger and the oral syringe.

- Rinse the oral syringe by drawing up 2 mL of water. Cap the oral syringe and shake it well for 10 seconds to suspend any remaining particles.

- Uncap the oral syringe and administer the suspension into the patient’s mouth, this time fully pressing the plunger and ensuring the syringe is empty and no particles are left in the tip of the syringe.

- After use, remove the plunger from the oral syringe barrel. Rinse the oral syringe with water after each use and let it dry. Do not replace the plunger into the barrel of the oral syringe until ready to use again to allow it to dry. Do not throw away the oral syringe.
How to prepare and take more than 2 NITYR tablets using an oral syringe:
If more than two NITYR tablets are needed for the prescribed dose, prepare and take the prescribed dose following the instructions in “How to prepare and take 1 NITYR and 2 NITYR tablets using a 5 mL oral syringe”. You may need an extra oral syringe.
The following instructions explain how to crush NITYR tablets in applesauce if you are unable to swallow the tablet/s.
How to prepare and take NITYR tablets mixed in applesauce:
- Measure around one teaspoon of applesauce and transfer it into a clean glass.
- Take out two metal teaspoons. Position one NITYR tablet between two metal teaspoons and apply light pressure on the top spoon. The two teaspoons should overlap each other. Always crush one tablet at a time.
- Press and rotate the two teaspoons against each other repeatedly until the whole tablet is crushed into a fine powder.
- Carefully transfer the resulting powder to the applesauce in the glass. Make sure all the powder is transferred and no powder is left on the teaspoon.
- If more than one tablet is needed, repeat the procedure starting in Step 2 and collect all the resulting powder together in the glass.
- Mix the powder into the applesauce until all the powder is dispersed.
- Give the entire NITYR tablet-applesauce mixture to the patient’s mouth using a teaspoon. The mixture should be given immediately. If this is not possible, the mixture can be stored at room temperature, out of direct sunlight, for up to 2 hours after adding the powder to the applesauce. Discard any mixture after 2 hours.
- To make sure that there is no leftover applesauce mixture in the glass, add another teaspoon of applesauce to the glass and mix. Ensure any remaining applesauce is mixed well with the extra applesauce.
- Give the additional NITYR tablet-applesauce mixture immediately to the patient’s mouth using a spoon.
Published by MIMS November 2024







 Nitisinone treatment leads to normalised porphyrin metabolism with normal erythrocyte PBG - synthase activity and urine 5-ALA, decreased urinary excretion of succinylacetone, increased plasma tyrosine concentration and increased urinary excretion of phenolic acids. Available data from a clinical study indicates that in more than 90% of the patients urine succinylacetone was normalized during the first week of treatment. Succinylacetone should not be detectable in urine or plasma when the nitisinone dose is properly adjusted.
Nitisinone treatment leads to normalised porphyrin metabolism with normal erythrocyte PBG - synthase activity and urine 5-ALA, decreased urinary excretion of succinylacetone, increased plasma tyrosine concentration and increased urinary excretion of phenolic acids. Available data from a clinical study indicates that in more than 90% of the patients urine succinylacetone was normalized during the first week of treatment. Succinylacetone should not be detectable in urine or plasma when the nitisinone dose is properly adjusted.
