1 Name of Medicine
Opicapone.
2 Qualitative and Quantitative Composition
Each hard capsule contains 50 mg of opicapone as active substance.
Excipients with known effect.
Each hard capsule contains 156 mg of lactose monohydrate and approximately 76 mg of gelatine which contains sulfites as a residue.
For the full list of excipients, see Section 6.1 List of Excipients.3 Pharmaceutical Form
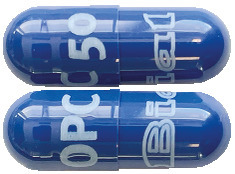
Hard capsules.
Dark blue capsules, size 1 (approximately 19 mm) imprinted "OPC 50" on the cap and "Bial" on the body.4.1 Therapeutic Indications
Ongentys is indicated as adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors (DDCI) in adult patients with Parkinson's disease and end-of-dose motor fluctuations who cannot be stabilised on those combinations.
4.2 Dose and Method of Administration
Dosage.
The recommended dose of opicapone is 50 mg.
Ongentys should be taken once daily at bedtime, preferably without food, at least one hour before or after levodopa combinations.
Missed dose.
If one dose is missed, the next dose should be taken as scheduled. The patient should not take an extra dose to make up for the missed dose.
Method of administration.
Oral use.
The capsules should be swallowed whole with water. Ongentys shall be taken preferably on an empty stomach (that is two hours before or two hours after a meal).
Dosage adjustment.
Antiparkinsonian therapy.
Ongentys is to be administered as an adjunct to levodopa treatment and enhances the effects of levodopa. Hence, it is often necessary to adjust levodopa dose by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating the treatment with opicapone according to the clinical condition of the patient (see Section 4.4 Special Warnings and Precautions for Use).
Renal impairment.
No dose adjustment is necessary in patients with renal impairment, as opicapone is not primarily excreted by the kidney (see Section 5.2 Pharmacokinetic Properties).
Hepatic impairment.
Ongentys is not recommended in patients with hepatic impairment or hepatic cirrhosis (Child-Pugh Class A, B, C).
The bioavailability of opicapone was significantly higher in patients with moderate chronic hepatic impairment (see Section 5.2 Pharmacokinetic Properties).
There is no clinical experience in patients with mild hepatic impairment (Child-Pugh Class A), and in patients with severe hepatic impairment (Child-Pugh Class C).
Paediatric population.
There is no relevant use of Ongentys in the paediatric population with Parkinson's disease and motor fluctuations.
Elderly.
No dose adjustment is needed for elderly patients (see Section 5.2 Pharmacokinetic Properties). Caution must be exercised in patients ≥ 75 years of age as there is limited experience in this age group.4.3 Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in Section 6.1 List of Excipients.
Phaeochromocytoma, paraganglioma, or other catecholamine secreting neoplasms.
History of neuroleptic malignant syndrome and/or non-traumatic rhabdomyolysis.
Concomitant use with monoamine oxidase (MAO-A and MAO-B) inhibitors (e.g. phenelzine, tranylcypromine and moclobemide) other than those for the treatment of Parkinson's disease (see Section 4.5 Interactions with Other Medicines and Other Forms of Interactions).
4.4 Special Warnings and Precautions for Use
Dose adjustments of antiparkinsonian therapy.
Ongentys is to be administered as an adjunct to levodopa treatment. Hence, the precautions valid for levodopa treatment should also be taken into account for Ongentys. Opicapone enhances the effects of levodopa. To reduce levodopa-related dopaminergic adverse reactions (e.g. dyskinesia, hallucinations, nausea, vomiting and orthostatic hypotension), it is often necessary to adjust the daily dose of levodopa by extending the dosing intervals and/or reducing the amount of levodopa per dose within the first days to first weeks after initiating treatment with Ongentys, according to the clinical condition of the patient (see Section 4.2 Dose and Method of Administration).
There is limited data available regarding the pharmacokinetic effects of Ongentys on sustained release formulation of levodopa. Thus, appropriate caution is advised.
If Ongentys is discontinued it is necessary to adjust the dosing of the other antiparkinsonian treatments, especially levodopa, to achieve a sufficient level of control of the symptoms.
Psychiatric disorders.
Patients and caregivers should be made aware that impulse control disorders including pathological gambling, increased libido, hypersexuality, compulsive spending or buying, binge eating and compulsive eating can occur in patients treated with dopamine agonists and/or other dopaminergic treatments. Patients should be monitored regularly for the development of impulse control disorders and review of treatment is recommended if such symptoms develop.
Others.
Increases in liver enzymes were reported in studies with nitrocatechol inhibitors of catechol-O-methyltransferase (COMT). For patients who experience progressive anorexia, asthenia and weight decrease within a relatively short period of time, a general medical evaluation including liver function should be considered.
Ischemic heart diseases were frequently observed in case of use of other substances having the same mechanism of action as opicapone (COMT inhibition).
Excipients.
Ongentys contains lactose. Patients with rare hereditary problems of galactose intolerance, the total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product.
Ongentys contains less than 1 mmol sodium (23 mg) per capsule, that is to say essentially 'sodium-free'.
Use in the elderly.
Caution must be exercised in patients ≥ 75 years of age as there is limited experience in this age group (see Section 4.2 Dose and Method of Administration).
Paediatric use.
No data available.
Effects on laboratory tests.
No data available.4.5 Interactions with Other Medicines and Other Forms of Interactions
Monoamino oxidase (MAO) inhibitors.
Combination of opicapone and MAO inhibitors could result in inhibition of the majority of the pathways responsible for the metabolism of catecholamines. Because of this, concomitant use of opicapone with MAO inhibitors (e.g. phenelzine, tranylcypromine, linezolid and moclobemide) other than those for the treatment of Parkinson's disease is contraindicated (see Section 4.3 Contraindications).
Concomitant use of opicapone and MAO inhibitors for the treatment of Parkinson's disease, e.g. rasagiline (up to 1 mg/day) and selegiline (up to 10 mg/day in oral formulation or 1.25 mg/day in buccal absorption formulation), is permissible.
There is no experience with opicapone when used concomitantly with the MAO-B inhibitor safinamide. Therefore, their concomitant use should be considered with appropriate caution.
Medicinal products metabolised by COMT.
Opicapone may interfere with the metabolism of medicinal products containing a catechol group that are metabolised by COMT (e.g. rimiterol hydrobromide, isoprenaline, adrenaline (epinephrine), noradrenaline (norepinephrine), dopamine, dopexamine or dobutamine) leading to potentiated effects of these medicinal products. Careful monitoring of patients being treated with these medicinal products is advised when opicapone is used.
Tricyclic antidepressants and noradrenaline (norepinephrine) re-uptake inhibitors.
There is limited experience with opicapone when used concomitantly with tricyclic antidepressants and noradrenaline (norepinephrine) re-uptake inhibitors (e.g. venlafaxine, maprotiline and desipramine). Thus, their concomitant use should be considered with appropriate caution.
Hormonal contraceptives.
The potential for drug interactions between opicapone and hormonal contraceptives had not been assessed. Female patients on oral contraceptives, while on treatment with opicapone should be informed that additional non-hormonal methods of contraception are to be used.
Influence of opicapone over other substances.
Warfarin.
After the co-administration of multiple doses of 50 mg of opicapone QD and a single dose of 25 mg of warfarin, the Cmax of warfarin S and R (CYP2C9, 3A4 end 1A2 substrates) remained unchanged. A reduction of 13.7% and 14.8% of the - AUC of warfarin S and R (respectively) was observed in the presence of opicapone.
CYP2C8 and OATP1B1 substrates.
Opicapone is a weak inhibitor of CYP2C8 (with an estimated Ki of 0.9 microgram/mL) and of OATP1B1, under in vitro testing.
A clinical study conducted in healthy subjects showed that there were no significant changes in the total plasma exposure of repaglinide, a CYP2C8 and OATP1B1 substrate, when administered concomitantly with opicapone 50 mg, following repeated once-daily administration.
In vitro studies.
In in vitro studies in human hepatic microsomes, minor inhibition of CYP1A2 and CYP2B6 was observed. All reductions in activity essentially occurred at the highest concentration of opicapone (10 microgram/mL).
Opicapone inhibited CYP2C8 activity with an estimated Ki of 0.9 microgram/mL.
Opicapone reduced CYP2C9 activity through competitive/ mixed type mode of inhibition.
Opicapone and/or BIA 9-1103 inhibits OAT1, OAT3, OATP1B1, OATP1B3 and BSEP in vitro.
Considering the plasma free fractions of opicapone and BIA 9-1103 detected in clinical studies, no interaction is expected in OAT1, OAT3, OATP1B1, OATP1B3, OCT1, OCT2, BCRP, P-gp/MDR1, BSEP, MATE1 and MATE2-K transporters. Inhibition of OATP1B1 cannot be ruled out.
Influence of other substances over opicapone.
In vitro studies have shown that opicapone is not transported by OATP1B1, but is transported by OATP1B3, and efflux transported by P-gp and BCRP. BIA 9-1103, its major metabolite, was transported by OATP1B1 and OATP1B3, and efflux transported by BCRP, but is not a substrate for the P-gp/MDR1 efflux transporter.
The effects of the inhibitors of OATP1B3, Pgp or BCRP on the pharmacokinetics of OPC and BIA 9-1103 were not studied.
Quinidine.
A study conducted in healthy volunteers showed that when a single dose of 50 mg opicapone was co-administered (within 1 hour) with a single dose of quinidine (600 mg), systemic exposure of opicapone decreased by 37% AUC0-tlast and 30% Cmax. Thus, particular consideration should be given to cases where quinidine needs to be administered together with opicapone as their co-administration should be avoided.4.6 Fertility, Pregnancy and Lactation
Effects on fertility.
The effects of opicapone on fertility in humans have not been studied.
In rats, opicapone did not affect male and female fertility or prenatal development at exposure levels 16-17 times the therapeutic exposure in humans.
(Category B2)
There are no or limited amount of data from the use of opicapone in pregnant women. Opicapone and/or its metabolites crossed the placenta in rats. Animal studies are insufficient with respect to reproductive toxicity. Ongentys is not recommended during pregnancy and in women of childbearing potential not using contraception.
In rats opicapone was not teratogenic at oral doses up to 1000 mg/kg/day (exposure levels 31 times the therapeutic exposure in humans). In pregnant rabbits, opicapone was less well tolerated resulting in maximum systemic exposure levels around or below the therapeutic range. Although embryo-fetal development was not negatively influenced in rabbits, the study is not considered predictive for human risk assessment. During studies on pre- and post-natal development in rats, no adverse effect was observed on the F0 generation at oral doses up to 1000 mg/kg/day, corresponding to a safety margin of 31 times the therapeutic exposure in humans.
Levels of opicapone-related material in the milk of lactating rats were equivalent to those in plasma. It is unknown whether opicapone or its metabolites are excreted into human milk. A risk to the newborns/infants cannot be excluded. Breast-feeding should be discontinued during treatment with Ongentys.4.7 Effects on Ability to Drive and Use Machines
Opicapone in association with levodopa may have major influence on the ability to drive and use machines. Opicapone may, together with levodopa, cause dizziness, symptomatic orthostatism and somnolence. Therefore, caution should be exercised when driving or using machines.
4.8 Adverse Effects (Undesirable Effects)
Summary of the safety profile.
The safety of opicapone was evaluated in two Phase 3 double-blind, placebo and active controlled studies in 1,027 randomized adult patients with Parkinson's disease treated with levodopa/DDCI (alone or in combination with other antiparkinsonian drugs) and end-of-dose motor fluctuations for up to 15 weeks. At screening, the mean age was similar in all treatment groups in both studies, ranging between 61.5 and 65.3 years.
Common adverse reactions.
Adverse reactions that occurred in the pooled controlled trials at an incidence of at least 3% in any treatment group and greater than placebo is presented in Table 1. The most common adverse reactions (incidence at least 4% in total OPC) were dyskinesia, constipation, insomnia, dry mouth.

Other adverse reactions.
Opicapone use compared with placebo was also associated with slightly higher frequencies of the following adverse reactions:
Adverse reactions are presented by System Organ Class and frequency. Frequency are indicated in a descending order defined as follows: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), not known (cannot be estimated from the available data).
Within each category of frequency, the adverse reactions are indicated by descending order of severity.
Metabolism and nutrition disorders.
Uncommon: hypertriglyceridemia, decreased appetite.
Psychiatric disorders.
Common: hallucination, hallucination visual, abnormal dreams.
Uncommon: hallucination auditory, depression, anxiety, nightmare, sleep disorder.
Nervous system disorders.
Common: headache.
Uncommon: syncope, hyperkinesia, dysgeusia.
Eye disorders.
Uncommon: dry eye.
Ear and labyrinth disorders.
Uncommon: ear congestion.
Vascular disorders.
Common: orthostatic hypotension.
Uncommon: hypotension.
Respiratory, thoracic and mediastinal disorders.
Uncommon: dyspnoea.
Gastrointestinal disorders.
Common: vomiting.
Uncommon: abdominal pain, abdominal pain upper, dyspepsia, abdominal distention.
Musculoskeletal and connective tissue disorders.
Common: muscle spasms.
Uncommon: muscle twitching, musculoskeletal stiffness, myalgia, pain in extremities.
Renal and urinary disorders.
Uncommon: chromaturia, nocturia.
Adverse reactions from post-marketing reports.
The following adverse reactions have been identified during post approval use of Ongentys. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
Psychiatric disorders.
Unknown: agitation, psychotic disorder, anxiety, confusional state.
Nervous system disorders.
Unknown: balance disorder, hyperkinesia tremor.
Gastrointestinal disorders.
Common: nausea.
Unknown: diarrhoea.
General disorders and administration site conditions.
Unknown: fatigue, malaise.
Injury, poisoning and procedural complications.
Uncommon: fall.
Reporting of suspected adverse reactions.
Reporting suspected adverse reactions after registration of the medicinal product is important. It allows continued monitoring of the benefit-risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions at www.tga.gov.au/reporting-problems.4.9 Overdose
There is no known specific antidote. Symptomatic and supportive treatment should be administered as appropriate. Removal of opicapone by gastric lavage and/or inactivation by administering activated charcoal should be considered.
For information on the management of overdose, contact the Poisons Information Centre on 131126 (Australia).
5 Pharmacological Properties
5.1 Pharmacodynamic Properties
ATC code: N04BX04.
Mechanism of action.
Opicapone is a peripheral, selective and reversible catechol-O-methyltransferase (COMT) inhibitor endowed with a high binding affinity (sub-picomolar) that translates into a slow complex dissociation rate constant and a long duration of action (> 24 hours) in vivo.
In the presence of a DOPA decarboxylase inhibitor (DDCI), COMT becomes the major metabolising enzyme for levodopa, catalysing its conversion to 3-O-methyldopa (3-OMD) in the brain and periphery. In patients taking levodopa and a peripheral DDCI, such as carbidopa or benserazide, opicapone increases levodopa plasma levels thereby improving the clinical response to levodopa.
Pharmacodynamic effects.
Opicapone showed a marked (> 90%) and long-lasting (> 24 hours) COMT inhibition in healthy subjects after administration of 50 mg opicapone.
At steady state, in healthy volunteers, following multiple oral administration of immediate-release 100/25 mg levodopa/carbidopa administered three times a day, 10 h after an opicapone 50 mg evening dose the mean extent of levodopa systemic exposure over 24 h (AUC0-24) significantly increased approximately 53% compared to placebo.
Clinical trials.
The efficacy and safety of opicapone has been demonstrated in two Phase 3 double-blind, placebo and active (Study 1 only) controlled studies in 1,027 randomized adult patients with Parkinson's disease treated with levodopa/DDCI (alone or in combination with other antiparkinsonian medicinal products) and end-of-dose motor fluctuations for up to 15 weeks. At screening, the mean age was similar in all treatment groups in both studies, ranging between 61.5 and 65.3 years. Patients had disease severity stages 1 to 3 (modified Hoehn and Yahr) at ON, were treated with 3 to 8 daily doses of levodopa/DDCI and had a daily average OFF-time of at least 1.5 hours. In both studies, 783 patients were randomized with 25 mg or 50 mg of opicapone or placebo. In Study 1, 115 patients were treated with 50 mg of opicapone and 122 patients were treated with 200 mg of entacapone (active comparator). The majority of patients treated in both pivotal studies were treated with immediate-release levodopa/DDCI. There were 60 patients in the combined Phase 3 studies who were predominantly using controlled-release levodopa (i.e. > 50% of their levodopa/DDCI formulations), 48 of whom were treated solely with controlled-release formulations of levodopa. Although there is no evidence that either the efficacy or safety of opicapone would be affected by use of controlled-release levodopa preparations, the experience with such preparations is limited.
Opicapone 50 mg demonstrated clinical efficacy superior to placebo during the double-blind treatment, for the primary efficacy variable used in both pivotal studies, i.e. reduction in OFF-time (Table 2), the proportion of OFF-time responders (i.e. a subject who had a reduction in OFF-time of at least 1 hour from baseline to endpoint) was superior to placebo in Study 2 (Table 3). Except for the proportion of OFF time and ON-time responders in Study 2 all secondary endpoints were exploratory.
The LS mean reduction in absolute OFF-time from baseline to endpoint in the entacapone group was -78.7 minutes. The difference in LS mean change in OFF-time of entacapone to placebo in Study 1 was -30.5 minutes. The difference in LS mean change in OFF-time of opicapone 50 mg to entacapone was -24.8 minutes and non-inferiority of opicapone 50 mg to entacapone was demonstrated (95% confidence interval: -61.4, 11.8).
Most of the gain of ON-time in all treatment groups was ON-time without troublesome dyskinesia. In Study 1, the change from baseline to endpoint in LS mean ON-time without troublesome dyskinesia was 109.1 minutes in the opicapone 50 mg group. The change from baseline for this endpoint in the placebo group was 46.5 minutes. In Study 2, the change from baseline to endpoint in LS mean ON-time without troublesome dyskinesia was 85.6 minutes in the opicapone 50 mg group. The change from baseline for this endpoint in the placebo group was 48.2 minutes.

 The results of the open-label (OL) extension studies of 1 year duration in 862 patients who continued treatment from the double-blind studies (Study 1-OL and Study 2-OL) indicated maintenance of the effect achieved during DB study periods. In the OL studies, all patients began at a dose of 25 mg opicapone for the first week (7 days), regardless of their prior treatment in the double-blind period. If end-of-dose motor fluctuations were not sufficiently controlled and tolerability allowed, the opicapone dose could be increased to 50 mg. If unacceptable dopaminergic adverse events were seen, the levodopa dose was to be adjusted. If not sufficient to manage the adverse events, the opicapone dose could then be down titrated.
The results of the open-label (OL) extension studies of 1 year duration in 862 patients who continued treatment from the double-blind studies (Study 1-OL and Study 2-OL) indicated maintenance of the effect achieved during DB study periods. In the OL studies, all patients began at a dose of 25 mg opicapone for the first week (7 days), regardless of their prior treatment in the double-blind period. If end-of-dose motor fluctuations were not sufficiently controlled and tolerability allowed, the opicapone dose could be increased to 50 mg. If unacceptable dopaminergic adverse events were seen, the levodopa dose was to be adjusted. If not sufficient to manage the adverse events, the opicapone dose could then be down titrated.
For other adverse events, the levodopa and/or opicapone dose could be adjusted.
5.2 Pharmacokinetic Properties
Absorption.
Pharmacokinetic results in healthy volunteers showed that opicapone is rapidly absorbed, with a tmax of 0.5 h to 3.0 h following once-daily multiple-dose administration of 50 mg opicapone under fasted conditions.
When a single-dose of 50 mg of opicapone was administered with a high-fat meal, Cmax, AUC0-t, and AUC0-∞ of opicapone significantly decreased around 68%, 53%, and 51%, respectively, in relation to fasted conditions. When a dose of 50 mg of opicapone under steady-state conditions was administered with a moderate-fat meal, Cmax of opicapone also decreased around 62% in relation to fasted conditions. However, no significant effect was observed on the total plasma exposure (AUC0-24), neither in the COMT inhibition profile.
Distribution.
In vitro studies over the opicapone concentration range 0.3 to 30 microgram/mL showed that binding of 14C-opicapone to human plasma proteins is high (99.9%) and concentration-independent. The binding of 14C-opicapone to plasma proteins was unaffected by the presence of warfarin, diazepam, digoxin and tolbutamide, and the binding of 14C-warfarin, 2-14C-diazepam, 3H-digoxin and 14C-tolbutamide was unaffected by the presence of opicapone and opicapone sulfate, the major human metabolite.
After oral administration, the apparent volume of distribution of opicapone at a dose of 50 mg was 29 L with an inter-subject variability of 36%.
Biotransformation.
Sulfation of opicapone is the primary metabolic pathway in humans, yielding an inactive opicapone sulfate metabolite that accounted for 58.6% of the total circulating radioactivity. Other lesser-abundant metabolic pathways include glucuronidation, methylation (by COMT), reduction and glutathione conjugation.
Elimination.
In healthy subjects, the opicapone elimination half-life was 0.7 h to 2.3 h following once-daily multiple-dose administration up to 50 mg opicapone.
Following once-daily multiple oral doses of opicapone in the dose range of 5 to 50 mg, opicapone sulfate presented a long terminal phase with elimination half-life values ranging from 94 h to 114 h and, as a consequence of this long terminal elimination half-life, opicapone sulfate presented a high accumulation ratio in plasma, with values close of up to 6.6.
After oral administration, the apparent total body clearance of opicapone at a dose of 50 mg was 22 L/h, with an inter-subject variability of 45%.
After administration of a single dose of radiolabeled opicapone 100 mg (2 times the recommended dosage) to healthy subjects, approximately 70% of the dose was recovered in feces (22% as unchanged), 20% in expired air, and 5% in urine (< 1% as unchanged).
Linearity/non-linearity.
Opicapone exposure was shown to increase in a dose proportional manner following once-daily multiple dose administration only up to 50 mg opicapone.
Elderly (≥ 65 years old).
The pharmacokinetics of opicapone was evaluated in elderly subjects (aged 65-78 years old) after 7-day multiple-dose administration of 30 mg. An increase in both the peak and extent of systemic exposure was observed for the elderly population when compared to the young population. The S-COMT activity inhibition was significantly increased in elderly subjects. The magnitude of this effect is not considered to be of clinical relevance.
Weight.
There is no relationship between exposure of opicapone and body weight over the range of 40-100 kg.
Hepatic impairment.
There is limited clinical experience in patients with moderate hepatic impairment (Child-Pugh Class B). The pharmacokinetics of opicapone was evaluated in healthy subjects and moderate chronic hepatic impaired patients after administration of a single dose of 50 mg. The bioavailability of opicapone was significantly higher in patients with moderate chronic hepatic impairment (Cmax = 1038 nanogram/mL vs 548 nanogram/mL in healthy subjects; ASC0-t = 3120 nanogram.h/mL vs. 1668 nanogram.h/mL in healthy subjects).
There is no clinical experience in patients with mild hepatic impairment (Child-Pugh Class A) and in patients with severe hepatic impairment (Child-Pugh Class C) (see Section 4.2 Dose and Method of Administration).
Renal impairment.
The pharmacokinetics of opicapone was not directly evaluated in subjects with chronic renal impairment. However, an evaluation with 50 mg opicapone was performed in subjects included in both phase 3 studies with GFR/1.73 m2 < 60 mL/min (i.e. moderately decreased renal elimination capacity), and using pooled BIA 9-1103 data (major metabolite of opicapone). BIA 9-1103 plasma levels were not affected in patients with chronic renal impairment, and as such, no dose adjustment needs to be considered.
5.3 Preclinical Safety Data
Genotoxicity.
Opicapone was not mutagenic in an in vitro bacterial reverse mutation (Ames) assay, chromosome aberration test in vitro and in vivo rat micronucleus test.
Carcinogenicity.
Two-year oral carcinogenicity studies at doses up to 750 or 1000 mg/kg/day in mice and rats respectively (approximately 4 or 10 times the clinical exposure based on AUC) showed no clear evidence of carcinogenicity.6 Pharmaceutical Particulars
6.1 List of Excipients
Capsule content.
Lactose monohydrate, sodium starch glycollate type A, pregelatinised maize starch, magnesium stearate.
Capsule shell.
Gelatin, indigo carmine aluminium lake, erythrosine, titanium dioxide.
Printing ink.
Shellac, titanium dioxide, propylene glycol, ammonia solution (concentrated), simethicone.
6.2 Incompatibilities
Not applicable.
6.3 Shelf Life
In Australia, information on the shelf life can be found on the public summary of the Australian Register of Therapeutic Goods (ARTG). The expiry date can be found on the packaging.
6.4 Special Precautions for Storage
Store below 30°C.
Store in the original package to protect from moisture.
6.5 Nature and Contents of Container
Opicapone 50 mg hard capsule is packaged in OPA/AL/PVC/Al blisters containing 10, 30 or 90 capsules.
Not all pack sizes may be marketed.
6.6 Special Precautions for Disposal
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
6.7 Physicochemical Properties
Chemical structure.

CAS number.
923287-50-7.7 Medicine Schedule (Poisons Standard)
Schedule 4.
Summary Table of Changes




 The results of the open-label (OL) extension studies of 1 year duration in 862 patients who continued treatment from the double-blind studies (Study 1-OL and Study 2-OL) indicated maintenance of the effect achieved during DB study periods. In the OL studies, all patients began at a dose of 25 mg opicapone for the first week (7 days), regardless of their prior treatment in the double-blind period. If end-of-dose motor fluctuations were not sufficiently controlled and tolerability allowed, the opicapone dose could be increased to 50 mg. If unacceptable dopaminergic adverse events were seen, the levodopa dose was to be adjusted. If not sufficient to manage the adverse events, the opicapone dose could then be down titrated.
The results of the open-label (OL) extension studies of 1 year duration in 862 patients who continued treatment from the double-blind studies (Study 1-OL and Study 2-OL) indicated maintenance of the effect achieved during DB study periods. In the OL studies, all patients began at a dose of 25 mg opicapone for the first week (7 days), regardless of their prior treatment in the double-blind period. If end-of-dose motor fluctuations were not sufficiently controlled and tolerability allowed, the opicapone dose could be increased to 50 mg. If unacceptable dopaminergic adverse events were seen, the levodopa dose was to be adjusted. If not sufficient to manage the adverse events, the opicapone dose could then be down titrated.
