What is in this leaflet
This leaflet answers some common questions about Ospolot. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Ospolot against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Ospolot is used for
Ospolot is used to control epilepsy. Epilepsy is a condition where you have repeated seizures or fits. There are many different types of seizures, ranging from mild to severe.
This medicine belongs to a group of medicines called sulphonamides.
These medicines are thought to work by controlling brain chemicals that send signals to nerves so that seizures do not happen.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
Before you take Ospolot
When you must not take it
Do not take Ospolot if you have an allergy to:
- any medicine containing sulthiame
- any of the ingredients listed at the end of this leaflet
- any other similar medicines such as sulphonamides
Symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Do not drink alcohol while you are being treated with Ospolot.
You should not take this medicine after the expiry date printed on the pack, or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- kidney problems
- depression.
Tell your doctor if you are pregnant or intend to become pregnant or are breastfeeding. Your doctor can discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell them before you start taking Ospolot.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket, health food shop, naturopath or herbalist.
Some medicines and Ospolot may interfere with each other. These include:
- other medicines used to treat fits and convulsions such as primidone and phenytoin
- phenobarbitone, carbamazepine, lamotrigine, a medicine used to sedate people or control convulsions
- medicines used to treat eye conditions or control convulsionssuch as carboanhydrase-inhibitors.
These medicines may be affected by Ospolot or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take Ospolot
Follow all directions given to you by your doctor or pharmacist carefully. It may differ from the information contained in the leaflet.
If you do not understand the instructions on the bottle, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how many tablets you will need to take each day. This may depend on your age, your condition and whether or not you are taking any other medicines.
Your doctor may recommend that you start with a low dose of Ospolot and slowly increase the dose to the lowest amount needed to control your epilepsy.
Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
Follow the instructions they give you. If you take the wrong dose, Ospolot may not work as well and your problem may not improve.
How to take it
Swallow Ospolot with a glass of water.
When to take it
Take Ospolot at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
Take Ospolot immediately after a meal, at about the same time each day. If you take it on an empty stomach, it may cause a stomach upset.
How long to take it
Continue taking Ospolot for as long as your doctor tells you to. Ospolot helps control your condition, but does not cure it. Therefore you must take your medicine every day, even if you feel well.
Most anticonvulsant medicines take time to work, so do not be discouraged if you do not feel better straight away.
Do not stop taking Ospolot or lower the dosage, without checking with your doctor. Do not let yourself run out of medicine over the weekend or on holidays. Stopping this medicine suddenly may cause unwanted effects or make your condition worse. Your doctor will slowly reduce your dose before you can stop taking it completely.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26), or go to the Accident and Emergency Department at your nearest hospital, if you think that you or anyone else may have taken too much Ospolot. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of an overdose may include:
- vomiting
- headache
- dizziness, light-headedness
- spinning sensation
- unsteadiness when walking
- increased rate or abnormal breathing
While you are using Ospolot
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking Ospolot.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
Tell your doctor if you have any changes in mood or behaviour, or have thoughts about harming yourself. This medicine may increase the risk of suicidal thoughts and behaviours.
If you become pregnant while taking Ospolot, tell your doctor immediately.
If you need to have any blood tests tell your doctor that you are taking this medicine. It may affect the results of some tests.
Keep all of your doctor’s appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Tell your doctor if you feel Ospolot is not helping your condition. Your doctor may need to change the dose of your medicine or may need to change your medicine.
Things you must not do
Do not take Ospolot to treat any other complaints unless your doctor tells you to.
Do not give Ospolot to anyone else, even if they have the same condition as you.
Do not stop using taking your medicine or lower the dosage without checking with your doctor. If you stop taking it suddenly, your condition may worsen.
Do not drink alcohol while taking Ospolot.
Things to be careful of
Be careful driving or operating machinery until you know how Ospolot affects you. This medicine may cause dizziness in some people. If you have any of these symptoms do not drive, operate machinery or do anything else that could be dangerous.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Ospolot
This medicine helps most people with epilepsy, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- weakness, unsteadiness when walking, reduced co-ordination or slowed reactions
- rapid breathing, shortness of breath, difficulty breathing
- change in heart beat
- changes in appetite, changes in your weight
- numbness or tingling face, hands and feet
- fainting.
The above list includes the more common side effects of your medicine.
Tell your doctor as soon as possible if you notice any of the following:
- giddiness
- skin rash
- nausea or vomiting
- stomach pain, cramps or discomfort
- headache
- double vision
- increased saliva
- increased pain
- sleeplessness (insomnia)
- unusual changes in mood or behaviour
- symptoms of depression which may include:
- sadness
- loss of interest or pleasure in activities you used to enjoy
- change in weight
- difficulty sleeping, or oversleeping
- energy loss
- feelings of worthlessness
- thoughts of death
The above list includes the less common side effects of your medicine.
Tell your doctor immediately or go to the Accident and Emergency Department at your nearest hospital if you notice any of the following:
- suicidal thoughts, behaviour, or thoughts about self-harm
- severe skin blisters and bleeding in the lips, eyes, mouth, nose and genitals
- fever, severe chills, sore throat or mouth ulcers
- more frequent or more severe seizures or fits
- a series of rapidly repeated seizures without gaining consciousness
- severe depression, recurrence of a previous mental illness.
These are very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people. Some of these side effects such as changes in the levels of calcium and vitamin D can only be found when your doctor does tests from time to time to check your progress.
After using Ospolot
Storage
Keep your tablets in the bottle until it is time to take them. If you take the tablets out of the bottle they will not keep well.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store Ospolot or any other medicine in the bathroom or near a sink. Do not leave it in on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
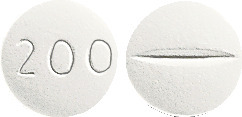
Ospolot 50 mg contains 50 mg tablets that are white, round, film-coated and debossed 50 on one side, plain on the reverse side.
Ospolot 200 mg contains 200 mg tablets that are white, round, film-coated and debossed 200 on one side and scored on the reverse side.
The 50 mg tablets and 200 mg tablets are supplied in HDPE bottles (200 tablets per bottle).
Ingredients
Ospolot 50 mg contains 50 mg of sulthiame as the active ingredient per tablet.
Ospolot 200 mg contains 200 mg of sulthiame as the active ingredient per tablet.
Both strengths also contain:
- maize starch
- lactose monohydrate (sugars)
- purified talc
- colloidal anhydrous silica
- gelatin
- magnesium stearate
- hypromellose
- macrogol 4000
- titanium dioxide
Ospolot does not contain sucrose, gluten, tartrazine or any other azo dyes.
Supplier
Ospolot® is supplied in Australia by:
Phebra Pty Ltd
19 Orion Road
Lane Cove West NSW 2066
Australia
Ospolot® 50 mg
AUST R 18847
Phebra product code TAB002
Ospolot® 200 mg
AUST R 18848
Phebra product code TAB003
This leaflet was updated in Jun 2021.
Ospolot, Phebra and the Phi symbol are registered trademarks of Phebra Pty Ltd.
Published by MIMS August 2021


 The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
