What is in this leaflet
This leaflet answers some common questions about Panadeine EXTRA. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor or pharmacist has weighed the risks of you taking Panadeine EXTRA against the benefits this medicine is expected to have for you.
Keep this leaflet with the medicine.
You may need to read it again.
What is Panadeine EXTRA used for
This medicine is for the short-term treatment of acute strong pain when other pain killers have not worked.
You should only take this product for a maximum of 3 days at a time. If you need to take it for longer than 3 days, you should see your doctor for advice.
This medicine contains codeine which can cause addiction if you take it continuously for more than 3 days.
Panadeine EXTRA provides effective temporary relief from strong pain and discomfort associated with headache, muscle pain, period pain, arthritis, neuralgia, migraine headache, cold & flu, tension headache, back pain and toothache. Panadeine EXTRA also reduces fever associated with these pain conditions.
Panadeine EXTRA contains paracetamol and codeine phosphate.
Paracetamol and codeine phosphate are analgesics. They provide effective temporary relief from pain.
Other uses
Panadeine EXTRA is only registered for the uses listed above. However, your doctor or pharmacist may recommend this medicine for another use.
If you want more information, ask your doctor or pharmacist.
Do not use Panadeine EXTRA if
- You are allergic to paracetamol or codeine or other opioid pain killers or any of the ingredients listed under "Product Description". The symptoms of an allergic reaction may include a rash, asthma attack or hay fever.
- You are under 18 years.
- You are taking any other medicines containing paracetamol or codeine.
- You are pregnant, unless advised by your doctor.
- You are breastfeeding. The use of codeine containing products whilst breastfeeding may harm your baby.
- You have been told by your doctor that you breakdown codeine rapidly since the following side effects may develop: feeling sick, vomiting, constipation, decreased or lack of appetite, feeling tired or sleeping for longer than usual, feeling confused and have breathing problems.
- The expiry date (EXP) printed on the pack has passed.
- The packaging is torn or shows signs of tampering.
Before you start to take it
You must tell your doctor or pharmacist if:
- You have allergies to:
- Any of the ingredients in Panadeine EXTRA.
- You have any of these conditions:
- Liver or kidney problems
- you have a severe infection as this may increase the risk of metabolic acidosis
- signs of metabolic acidiosis include: deep, rapid, difficult breathing, feeling sick (nausea), being sick (vomiting), loss of appetite
- Bowel problems including blockage of your bowel
- You had an operation to remove your gallbladder
- Depression
- Alcoholism
- Respiratory Depression
- You are pregnant or breastfeeding
- You are taking any of these medicines:
- Any medicines causing sleepiness or drowsiness including sleeping tablets, sedatives, tricyclic antidepressants, phenothiazine tranquilizers or alcohol
- Metoclopramide or domperidone: medicines used to stop you feeling sick
- Epilepsy medication
- Medicines called MAOIs (monoamine oxidase inhibitors)
- Medicines used to thin the blood such as warfarin
Panadeine EXTRA may affect the way these medicines work.
How to take Panadeine EXTRA
Tablets, Caplets
Adults aged 18 years and over (including the elderly)
Tablets: 2
How often: Every 4-6 hrs with water as required (maximum 8 tablets in 24 hrs)
If symptoms persist or worsen, please consult your doctor.
This product should be taken at the lowest dose for the shortest time necessary to relieve your symptoms. Taking this medicine regularly for a long time can lead to addiction.
Do not take for more than 3 days without asking your doctor.
Do not exceed the stated dose and do not take more frequently than every 4 hours.
Do not take this product with any other product containing paracetamol or codeine.
You should follow the instructions on the label unless your doctor advises otherwise.
This preparation is for the relief of minor and temporary ailments and should be used strictly as directed. Prolonged use without medical supervision could be harmful.
Do not use in children under 18 years.
If you forget to take it
You may take Panadeine EXTRA as soon as you remember if you think you need it. Do not take a double dose to make up for the one you missed.
Your next dose should be taken in 4 hours if you think you need it.
If you take too much (Overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26 in Australia or 0800 764 766 in New Zealand) for advice or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much Panadeine.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention because of the risk of delayed, serious liver damage if left untreated.
While you are taking Panadeine EXTRA
Things you must do
Take Panadeine EXTRA exactly as your pharmacist or doctor has told you to.
Tell any other doctor, dentist and pharmacist who treat you that you are taking this medicine.
Tell your doctor or pharmacist if you become pregnant while taking Panadeine EXTRA.
Things you must NOT do
Do not use this medicine to treat any other complaint unless your doctor or pharmacist says it is safe. Do not give this medicine to anyone else even if they have the same symptoms as you.
Things to be careful of
Do not drink alcohol.
About 8% of people are poor metabolisers of codeine and Panadeine EXTRA may not work as well if you are one of those people.
Product may cause drowsiness or dizziness. If affected do not drive or operate machinery.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while taking Panadeine EXTRA.
Like other medicines, Panadeine EXTRA can cause some side effects. If they occur, they are most likely minor and temporary. However, sometimes they are serious and need medical treatment.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your pharmacist or doctor if you notice any of the following and they worry you:
- Heartburn
- Nausea
- Vomiting
- Constipation
- Dizziness
- Drowsiness
Panadeine EXTRA may worsen the side effects of alcohol. Avoid alcohol while using Panadeine EXTRA.
Stop taking this medicine and tell your doctor immediately if:
- You have previously had gallbladder removal surgery and experience abdominal pain, nausea and vomiting
- You experience allergic reactions such as skin rash or itching, sometimes with breathing problems or swelling of the lips, tongue, throat or face
- You experience a skin rash or peeling or mouth ulcers
- You have previously experienced breathing problems with aspirin or non-steroidal anti-inflammatories and experience a similar reaction with this product.
- You experience unexplained bruising or bleeding.
These reactions are rare.
After taking Panadeine EXTRA
Storage
Keep your tablets or caplets in the blister pack until it is time to take them.
Keep pack stored in a cool, dry place where the temperature stays below the stated temperature on the pack. Protect from moisture.
Do not store Panadeine EXTRA or any other medicine in the bathroom or moist areas.
Keep Panadeine EXTRA where young children cannot see or reach them.
A locked cupboard at least one and a half metres above the ground is a good place to store medicines.
Do not leave Panadeine EXTRA in the car on hot days.
Disposal
If you stop taking Panadeine EXTRA, ask your pharmacist what to do with any that is left over.
This is not all the information that is available on Panadeine EXTRA. If you have any more questions or are not sure about anything, ask your doctor or pharmacist.
Product Description
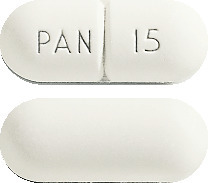
Panadeine EXTRA comes as white, scored, capsule shaped tablet (caplet), marked PAN 15.
A box contains 12, 24, or 40 caplets (when sold in a pharmacy) or 6 caplets (when provided as a health professional sample).
Active Ingredients
Panadeine EXTRA contains 500 mg paracetamol and 15 mg codeine phosphate as active ingredients.
Other ingredients:
- Maize Starch
- Purified Talc
- Pregelatinised Maize Starch
- Povidone
- Stearic Acid
- Potassium Sorbate
- Magnesium stearate
- Panadeine EXTRA contains no sugar, lactose, alcohol or wheat starch.
Manufacturer/Supplier
GlaxoSmithKline Consumer Healthcare Australia Pty Ltd
82 Hughes Avenue, Ermington NSW and Auckland, New Zealand
Tablets: AUST R 101436
Date of preparation: November 2015
PANADEINE and The Panadeine Vibration are trade marks of the GSK group of companies or it licensor.
Helpful Advice on Managing Strong Pain
Strong pain can be debilitating and therefore effect your concentration and ability to carry on with everyday tasks. Below is some helpful advice on additional ways to manage your strong pain.
- Application of gentle heat to the painful area. This increases the blood flow to the affected area, which works to relieve the sensation of pain and aids the healing process. Hot water bottles, hot showers and heat bags can be useful.
- Pain as a result of inflammation can also be treated by the application of cold to the affected area. Cold packs can often be more effective in the early stages of an injury than heat. See your doctor or pharmacist for advice on the best way to treat your pain.
- For some people massage can also help to increase the blood flow to an area and contribute to increasing flexibility of joints and muscles. Massage oils may help.
- Practice relaxation techniques. There are many useful books and courses available to instruct you on simple, effective techniques.