What is in this leaflet
This leaflet answers some common questions about Panadeine Forte tablets. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Panadeine Forte against the benefits this medicine is expected to have for you.
Keep this information with the tablets. You may need to read it again.
What is Panadeine Forte used for
Panadeine Forte is used to relieve moderate to severe pain and fever.
Panadeine Forte contains paracetamol and codeine. Paracetamol and codeine work together to stop the pain messages from getting through to the brain. Paracetamol also acts in the brain to reduce fever.
Your doctor may have prescribed this medicine for another use.
Ask your doctor or pharmacist if you have any questions about why the medicine has been prescribed for you.
This medicine is only available with a doctor's prescription.
Before you take Panadeine Forte
When you must not take it
Do not take Panadeine Forte if you are allergic to paracetamol or codeine or any of the ingredients listed under "Product Description" at the end of this leaflet.
The symptoms of an allergic reaction may include a rash, asthma attack or hay fever.
Do not take this medicine if you have or have had any of the following medical conditions:
- Acute breathing difficulties such as bronchitis, unstable asthma or emphysema
- Glucose-6-phosphate dehydrogenase deficiency (an enzyme deficiency)
- Ultra-rapid metaboliser of CYP 2D6
- Diarrhoea caused by poisoning or antibiotics
- Liver failure
Do not take Panadeine Forte if you have a history of drug dependence, including alcohol dependence.
Do not take Panadeine Forte if you have experienced systemic allergy (generalised rash or shortness of breath) to morphine or oxycodone.
Do not take Panadeine Forte if you have a history of intolerance to paracetamol and/or codeine.
Do not take Panadeine Forte if you are aged below 18 years of age and have had your tonsils or adenoids removed to treat sleep apnoea.
Do not take Panadeine Forte during the third trimester of pregnancy.
Do not take Panadeine Forte during labour especially if the baby is premature. This medicine contains codeine, which may produce withdrawal effects in the newborn baby.
Do not use Panadeine Forte if you are breastfeeding or planning to breastfeed. The medicine passes into breast milk and may affect the baby.
Do not use Panadeine Forte after the expiry date (EXP) printed on the pack.
If you take it after the expiry date it may have no effect at all, or worse, have an entirely unexpected effect.
Do not use Panadeine Forte if the packaging is torn or shows signs of tampering.
Do not use this medicine to treat any other complaint unless your doctor says it is safe.
Panadeine Forte is not recommended for children under 12 years.
Before you start to take it
Tell your doctor or pharmacist if you have allergies to:
- Any other medicines
- Aspirin or any other NSAID medicine
- Any other substances, such as foods, preservatives or dyes
- Any ingredients listed under "Product Description" at the end of this leaflet
Tell your doctor or pharmacist if you have or have had any medical conditions, especially the following:
- Lung, heart, liver or kidney problems
- Difficulty breathing, wheezing, chronic cough, asthma, or other chronic breathing conditions
- A history of drug dependence, including alcohol dependence
- You drink large quantities of alcohol
- Recent cessation of alcohol
- Low glutathione reserves
- Gilbert's syndrome
- Gall bladder problems or your gall bladder has been removed.
- Multiple sclerosis
- Diarrhoea caused by poisoning
- Recent stomach, intestine or urinary tract surgery
- Irritable bowel syndrome or other bowel problems
- Prostate problems
- Under active thyroid gland or problems with your adrenal glands
- Fits or seizures
- Head injury
- Brain tumours
Tell your doctor if you are pregnant or are planning to become pregnant. Your pharmacist or doctor will discuss the benefits and possible risks of taking the medicine during pregnancy.
If you have not told your doctor about any of these things, tell them before you take any Panadeine Forte.
Taking other medicines
You should also tell your doctor about any other medicines that you have bought without a prescription from either your pharmacy, supermarket or health food shop.
Tell your doctor if you are using any other medicines, including any of the following medicines:
- Any medicine causing sleepiness or drowsiness
- Tranquillisers (medicines for anxiety and nerves)
- Benzodiazepines (medicines used as sedatives or to treat anxiety)
- Medicines used to treat alcohol and/or opioid dependence (eg naltrexone or buprenorphine)
- Medicines containing alcohol (ethanol), e.g. some cough syrups
- Cough suppressants or antitussives
- Antihistamines (medicines used to treat allergies)
- Medicines used to treat depression
- Medicines used to treat mental illness
- Medicines which thin the blood
- Medicines to treat epilepsy
- Other pain relief medication
- Medicines used to treat high blood pressure
- Medicines used to relax muscles
- Medicines used to treat diarrhoea, nausea or vomiting
- Propantheline, a drug used to treat stomach ulcers
- Cholestyramine (medicine used to treat bile problems and/or high cholesterol)
- Chelating resin
- Chloramphenicol (antibiotic used to treat ear and eye infections)
- Flucloxacillin, rifampicin or zidovudine (medicines for infection)
These medicines may be affected by Panadeine Forte or may affect how well Panadeine Forte works.
Your doctor or pharmacist can tell you what to do if you are taking any of these medicines.
How to take Panadeine Forte
The label on your pack of Panadeine Forte will tell you how to take your medicine and how often.
If you are unsure about the directions ask your doctor or pharmacist.
Do not take more than the dose your doctor or pharmacist has directed. The dosage recommended by the doctor may be different to the recommended dosage.
The recommended dose of Panadeine Forte is:
Adults: 1 tablet for mild to moderate pain. 2 tablets for severe pain.
This dosage may be repeated in 4-6 hours if necessary.
Do not take more than 8 tablets in 24 hours.
Do not take more than the recommended dose. Taking more than the recommended dose may cause liver damage.
Talk to your doctor about pain control if the medicine is not helping.
If your body cannot metabolise codeine properly, you may be getting reduced benefit from the medicine.
How to take it
Swallow the tablets with water.
The directions given to you by your doctor or pharmacist may be different from the information in this leaflet. If you are unsure what dose to take ask your pharmacist or doctor.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed.
This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your pharmacist or doctor.
If you take too much (Overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else has taken too much Panadeine Forte.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep telephone numbers of these places handy.
If you take too many tablets you may feel nauseous, light headed, dizzy or drowsy.
While you are taking Panadeine Forte
Things you must do
Take Panadeine Forte exactly as your doctor has prescribed.
Tell all your doctors, dentists and pharmacists that you are taking Panadeine Forte.
Tell your doctor if you become pregnant while taking Panadeine Forte.
Things you must not do
Do not take more than the recommended dose unless your doctor tells you to.
Adults should not take more than 8 tablets a day.
Do not take high doses of the medicine for long periods of time unless your doctor tells you to.
Taking more than the recommended dose may cause liver damage.
Codeine may be habit forming.
Do not give this medicine to anyone else.
Things to be careful of
Panadeine Forte may cause dizziness or drowsiness in some people, especially after the first dose.
If affected do not drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or drowsy. Children should not ride bikes if affected and should be supervised to avoid potential harm.
Do not drink alcohol.
Drinking alcohol increases the likelihood of becoming drowsy.
Panadeine Forte may be habit forming if taken in high doses for extended periods of time.
Ask your doctor or pharmacist if you are concerned about this.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while taking Panadeine Forte.
Like other medicines, Panadeine Forte can cause some side effects. If they occur, they are most likely minor and temporary. However, sometimes they are serious and need medical treatment.
If you have any questions, ask your doctor or pharmacist.
Tell your doctor if you notice any of the following and they worry you:
- Constipation
- Nausea
- Vomiting
- Stomach pain
- Dizziness
- Drowsiness
- Skin rashes
- Sweating
These are the more common side effects of Panadeine Forte. They are usually mild.
Tell your doctor as soon as possible if you notice any of the following:
- Shortness of breath
- Mouth ulcers, fever and sore throat
- Bleeding, bruising more easily
- Unusual or extreme mood swings
- Dizziness, light-headedness
- Flushing of the face
- Painful red areas with blisters and peeling layers of skin which may be accompanied by fever and/or chills
- Severe blisters and bleeding in the lips, eyes, mouth, nose and genitals
- Hepatitis (symptoms include loss of appetite, itching, yellowing of the skin and eyes, light coloured bowel motions, dark coloured urine)
The above list includes serious side effects that may require medical attention. These side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- Wheezing or difficulty breathing
- Swelling of the face, lips, tongue or other parts of the body
- Rash, itching or hives on the skin
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
If you are taking Panadeine Forte regularly, you may also need to take laxatives to prevent constipation.
Some people may get other side effects not listed above.
Tell your doctor if you notice anything else that is making you feel unwell.
After taking Panadeine Forte
Storage
Keep your tablets in the blister pack until it is time to take them.
If you take the tablets out of the box or the blister pack they will not keep well.
Keep Panadeine Forte in a cool, dry place where the temperature stays below 25°C.
Heat and dampness can destroy some medicines. Do not leave Panadeine Forte in the car on hot days.
Do not store Panadeine Forte or any other medicine in the bathroom or near a sink.
Keep Panadeine Forte where young children cannot reach it.
A locked cupboard at least one and a half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking the tablets, ask your pharmacist what to do with any tablets that are leftover.
Product Description
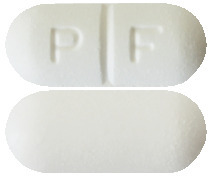
Panadeine Forte comes as a white capsule shaped tablet, marked PF.
It comes in boxes of 20 or 50 tablets.
Each Panadeine Forte tablet contains:
Active Ingredient
- Paracetamol 500 mg
- Codeine phosphate hemihydrate 30 mg
Other ingredients
- Maize starch
- Purified talc
- Magnesium stearate
- Microcrystalline cellulose
- Croscarmellose sodium
- Potassium sorbate
- Pre-gelatinised maize starch
- Stearic acid
- Povidone
Panadeine Forte does not contain gluten, lactose, sucrose, tartrazine or any azo dyes.
Manufacturer
Panadeine Forte is supplied by:
sanofi-aventis australia pty ltd
12-24 Talavera Road
Macquarie Park NSW 2113
AUST R 73507
This leaflet was prepared in June 2017
panadeine-forte-ccsiv1-cmiv10-jun17
Published by MIMS September 2017

 Paracetamol MW 151.17.
Paracetamol MW 151.17. Codeine phosphate hemihydrate MW 406.37.
Codeine phosphate hemihydrate MW 406.37.