What is in this leaflet
This leaflet answers some common questions about PURI-NETHOL. It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking PURI-NETHOL against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What PURI-NETHOL is used for
PURI-NETHOL contains mercaptopurine monohydrate as the active ingredient. It belongs to a group of medicines called cytotoxics.
PURI-NETHOL is used solely or in combination with other medicines to treat acute leukaemia, a cancer of certain blood cells.
It works by interfering with the growth of cancer cells.
Ask your doctor if you have any questions about why PURI-NETHOL has been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor's prescription.
There is no evidence that it is addictive.
Before you take it
When you must not take it
Do not take PURI-NETHOL if you have ever had an allergic reaction to:
- Mercaptopurine monohydrate
- Azathioprine
- any of the tablet ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty in breathing; swelling of the face, lips, tongue or any other parts of the body; rash, itching or hives on the skin.
Do not take PURI-NETHOL if you are planning to become pregnant or father a child unless you and your doctor have discussed the risks and benefits involved. As with all cytotoxic drugs, PURI - NETHOL may harm eggs and sperm. Reliable contraceptive methods must be taken to avoid pregnancy whilst you or your partner is taking this medicine. Contraception is advised for at least 3 months after receiving the last dose of PURI-NETHOL.
Do not take PURI-NETHOL if you are pregnant unless you and your doctor have discussed the risks and benefits involved. It may affect your developing baby if you take it during pregnancy.
Do not take this medicine whilst breast feeding. It is not recommended for use while breast feeding as it is found in breast milk.
Do not take PURI-NETHOL after the expiry date printed on the pack. If you take it after the expiry (EXP) date has passed, it may not work as well.
Do not take it if the packaging is torn or shows signs of tampering.
Before you start to take it
Tell your doctor if you are allergic to any other medicines or any other foods, dyes or preservatives.
Tell your doctor if you have or have had any of the following conditions:
- you have recently received or are receiving radiotherapy or chemotherapy
- you have recently been vaccinated or are planning to be vaccinated
- kidney or liver disease
- a condition where your body produces too little of a natural chemical called thiopurine methyltransferase (TPMT).
If you have not told your doctor about any of the above, tell them before you start taking PURI-NETHOL.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by PURI-NETHOL or may affect how well it works. You may need to take different amounts of your medicine or you may need to take different medicines. These include:
- allopurinol, oxipurinol and/or thiopurinol and other xanthine oxidase inhibitors such as febuxostat.
- Methotrexate
- Infliximab
- anticoagulants e.g. warfarin
- 6-thioguanine
- aminosalicylate derivatives such as olsalazine, mesalazine or sulphasalazine
- vaccinations with 'live' organism vaccines
- myelosuppressive agents
- ribavirin
Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking this medicine.
How to take it
How much to take
Take PURI-NETHOL exactly as directed by your doctor.
Your doctor will decide what dose and for how long you will be taking PURI-NETHOL. This depends on factors such as:
- your age and weight
- any pre-existing conditions such as kidney or liver disease, (especially in the elderly)
- your response to the treatment
- other medicines taken in combination with PURI-NETHOL.
Your doctor may change the dose and frequency of your medicine as your condition changes.
Your doctor may order regular blood cell count, liver function and urinetests while you are taking PURI-NETHOL in order to monitor your condition and to change your dose if necessary.
How to take it
Do not crush or chew the tablets.
Like all cytotoxic drugs, PURI-NETHOL is irritant to the eyes and skin. To prevent irritation it is important to wash your hands immediately after handling or halving the tablets, to avoid contact with the eyes and be careful not to inhale any particle of the tablet.
How long to take it
Your doctor will tell you how long to take PURI-NETHOL for.
Do not stop taking it or change the dose without first checking with your doctor.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 131126) for advice, if you think you or anyone else may have taken too much PURI-NETHOL, even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
Tell your doctor if, for any reason, you have not taken your medicine exactly as directed. Otherwise, your doctor may think that it was not working as it should and change your treatment unnecessarily.
Do not take a double dose to make up for the one you have missed.
Visit your doctor regularly so they can check your progress and make sure your medicine is working.
Tell any other specialist, doctor, dentist or pharmacist that you are on PURI-NETHOL, especially if you are about to be started on any new medicines, immunisations, vaccinations or radiotherapy.
Tell your doctor if you become pregnant, are trying to become pregnant or trying to father a child.
Use a sunscreen with a high SPF and protective clothing and limit exposure to sunlight and UV light.
Things you must not do
Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
Do not use PURI-NETHOL to treat any other complaints unless your doctor says to.
Things to be careful of
Be careful driving or operating machinery until you know how PURI-NETHOL affects you.
Do not have any vaccinations without your doctor's approval.
PURI-NETHOL can lower the number of white blood cells and platelets in your blood. This means that you have an increased chance of getting an infection or bleeding.
Side effects
Tell your doctor as soon as possible if you do not feel well while you are taking PURI-NETHOL.
All medicines can cause some side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
The following side effects have been reported with PURI-NETHOL:
- production of bone marrow cells may be reduced. You may notice an increase in infections. Your doctor will do regular blood tests, but you should tell them at once if you notice any signs of fever or infection or any unexpected bruising, bleeding or signs of blood in your urine
- increased risk of liver disease
- in men, sperm production may be reduced
- as with all cytotoxic medicines, there is an increased risk of damage to the genes in some cells.
Tell your doctor if you notice any of the following:
- nausea and vomiting
- diarrhoea
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bruising or bleeding more easily than normal
- weight loss
- jaundice, a yellowing of the whites of the eyes or the skin
- painful, swollen joints
- skin rash
- hair loss.
Tell your doctor immediately if you notice any of the following allergic-type symptoms:
- wheezing
- swelling of the lips/mouth
- difficulty in breathing
- hayfever
- lumpy rash (hives)
- fainting.
Tell your doctor if you notice anything else that is making you feel unwell, even if you think the problems are not connected with this medicine and are not referred to in this leaflet. Other side effects not listed above may also occur in some people.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking it
Storage
Keep your tablets in the bottle until it is time to take them. If you take the medicine out of the bottle it may not keep as well.
Keep it in a cool, dry place, protected from light, where the temperature stays below 25°C.
Do not leave it in a car, on window sills, near a sink or in the bathroom. Heat and dampness can affect some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Product description
What it looks like
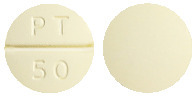
PURI-NETHOL tablets are pale yellow, round, biconvex tablets, marked PT above the line and 50 below the line on one side and plain on the other. Available in bottles of 25 tablets.
Ingredients
Active ingredient:
Each tablet contains 50 mg mercaptopurine monohydrate.
Inactive ingredients:
- lactose monohydrate
- magnesium stearate
- starch-hydrolyzed maize
- starch- maize
- stearic acid.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Phone: +61 2 8436 8300
Web: www.aspenpharma.com.au
Australian Registration Number:
AUST R 10993
This leaflet was revised in February 2021
Published by MIMS May 2021