What is in this leaflet
This leaflet answers some common questions about RBX TOPIRAMATE (topiramate). It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
This leaflet was last updated on the date at the end of this leaflet. More recent information may be available. The latest Consumer Medicine Information is available from https://www.ebs.tga.gov.au/ and may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking RBX TOPIRAMATE against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What RBX Topiramate is used for
The name of your medicine is RBX TOPIRAMATE. RBX TOPIRAMATE contains topiramate.
Topiramate belongs to a group of medicines called antiepileptics. Topiramate prevents seizures and migraines by affecting chemicals in the brain that are involved in sending signals to the nerves.
RBX TOPIRAMATE is used for the treatment of various types of epilepsy in adults and children over 2 years of age.
RBX TOPIRAMATE is also used for the prevention of migraines in adults.
Your doctor may prescribe RBX TOPIRAMATE on its own, or in combination with other medicine for controlling your seizures or migraines. Your doctor may have prescribed RBX TOPIRAMATE for another reason.
Ask your doctor if you have any questions about why RBX TOPIRAMATE has been prescribed for you.
RBX TOPIRAMATE is available only with a doctor’s prescription.
Before you take RBX Topiramate
When you must not take it
- Do not take RBX TOPIRAMATE if you are allergic to topiramate or any of the inactive ingredients listed at the end of this leaflet. Symptoms of an allergic reaction may include: wheezing, swelling of the lips/mouth, difficulty in breathing, hay fever, lumpy rash (hives) or fainting.
- Do not take RBX TOPIRAMATE after the expiry date printed on the pack. If you take it after the expiry date has passed, it may not work as well.
- Do not take RBX TOPIRAMATE if the tablets do not look quite right or if the packaging is torn or shows signs of tampering.
If you are not sure whether you should start taking RBX TOPIRAMATE, talk to your doctor or pharmacist.
Before you start to take it
You must tell your doctor if you:
- have allergies to any medicine, foods, dyes or preservatives.
- are pregnant or intend to become pregnant. Topiramate has caused harm to the developing foetus when administered to a pregnant woman. Its safety has not been verified in pregnant women.
Information available suggests There is an association between the use of topiramate during pregnancy and birth defects including cleft lip/ palate, and neurodevelopmental disorders such as autism spectrum disorders and intellectual disability. However, it is very important to control your fits while you are pregnant. If it is necessary for you to take RBX TOPIRAMATE your doctor will discuss with you whether you should continue to take it during pregnancy. - are breast-feeding or intend to breast-feed. Lactating women should be advised not to breast-feed during treatment with RBX TOPIRAMATE. Your doctor will discuss the possible risks and benefits of taking/using RBX TOPIRAMATE while breast-feeding.
- have or have had mental disorders such as depression or personality disorder.
- have or have had kidney stones, kidney disease or have a family history of kidney stones.
- have or have had liver problems.
- have or have had eye problem or high pressure in the eye.
- have a history of metabolic acidosis (too much acid in the blood, which may cause an increased rate of breathing).
If you have not told your doctor or pharmacist about any of the above, do so before you take RBX TOPIRAMATE.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines you buy without a prescription from your pharmacy, supermarket or health food shop.
In particular, tell your doctor or pharmacist if you are taking:
- other medicines for epilepsy (fits), such as phenytoin, carbamazepine or valproic acid
- digoxin (used to treat heart disease)
- oral contraceptives (the pill)
- metformin, pioglitazone, glibenclamide (used to treat sugar diabetes)
- acetazolamide used to treat glaucoma (increased intraocular pressure)
- lithium, risperidone (used to treat bipolar disorder and schizophrenia)
- haloperidol (used to treat psychoses)
- hydrochlorothiazide (used to treat swelling or high blood pressure)
- diltiazem or propranolol used to treat high blood pressure and or severe chest pain (angina)
- vitamin K-antagonist anticoagulant medications (such as warfarin)
- venlafaxine and amitriptyline (used to treat depression)
- flunarizine (used to treat migraine headache)
- any medicine which slows your reactions. This may include medicines to help you sleep or relieve pain, antidepressants, tranquillisers, alcohol or antihistamines which can make you drowsy
- any medicine which may cause kidney stone
These medicines may be affected by RBX TOPIRAMATE or may affect how well RBX TOPIRAMATE works. Your doctor or pharmacist can tell you what to do if you are taking any of these medicines.
How to take RBX Topiramate
Follow all directions given to you by your doctor or pharmacist carefully. This may differ from the information contained in this leaflet.
How to take it
You can take RBX TOPIRAMATE with or without food. Always swallow the tablets whole with plenty of water.
When to take it
At the start of treatment RBX TOPIRAMATE may be taken once a day, preferably at night. After the dose is increased, it is taken twice a day.
You should continue taking RBX TOPIRAMATE until your doctor tells you to stop. Before stopping, it is recommended that the dose be reduced gradually.
How much and how long to take
The doses shown below are the usual recommended doses. However, your doctor may tell you to take higher or lower doses. Your doctor will start with a low dose and slowly increase the dose to the most suitable dose needed to control your epilepsy. Continue taking RBX TOPIRAMATE for as long as your doctor tells you to. Do not stop taking RBX TOPIRAMATE, or lower the dosage, without checking with your doctor.
Epilepsy
If you are taking only RBX TOPIRAMATE to treat your epilepsy:
For adults, treatment starts at a low dose of 25 mg/day as a single dose (nightly) for one week or longer. The dosage is then increased by 25 to 50 mg/day at weekly or longer intervals to the recommended target dose of 100 mg/day.
For children 2 years and over, treatment starts at a low dose of 0.5 to 1 mg/kg as a single dose (nightly) for the first week. The dosage is then increased by 0.5 to 1 mg/kg daily at weekly or longer intervals to the recommended target dose of 3 to 6 mg/kg/day.
If you are taking RBX TOPIRAMATE with other antiepileptic drugs:
For adults, treatment starts at a low dose of 25 to 50 mg as a single dose (nightly) or divided dose for one week or longer. The dosage is then increased by 25 to 100 mg/day at weekly or longer intervals to the recommended target dose of 200 to 400 mg/day.
For children 2 years and over, treatment starts at 1 to 3 mg/kg/day up to 25 mg/day as a single dose (nightly) for the first week. The dosage is then increased by 1 to 3 mg/kg/day at weekly or longer intervals to the recommended target dose of 5 to 9 mg/kg/day.
Migraine
Treatment starts at a low dose of 25 mg as a single dose (nightly) for one week. The dose is then increased over weekly periods or longer by 25 mg/day, until the most suitable dose is reached (only for adults).
If you forget to take it
- Take your dose as soon as you remember, and then go back to taking your medicine as you would normally.
- If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
- Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some hints.
If you have taken too much (overdose)
If you have taken too much, immediately telephone your doctor or the Poisons Information Centre (Tel. No. 131126) for advice, or go to Accident & Emergency at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep these numbers handy in case of an emergency.
If you take too much RBX TOPIRAMATE, you may experience headache, lightheadedness, agitation, drowsiness, lethargy, convulsions, speech disturbances, double or blurred vision, difficulty with thinking, abnormal coordination, reduced responsiveness and awareness, hypotension, abdominal pain, dizziness and depression, muscular weakness, muscle cramps and change in heart rhythm (apart from that you may also experience other symptoms due to low levels of potassium in blood.
While you are using RBX Topiramate
Things you must do
- Drink plenty of water while taking RBX TOPIRAMATE. RBX TOPIRAMATE has been known to cause kidney stones and drinking water may help to prevent this.
- Always follow your doctor's instructions carefully.
- If you are about to start taking a new medicine, tell your doctor or pharmacist that you are taking RBX TOPIRAMATE.
- Tell your doctor if you become pregnant while taking RBX TOPIRAMATE.
Things you must not do
- Do not suddenly stop taking RBX TOPIRAMATE without checking with your doctor.
- Do not drink alcohol.
- Do not drive or operate machinery until you know how the medicine affects you.
- Do not use RBX TOPIRAMATE to treat any other complaint unless your doctor says so.
- Do not give this medicine to anyone else to use.
Things to be careful of
Changes to your medication
If you are seizure free or your seizures are well controlled, a reduction in your dose, discontinuation or substitution of your current medication should first be assessed by your doctor and pharmacist, and any changes should be implemented gradually.
Effects on thoughts and behaviour
Medicines used to treat epilepsy can increase the risk of suicidal thoughts and behaviour. If you experience feelings of deep sadness and unworthiness (depression) or a worsening of these feelings, any unusual changes in your mood, or the emergence of suicidal thoughts, behaviour or thoughts of self harm, you should report this to your doctor immediately.
Decreased sweating and elevation in body temperature
RBX Topiramate may cause decreased sweating and increased body temperature (fever). People, especially children, should be watched for signs of decreased sweating and fever, especially in hot temperatures. Some people may need to be hospitalized for this condition. Call your healthcare provider right away if you have a high fever, a fever that does not go away, or decreased sweating.
Effects on driving and operating machinery
RBX TOPIRAMATE may cause drowsiness, dizziness or other symptoms which could affect your ability to drive or operate machinery. It may also cause visual disturbances and/or blurred vision. Make sure you know how you are affected by this medicine before you drive or use machinery. Particular care is recommended when you first start taking RBX TOPIRAMATE or if the amount of RBX TOPIRAMATE or any other medicine you are taking is increased or decreased.
Effects of food and alcohol
RBX TOPIRAMATE can be taken with or without food. Do not drink alcohol while taking RBX TOPIRAMATE. Alcohol may increase the risk of unwanted side effects, such as drowsiness.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking RBX TOPIRAMATE. RBX TOPIRAMATE helps most people with epilepsy/migraine, but it may have unwanted side effects in a few people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects. Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- dizziness
- decrease in appetite or weight loss
- itchy skin or skin rash
- sleeplessness
- tingling and numbness in fingers and toes
- nausea (feeling sick), loose stool (diarrhoea), vomiting or constipation
- abdominal pain or discomfort
- ear pain, buzzing or ringing in ears, deafness
Tell your doctor as soon as possible if you notice any of the following as you may need medical attention:
- depression
- nervousness or anxiety
- mood alterations such as aggression, agitation or anger
- difficulty with memory and slowing of thought processes
- abnormal behaviour
- speech or language problems
- difficulty with concentration or attention
- fever
- decreased or lack of sweating or overheating (mainly in children)
- reduced sense of touch or sensation
- reduced co-ordination
- balance disorder
- unusual hair loss or thinning
- abnormal frequent urination
- unusual weakness
- taste disturbance or loss of taste
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if you notice any of the following
- unusual tiredness, drowsiness, irritability or lack of energy
- difficulty breathing, fast or irregular heartbeat or tightening of chest
- thoughts of harming yourself or thoughts of suicide
- sudden signs of allergy such as rash, itching or hives, swelling of the face, lips, tongue or other parts of the body, shortness of breath, wheezing or difficulty breathing
- kidney stones
- sudden severe back or side pain, difficult or painful to pass urine
- blood in your urine or severe pain in the lower back or genital area
- sudden changes in your eyesight (eg. blurred, double vision or loss of vision) or uncontrollable eye movements
- eye pain or increased pressure in the eye
- unexplained bleeding or bleeding more frequently
- severe blisters and bleeding in mucosal sites (such as lips, eyes, mouth, nose, genitals)
These are serious side effects. You may need urgent medical attention. Serious side effects are rare.
Other side effects not listed above may also occur in some people. Tell your doctor if you notice any other effects.
After using RBX Topiramate
Storage
Keep RBX TOPIRAMATE in the original pack until it is time to take it.
Keep RBX TOPIRAMATE in a cool, dry place where the temperature is below 25 degrees C. Protect from light.
Do not store RBX TOPIRAMATE or any medicine in the bathroom or near a sink. Do not leave medicines in the car or on window sills. Heat and dampness can destroy some medicines.
Keep RBX TOPIRAMATE where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking RBX TOPIRAMATE, or your medicine has passed its expiry date, ask your pharmacist what to do with any tablets which may be left over.
Product Description
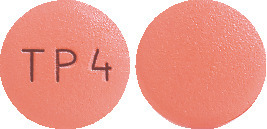
What it looks like
RBX TOPIRAMATE 25 mg tablets are white, film-coated, circular tablets debossed with ‘TP1’ on one side and plain on the other side. Available in packs of 60 tablets.
RBX TOPIRAMATE 50 mg tablets are yellow, film-coated, circular tablets debossed with ‘TP2’ on one side and plain on the other side. Available in packs of 60 tablets.
RBX TOPIRAMATE 100 mg tablets are yellow, film-coated, circular tablets debossed with ‘TP3’ on one side and plain on the other side. Available in packs of 60 tablets.
RBX TOPIRAMATE 200 mg tablets are peach-coloured, film-coated, circular tablets debossed with ‘TP4’ on one side and plain on the other side. Available in packs of 60 tablets.
Ingredients
Active ingredient:
RBX TOPIRAMATE 25 mg tablets - 25 mg of topiramate
RBX TOPIRAMATE 50 mg tablets - 50 mg of topiramate
RBX TOPIRAMATE 100 mg tablets - 100 mg of topiramate
RBX TOPIRAMATE 200 mg tablets - 200 mg of topiramate
Inactive ingredients:
Microcrystalline cellulose, lactose monohydrate, pregelatinised maize starch, sodium starch glycolate (Type A), and magnesium stearate. In addition the 25 mg tablet contains Opadry 12 B 58956 (White), the 50 mg and 100 mg tablets contain Opadry 12 B 52749 (Yellow), and the 200 mg tablet contains Opadry 12 B 56662 (Brown). Opadry 12 B 58956 (White) contains hypromellose 5 cp, titanium dioxide, macrogol PEG 400 and polysorbate 80. Opadry 12 B 52749 (Yellow) contains hypromellose 5 cp, titanium dioxide, macrogol PEG 400, polysorbate 80 and iron oxide yellow. Opadry 12 B 56662 (Brown) contains hypromellose 5 cp, titanium dioxide, macrogol PEG 400, polysorbate 80 and iron oxide red.
Sponsor
RBX TOPIRAMATE is supplied in Australia by:
Sun Pharma ANZ Pty Ltd
12 Waterloo Road
MACQUARIE PARK NSW 2113
Australia
Tel: 1800 726 229
[email protected]
Australian Registration Numbers
RBX TOPIRAMATE 25 mg tablets: AUST R 157964
RBX TOPIRAMATE 50 mg tablets: AUST R 157971
RBX TOPIRAMATE 100 mg tablets: AUST R 157966
RBX TOPIRAMATE 200 mg tablets: AUST R 157973
This leaflet was prepared in May 2024.
Published by MIMS July 2024




 It is not necessary to monitor topiramate plasma concentrations to optimize topiramate therapy. For patients receiving concomitant phenytoin and carbamazepine, dosage adjustment for topiramate may be required (see Section 4.5 Interactions with Other Medicines and Other Forms of Interactions).
It is not necessary to monitor topiramate plasma concentrations to optimize topiramate therapy. For patients receiving concomitant phenytoin and carbamazepine, dosage adjustment for topiramate may be required (see Section 4.5 Interactions with Other Medicines and Other Forms of Interactions). The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. No data are available on the use of topiramate with vigabatrin.
No data are available on the use of topiramate with vigabatrin.





 ADRs reported, rate unspecified, in open-label clinical trials of topiramate-treated paediatric patients are shown in Table 11.
ADRs reported, rate unspecified, in open-label clinical trials of topiramate-treated paediatric patients are shown in Table 11.
 No adverse events were reported during the bioequivalence study comparing RBX Topiramate 25 mg tablets and Topamax 25 mg tablets (Janssen-Cilag Pty Ltd) in healthy, adult, human, male, subjects, under fasting conditions.
No adverse events were reported during the bioequivalence study comparing RBX Topiramate 25 mg tablets and Topamax 25 mg tablets (Janssen-Cilag Pty Ltd) in healthy, adult, human, male, subjects, under fasting conditions. The overall safety profile of topiramate observed in the migraine studies was generally consistent with that established for epilepsy therapy.
The overall safety profile of topiramate observed in the migraine studies was generally consistent with that established for epilepsy therapy.
 Molecular formula: C12H21NO8S.
Molecular formula: C12H21NO8S.