What is in this leaflet
This leaflet answers some common questions about REVOLADE.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available.
You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on the medicine. You can also download the most up to date leaflet from www.novartis.com.au. Those updates may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking REVOLADE against the benefits they expect it will have for you.
If you have any concerns about taking this medicine or giving it to your child, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What REVOLADE is used for
REVOLADE is a medicine that is used to treat a number of conditions.
Low platelet count
This is a bleeding disorder known as idiopathic thrombocytopenic purpura (ITP). Patients with ITP may suffer from an increased risk of bleeding. The symptoms of ITP may include:
- Pinpoint sized flat round red spots under the skin (petechiae)
- Bruising (purpura)
- Nosebleeds
- Bleeding gums
- Not being able to control bleeding, if cuts or injuries occur.
REVOLADE helps to increase the number of platelets, a type of blood cell that helps to reduce or prevent bleeding.
Hepatitis C virus (HCV)
Many patients with HCV have low platelet counts (thrombocytopenia), not only as a result of the disease but also due to some of the medicines that are used to treat the disease.
The use of REVOLADE to increase and maintain the platelet count prior to and throughout antiviral treatment of HCV infection gives patients a better opportunity to maintain the optimal the dose and duration of their antiviral therapy.
Severe aplastic anaemia (SAA)
Severe aplastic anaemia, or SAA, is a blood disorder in which the bone marrow does not make enough blood cells, especially red and white blood cells and platelets. Red blood cells carry oxygen to tissues in the body. White blood cells fight infection and disease. Platelets help blood to clot.
The low number of blood cells puts a patient with this condition at risk of tiredness, infections, and bleeding. REVOLADE may be used to treat patients with these low blood counts:
- In combination with immunosuppressive therapy in adults or children from 2 years of age or
- In adult patients when other medicines to treat SAA have not worked well enough.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is available only with a doctor's prescription.
It is not addictive.
REVOLADE may be used to treat children from 1 to 17 years with chronic immune thrombocytopaenia (ITP) who have failed other treatments and need an increased platelet concentration for a planned procedure or are at a high risk of bleeding.
REVOLADE may be used to treat children from 2 to 17 years with low blood counts caused by severe aplastic anaemia.
REVOLADE it is not recommended to treat children with hepatitis C virus (HCV) infections (to treat low platelet counts).
Before you take REVOLADE
Do not take REVOLADE if you are allergic (hypersensitive) to:
- eltrombopag olamine, the active ingredient in REVOLADE
- any other ingredients in REVOLADE tablets listed at the end of this leaflet
Some of the symptoms of an allergic reaction may include:
- Shortness of breath, wheezing or difficulty breathing;
- Swelling of the face, lips, tongue or other parts of the body;
- Rash, itching or hives on the skin.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering.
If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have any of the following medical conditions:
- Liver problems - your doctor will request blood tests to check your liver function before and during treatment with REVOLADE. You may need a lower dose of REVOLADE
- Kidney problems
- Risk factors for thrombosis (formation of a clot inside a blood vessel, obstructing the flow of blood), or you know that thrombosis occurs frequently in your family
- A history of blood cancers
- Another blood condition, such as myelodysplastic syndrome (MDS). Your doctor will carry out tests to check that you do not have this blood condition before you start REVOLADE. If you have MDS and take REVOLADE your MDS may get worse.
- Had or developed sensitivity to the sun
- A history of cataracts (problems with sight)
- Are pregnant or plan to become pregnant (see PREGNANCY AND BREAST FEEDING)
- Are breast feeding (see PREGNANCY AND BREAST FEEDING).
Taking other medicines
Tell your doctor or pharmacist if you:
- Are taking any other medicines
- Have taken any medicines recently, or
- Start taking new medicines.
This includes herbal medicines and other medicines or complementary therapies you've bought without a prescription.
There are certain medicines, including some prescription, non-prescription medicines, and vitamins, that interact with REVOLADE.
You should not take these at the same time as REVOLADE or they may require dose adjustment while taking REVOLADE.
These medications include some products within the following groups:
- Antacid medicines to treat stomach ulcers or heartburn
- Certain medicines used to lower cholesterol (statins)
- Certain drugs used to treat human immunodeficiency virus (HIV) (lopinavir / ritonavir)
- A medicine used for transplantations or immune diseases (cyclosporin)
- Minerals such as aluminium, calcium, iron, magnesium, selenium and zinc which may be found in mineral supplements and complementary medicines
- Certain medicines used to treat low platelet count due to hepatitis C (interferon-based treatments).
Your doctor will review the medicines you are currently taking to make sure you are not taking something that cannot be taken with the REVOLADE.
If you require any of these medications and a suitable substitute is not available, please discuss this with your doctor.
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
Taking REVOLADE with food and drink
Do not take REVOLADE with food or products rich in calcium.
REVOLADE is affected by calcium intake. REVOLADE may be taken with food low in calcium such as:
- Pineapple, raisins and strawberries
- Lean ham, chicken or beef
- Unfortified fruit juice, soy milk and grain. (Unfortified means not containing any added calcium, magnesium or iron.)
Please discuss this matter with your doctor, pharmacist or healthcare provider. They will be able to advise on the most suitable meals to be eaten while you are taking REVOLADE.
Don't take REVOLADE during the 2 hours before or 4 hours after you take:
- Antacid medication to treat indigestion
- Mineral supplements, such as aluminium, calcium, iron, magnesium, selenium or zinc, or
- Dairy products.
If you do, the medicine will not be properly absorbed into your body.
One way to avoid issues with these products would be to take them in the morning and REVOLADE in the evening.
Ask your doctor or pharmacist for advice if you are unsure.
Pregnancy and breast feeding
You should avoid becoming pregnant while taking REVOLADE can harm an unborn baby.
If you are pregnant, think you may be pregnant or are planning to have a baby speak to your doctor.
You must use a reliable method of contraception (a way to prevent you from becoming pregnant) during treatment with REVOLADE and for at least 7 days after you stop taking REVOLADE.
Ask your doctor about options of effective birth control.
If you do become pregnant while you are taking REVOLADE, tell your doctor immediately.
Breast feeding is not recommended while you are taking REVOLADE. It is not known whether REVOLADE passes into breast milk.
Ask your doctor or pharmacist for advice before taking any medicine if you are unsure.
How to take REVOLADE
Follow all directions given to you by your doctor or pharmacist. The directions may differ from the information contained in this leaflet.
If you do not understand the instructions on the label ask your doctor or pharmacist for help.
When to take it
Take REVOLADE at least 2 hours before or at least 4 hours after antacids, dairy products or some mineral supplements such as iron, calcium, magnesium, aluminium, selenium and zinc.
One way to avoid issues with these products would be to take them in the morning and REVOLADE in the evening.
Taking REVOLADE at the same time each day will help you remember when to take it.
How much to take
Immune thrombocytopenia in adults and children 6-17 years old
- The usual starting dose for adult and paediatric ITP patients 6 to 17 years of age is one 50 mg REVOLADE tablet a day.
- Patients of East-/Southeast-Asian origin need to start at a lower dose of 25 mg per day.
Immune thrombocytopenia in children 1 to 5 years old:
- The usual starting dose for paediatric ITP patients 1 to 5 years of age is one 25 mg REVOLADE tablet a day.
- Paediatric ITP patients 1 to 5 years of age of East-/Southeast-Asian origin need to start at a dose of one 25 mg REVOLADE tablet once daily.
Adult HCV patients
- The usual starting dose for adult HCV patients is one 25 mg REVOLADE tablet a day.
- Patients of East-/Southeast-Asian origin will start on the same 25 mg dose.
Adult patients with previously treated SAA
- The usual starting dose of REVOLADE for patients with previously treated SAA that reoccurred is one 50 mg REVOLADE tablet a day.
- Patients of East/Southeast-Asian origin need to start at a lower dose of 25 mg.
First-line treatment of SAA in combination with standard immunosuppressive therapy
The usual starting dose of REVOLADE for SAA patients when it is given with standard immunosuppressive therapy as the first treatment for severe SAA is:
- Adult and adolescent patients 12 to 17 years of age: 150 mg once a day for 6 months. Patients of East/Southeast-Asian origin should receive a reduced dose of 75 mg once a day for 6 months.
- Paediatric patients 6 to 11 years of age: 75 mg once a day for 6 months. Patients of East/ Southeast-Asian origin should receive a reduced dose of 37.5 mg once a day for 6 months.
- Paediatric patients 2 to 5 years of age: 2.5 mg/kg once a day for 6 months. Patients of East/South-East Asian origin should receive a reduced dose of 1.25 mg/kg once a day for 6 months.
Your doctor will prescribe the appropriate immunosuppressive therapy in addition to REVOLADE.
Based on your response to REVOLADE or if you have kidney, liver or other problems or if you are elderly, your doctor may adapt the dose and may recommend that your daily dose of REVOLADE be increased or decreased.
You should not take more REVOLADE. than your doctor prescribed.
How to take it
TABLETS
Swallow REVOLADE tablets with a glass of water.
How long to take it
Keep taking this medicine for as long as your doctor tells you. After you have stopped taking REVOLADE, your bleeding symptoms may come back.
Tell your doctor or pharmacist if you have any bleeding in the four (4) weeks after you stop taking REVOLADE.
If you forget to take REVOLADE
Do not take a double dose to make up for a missed dose. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take more REVOLADE than you should (Overdose)
Immediately telephone your doctor or the Poisons Information Centre (on 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much REVOLADE.
Do this even if there are no signs of discomfort or poisoning.
Take the REVOLADE pack with you.
Medical treatment may be necessary.
While you are taking REVOLADE
Things you must do
Keep all of your doctor's appointments so that your progress can be checked.
Your doctor will do tests from time to time to make sure the medicine is working and to prevent unwanted side effects. Your doctor will also carry out blood tests to check your liver function before and during treatment with REVOLADE.
At the beginning of therapy, your platelet count and other routine blood parameters will need to be monitored frequently. Based on your response to REVOLADE, your doctor will adapt the dose and may recommend that your daily dose be increased or decreased.
If you become pregnant while taking this medicine, tell your doctor immediately.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking REVOLADE.
Tell any doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
Things to be careful of
- Be careful driving or operating machinery until you know how REVOLADE affects you.
- Liver problems
REVOLADE may damage your liver and cause serious, even life threatening, illness.
You must have blood tests to check your liver before you start taking REVOLADE and during treatment.
When you are given certain antiviral treatments together with REVOLADE for the treatment of thrombocytopenia due to hepatitis C virus (HCV) infections some liver problems can get worse.
Your doctor will order these blood tests and any other tests required. In some cases REVOLADE treatment may need to be stopped.
- Bleeding after you stop treatment
When you stop taking REVOLADE, your blood platelet count will drop back down to what it was before you started taking REVOLADE.
These effects are most likely to happen within 4 weeks after you stop taking REVOLADE.
The lower platelet counts may increase your risk of bleeding.
Your doctor will check your platelet counts for at least 4 weeks after you stop taking REVOLADE.
Tell your doctor or pharmacist if you have any bruising or bleeding in the 4 weeks after you stop taking REVOLADE.
- Problems with bone marrow
Patients taking this medication may have problems with their bone marrow. REVOLADE could make this problem worse.
Signs of bone marrow changes may show up as abnormal results in your blood tests. Your doctor may also carry out tests to check your bone marrow during treatment with REVOLADE.
- Higher chance for blood clots with higher platelet counts
You have a higher chance of getting a blood clot if your platelet count is too high during treatment with REVOLADE, but blood clots can occur with normal or even low platelet counts.
If you have cirrhosis of the liver, you are at risk of a blood clot in a blood vessel that feeds your liver (portal vein thrombosis). You may have severe complications from some forms of blood clots, such as clots that travel to the lungs or that cause heart attacks or strokes.
Your doctor will check your blood platelet counts, and change your dose or stop REVOLADE if your platelet counts get too high.
Tell your doctor right away if you have signs and symptoms of a blood clot in the leg, such as swelling or pain/tenderness of one leg.
- Phototoxicity
REVOLADE may cause you to sunburn more easily.
As a safety precaution, while taking REVOLADE, you should avoid exposure to high-intensity artificial UV light such as tanning beds and being unprotected when in direct sunlight. If you do need to be in the sun, use protective clothing, sun glasses and sunscreen.
- Cataracts
Your doctor may recommend that you are checked for cataracts as part of any routine eye examination.
Things you must not do
Do not give this medicine to anyone else, even if their condition seems to be the same as yours.
Do not stop taking REVOLADE before talking to your doctor or pharmacist. After you have stopped taking REVOLADE, your bleeding symptoms may come back.
Possible side effects
Like all medicines, REVOLADE can cause side effects, although not everybody gets them.
Do not be alarmed by these lists of possible side effects. You may not experience any of them.
SERIOUS SIDE EFFECTS (All indications)
STOP taking REVOLADE and seek medical help immediately if you experience the following:
Serious side effects
- Blood clots (thromboembolic events)
- Loss of function of the liver due to side effects of this treatment (drug induced liver injury)
- Loss of functions of the liver
- Damage occurring in the smallest blood vessels inside the kidney leading to loss of kidney function (thrombotic microangiopathy with acute renal failure).
ADULT PATIENTS WITH ITP
The following side effects have been associated with REVOLADE treatment in adult patients with ITP.
Very common side effects
These may affect more than 1 in 10 people treated with REVOLADE:
- Diarrhoea
- Nausea
Very common side effect that may show up in blood tests:
- Increase in a liver enzyme (called ALT).
Common side effects
These may affect up to 1 in 10 people treated with REVOLADE:
- Dry mouth
- Vomiting
- Unusual hair loss or thinning
- Rash
- Back pain
- Pain that affects muscles and tendons along with bones, including in your chest
- Muscle pain
- Sore throat or discomfort when swallowing
- Urinary tract infections
- Cataract
Common side effects that may show up in blood tests
- Increase in other liver enzymes
- Increased level of the pigment (bilirubin) in the blood, which may cause a yellow discolouration of your skin, the whites of your eyes, or body fluids (jaundice).
PAEDIATRIC PATIENTS (aged 1 to 17 years) with ITP
The following additional side effects have been reported to be associated with treatment with REVOLADE in paediatric patients (aged 1 to 17 years) with ITP.
Very common side effects
- Sore throat, runny nose, nasal congestion and sneezing
- Infection in the nose, sinuses, throat and upper airways, common cold (upper respiratory tract)
- Cough
- Abdominal pain
- Fever.
Common side effects
- Toothache
- Pain in the nose and throat
- Itchy, runny or blocked nose.
Other side effects
Other side effects have occurred during further studies with REVOLADE
Rare side effects (these may affect up to 1 in 1,000 people):
- Clots in small blood vessels, which may harm organs such as the kidneys (Microangiopathy associated with renal impairment).
PATIENTS WITH HCV
The following side effects have been reported to be associated with treatment with REVOLADE in combination with pegylated interferon and ribavirin in patients with HCV.
Very common side effects
- Fever
- Feeling very tired (fatigue)
- Chills
- Headache
- Cough
- Nausea
- Diarrhoea
- Unusual hair loss or thinning of the hair
- Muscle pain
- Itching
- Feeling tired, weak
- Difficulty sleeping
- Loss of appetite
- Flu-like symptoms
- Generalised swelling.
Very common side effects that may show up in blood tests:
- Reduced number of red blood cells (anaemia)
- Increase in bilirubin (a substance produced by the liver).
Common side effects
- Liver failure (serious disturbance of liver function)
- Loss of functions of the liver
- Blood clots
- Rash
- Cataract.
Tell your doctor immediately if you get any of these symptoms. These symptoms may persist after you stop taking REVOLADE.
Tell your doctor right away if you have any of these signs and symptoms of liver problems:
- Jaundice (yellowing of the skin or the whites of the eyes)
- Unusual darkening of the urine
- Unusual tiredness
- Right upper stomach area pain.
PATIENTS WITH SEVERE APLASTIC ANAEMIA (where other medicines have not worked well)
The following side effects have been reported to be associated with REVOLADE treatment in patients with severe aplastic anaemia (SAA).
Very common side effects
- Cough
- Headache
- Shortness of breath
- Pain in the mouth and throat
- Runny nose
- Diarrhoea
- Nausea
- Bruising
- Joint pain
- Muscle spasms
- Pain in arms, legs, hands or feet (pain in extremities)
- Dizziness
- Feeling very tired (fatigue)
- Abdominal pain
- Fever
- Fever with very low number of neutrophils in the blood (white blood cells that are needed to fight infections) (febrile neutropenia).
Very common side effects that may show up in blood tests:
- Increase in some liver enzymes.
Common side effects
- Rash
- Runny nose
- Muscle spasms
- Cataract.
Common side effects that may show up in blood tests
- Increase in bilirubin (a substance produced by the liver).
Other side effects
- Yellowing or darkening of skin (skin discolouration).
PATIENTS WITH SEVERE APLASTIC ANAEMIA (given with standard immunosuppressive therapy)
The following side effects have been reported to be associated with REVOLADE treatment in patients with SAA when it is given with standard immunosuppressive therapy.
Common side effects
- More intense colour of the skin (hyperpigmentation)
Very common side effects
- Yellowing of the skin or whites of the eyes (due to jaundice or increased level of the pigment bilirubin in the blood)
If you experience any of the side effects listed in this leaflet, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
After taking REVOLADE
Storage
- Keep this medicine where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines. - Store the tablets in a cool, dark, dry place below 30°C.
- Do not store REVOLADE or any other medicine in the car, in the bathroom, near a sink, or on a window sill.
Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Medicines should not be disposed of via wastewater or household waste.
Product descriptions
What REVOLADE looks like
Tablets
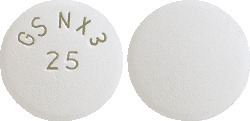
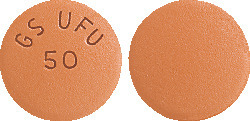
REVOLADE is supplied in packs of 28 tablets. REVOLADE tablets are round, biconvex, film coated tablets, and available in different strengths.
- 12.5 mg*
White, imprinted with 'GS MZ1' and '12.5' on one side. The reverse face is plain. They contain 16 mg of eltrombopag olamine, equivalent to 12.5 mg of eltrombopag. - 25 mg
White, imprinted with 'GS NX3' and '25' on one side. The reverse face is plain. They contain 32 mg of eltrombopag olamine, equivalent to 25 mg of eltrombopag. - 50 mg
Brown, imprinted with 'GS UFU' and '50' on one side. The reverse face is plain. They contain 64 mg of eltrombopag olamine, equivalent to 50 mg of eltrombopag. - 75 mg*
Round, biconvex, pink, and film-coated, debossed with ‘GS FSS’ and ‘75’ on one side. They contain 96 mg of eltrombopag olamine, equivalent to 75 mg of eltrombopag.
Ingredients
REVOLADE tablets contain the active ingredient eltrombopag olamine.
REVOLADE tablets contain the excipients:
- Hypromellose (E464)
- Macrogol 400 (E1521)
- Magnesium stearate (E572)
- Mannitol (E421)
- Microcrystalline cellulose (E460(i))
- Povidone (E1201)
- Sodium starch glycollate
- Titanium dioxide (E171).
- Polysorbate 80 (E433) (12.5 mg tablet and 25 mg tablet only)
- Iron oxide red CI77491 (E172) (50 mg tablet only)
- Iron oxide yellow CI77492 (E172) (50 mg tablet only).
REVOLADE tablets do not contain lactose, sucrose, tartrazine or any other azo dyes.
Supplier
REVOLADE is supplied in Australia by:
Novartis Pharmaceuticals Australia Pty Limited
ABN 18 004 244 160
54 Waterloo Road, Macquarie Park
NSW 2113 AUSTRALIA.
Telephone 1 800 671 203
www.novartis.com.au
® = Registered Trademark
© Copyright 2022
Australian Registration Numbers:
*12.5 mg tablets AUST R 236115
25 mg tablets AUST R 158419
50 mg tablets AUST R 158356
*75 mg tablets AUST R 200121
*Not all strengths and pack sizes may be distributed in Australia.
This leaflet was prepared in July 2022.
Internal document code
(rev270722c based on PI rev270722i)
Published by MIMS September 2022








 In 3 controlled and 2 uncontrolled clinical studies, among adult chronic ITP patients receiving Revolade (n = 446), 17 subjects experienced a total of 19 TEEs, which included (in descending order of occurrence) deep vein thrombosis (n = 6), pulmonary embolism (n = 6), acute myocardial infarction (n = 2), cerebral infarction (n = 2), embolism (n = 1) (see Section 4.4 Special Warnings and Precautions for Use).
In 3 controlled and 2 uncontrolled clinical studies, among adult chronic ITP patients receiving Revolade (n = 446), 17 subjects experienced a total of 19 TEEs, which included (in descending order of occurrence) deep vein thrombosis (n = 6), pulmonary embolism (n = 6), acute myocardial infarction (n = 2), cerebral infarction (n = 2), embolism (n = 1) (see Section 4.4 Special Warnings and Precautions for Use).

 In the single arm, open label study in SAA, patients had bone marrow aspirates evaluated for cytogenetic abnormalities. Eight patients had a new cytogenetic abnormality reported, including 5 patients who had changes in chromosome 7 (see Section 4.4 Special Warnings and Precautions for Use).
In the single arm, open label study in SAA, patients had bone marrow aspirates evaluated for cytogenetic abnormalities. Eight patients had a new cytogenetic abnormality reported, including 5 patients who had changes in chromosome 7 (see Section 4.4 Special Warnings and Precautions for Use). New or worsening liver function laboratory abnormalities (CTCAE Grade 3 and Grade 4) in the Revolade D1-M6 cohort were 15.2% and 2.2% for AST, 26.4% and 4.3% for ALT, and 12.1% and 1.1% for bilirubin, respectively.
New or worsening liver function laboratory abnormalities (CTCAE Grade 3 and Grade 4) in the Revolade D1-M6 cohort were 15.2% and 2.2% for AST, 26.4% and 4.3% for ALT, and 12.1% and 1.1% for bilirubin, respectively.

 A significantly greater proportion of patients treated with eltrombopag (75%) compared with placebo (21%) had a platelet response (at least one platelet count > 50 x 109/L during the first 12 weeks of randomised treatment in absence of rescue therapy) (odds ratio: 11.7 [95% CI: 4.0, 34.5], p < 0.001).
A significantly greater proportion of patients treated with eltrombopag (75%) compared with placebo (21%) had a platelet response (at least one platelet count > 50 x 109/L during the first 12 weeks of randomised treatment in absence of rescue therapy) (odds ratio: 11.7 [95% CI: 4.0, 34.5], p < 0.001). A significantly greater proportion of patients treated with eltrombopag (36%) compared with placebo (0%) had a platelet response (platelet counts > 50 x 109/L for at least 60% of assessments between weeks 2 and 6) (odds ratio: 5.8 [95% CI: 1.2, 28.9], p = 0.002).
A significantly greater proportion of patients treated with eltrombopag (36%) compared with placebo (0%) had a platelet response (platelet counts > 50 x 109/L for at least 60% of assessments between weeks 2 and 6) (odds ratio: 5.8 [95% CI: 1.2, 28.9], p = 0.002).
 The overall and complete haematological response rates at Year 1 (n=78) are 56.4% and 38.5% and at Year 2 (n=62) are 38.7% and 30.6%, respectively.
The overall and complete haematological response rates at Year 1 (n=78) are 56.4% and 38.5% and at Year 2 (n=62) are 38.7% and 30.6%, respectively. Revolade was discontinued after 16 weeks if no haematological response or transfusion independence was observed. Patients who responded continued therapy in an extension phase of the study.
Revolade was discontinued after 16 weeks if no haematological response or transfusion independence was observed. Patients who responded continued therapy in an extension phase of the study. Plasma eltrombopag Cmax and AUC(0-T) estimates for patients with HCV enrolled in phase III studies TPL103922 (ENABLE 1) and TPL108390 (ENABLE 2) are presented for each dose studied in Table 21. A higher eltrombopag exposure was observed in patients with HCV at a given eltrombopag dose.
Plasma eltrombopag Cmax and AUC(0-T) estimates for patients with HCV enrolled in phase III studies TPL103922 (ENABLE 1) and TPL108390 (ENABLE 2) are presented for each dose studied in Table 21. A higher eltrombopag exposure was observed in patients with HCV at a given eltrombopag dose. The pharmacokinetic parameters of eltrombopag after administration of Revolade 150 mg once daily 45 patients with definitive immunosuppressive therapy-naïve severe aplastic anaemia are shown in Table 22.
The pharmacokinetic parameters of eltrombopag after administration of Revolade 150 mg once daily 45 patients with definitive immunosuppressive therapy-naïve severe aplastic anaemia are shown in Table 22.

 Molecular formula: C25H22N4O4.2(C2H7NO).
Molecular formula: C25H22N4O4.2(C2H7NO).