What is in this leaflet
This leaflet answers some common questions about Rifadin.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Rifadin against the benefits he/she expects it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine.
You may need to read it again.
What Rifadin is used for
Rifadin is an antibiotic that is used in combination with other medicines to treat tuberculosis, also known as TB. TB is a bacterial infection, which mainly affects the lungs, but it can also spread to other organs in the body.
Rifadin is also used to treat leprosy, a skin condition that has many forms.
Rifadin is also used to prevent certain diseases occurring where you may be in contact with, or have had contact with, a person known to have the disease or is known to be able to pass it on to others. Examples of such diseases are meningitis, a serious infectious disease (an inflammation of the membranes that cover the brain and spinal cord), affecting children and young adults, and pneumonia, conjunctivitis and meningitis caused by Haemophilus influenzae, a bacterium in the respiratory tract.
This medicine is available only with a doctor's prescription.
Before you take it
When you must not take it
Do not use Rifadin if:
You have an allergy to Rifadin (rifampicin) or any other rifamycin antibiotics or any of the ingredients listed at the end of this leaflet. Symptoms of an allergic reaction may include skin rash, itching, difficulty breathing or swallowing, and swelling of the face, lips, tongue and throat.
You have jaundice (yellowing of the eyes and skin).
You are taking combination saquinavir/ritonavir medications.
You are breast-feeding or planning to breastfeed. Rifadin passes into breast milk and there is a possibility your baby may be affected.
If the packaging is torn or shows signs of tampering.
If the expiry date (exp) printed on the pack has passed. If you use this medicine after the expiry date has passed, it may not work as well.
If you are not sure whether you should start using Rifadin, talk to your doctor.
Before you start to take it
Tell your doctor if:
You have any type of liver disease.
You have any allergies to any other medicines or any other substances, such as foods, preservatives or dyes.
You have a problem with bleeding or tendency to bruise easily.
You are taking other antibiotics at the same time.
You have diabetes.
You are pregnant or intend to become pregnant. Your doctor will discuss the possible risks and benefits of using Rifadin during pregnancy.
You are breast-feeding or plan to breast-feed. Rifadin should not be used while breast-feeding.
If you have not told your doctor about any of the above, tell them before you are given Rifadin.
Urine, faeces, saliva, sputum, sweat, tears and teeth may be coloured red-orange, yellow or brown by Rifadin. Soft contact lenses may be permanently stained.
Taking other medicines
Tell your doctor if you are taking any other medicines, including medicines that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some drugs should not be taken with Rifadin. These include:
- The combination of saquinavir and ritonavir, antiviral agents used to treat acquired immune deficiency syndrome (AIDS) and human immunodeficiency virus (HIV) infections.
- Halothane, a general anaesthetic (a sleep inducing drug)
- Daclatasvir, simeprevir, sofosbuvir and telaprevir, antiviral agents used to treat Hepatitis C
- Cephazolin and other cephalosporin antibiotics used to treat infection.
Some medicines and Rifadin may interfere with each other. These include:
- Antacids, used for heart burn and indigestion
- Atovaquone, used to treat a respiratory infection in acquired immune deficiency syndrome (AIDS)
- Ketoconazole, used for fungal infections
- Enalapril, used to treat high blood pressure and heart problems
- Isoniazid and p-aminosalicylic acid (PAS), used for TB (tuberculosis).
Rifadin may reduce the effectiveness of a wide variety of medicines or they may affect how well Rifadin works. These include certain medicines used for:
- Decreasing the clotting of the blood
- Controlling and preventing seizures
- Heart disease and high blood pressure
- Breast cancer treatment or prevention
- Sedation
- Bacterial infections
- Fungal infections
- Inflammatory conditions
- Contraception
- High blood cholesterol
- Diabetes
- TB and leprosy
- Malaria
- Rejection of transplanted organs
- Thyroid deficiency states
- Pain
- Nocturnal cramps
- Breathing difficulties
- Anxiety or depression
- Treatment of certain mental illnesses
- Treatment of HIV (Human Immunodeficiency Virus) infections.
- Nausea and vomiting
Your doctor or pharmacist may have more information on medicines to be careful with or to avoid while taking Rifadin.
How to take it
How much to take
Your doctor will decide what dose and for how long you will receive Rifadin.
How to take it
Follow all directions given to you by your doctor or pharmacist carefully.
Swallow Rifadin tablets and capsules whole with a glass of water.
Do not crush or chew the tablets. These tablets have a special coating to stop them dissolving until they have gone through the stomach and into the intestines, where they start to work. If you chew them, the coating is destroyed.
Rifadin should be taken on an empty stomach at least 30 minutes before or 2 hours after a meal.
If you need to take an antacid, take it at least 1 hour after your dose of Rifadin.
If you forget to take it
Take the dose as soon as you remember, and then resume taking Rifadin as directed.
Do not take a double dose to make up for the missed dose.
If you are unsure about taking the next dose, speak to your doctor or pharmacist.
If you have trouble remembering when to take your medication, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (Australia: telephone 13 11 26, New Zealand: telephone 0800 POISON or 0800 764766) for advice, or go to casualty at your nearest hospital, if you think that you or anyone else has taken too much Rifadin.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much Rifadin you may have symptoms of nausea, vomiting, abdominal pain, itchy skin, headache, fatigue, dizziness, swelling and abnormal heart beating.
While you are taking it
Things you must do
Take Rifadin exactly as directed or as your doctor has prescribed. If you miss doses, side effects may occur more often and may be more serious than usual.
You should see your doctor monthly for a check-up.
If you develop itching with swelling or skin rash or difficulty breathing, or if you turn yellow while you are taking Rifadin do not take any more Rifadin and tell your doctor immediately.
If you get severe diarrhoea tell your doctor, pharmacist or nurse immediately. Do this even if it occurs several weeks after you have stopped taking Rifadin. Diarrhoea may mean that you have a serious condition affecting your bowel. You may need urgent medical care. Do not take any diarrhoea medicine without first checking with your doctor.
If you get a sore white mouth or tongue while taking or soon after stopping Rifadin, tell your doctor. Also tell your doctor if you get vaginal itching or discharge. This may mean you have a fungal infection called thrush. Sometimes the use of Rifadin allows fungi to grow and the above symptoms to occur. Rifadin does not work against fungi.
If you become pregnant while you are taking Rifadin tell your doctor.
If you are using oral contraceptives you should change to alternative methods of birth control while you are taking Rifadin.
If you are about to start taking any new medicine, tell your doctor or pharmacist that you are taking Rifadin.
If you have to have any blood or urine tests tell your doctor you are being given Rifadin. Rifadin may affect the results of some blood and urine tests.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking Rifadin.
Things you must not do
Do not stop taking Rifadin because you feel better.
If you do not complete the full treatment prescribed by your doctor, some of the bacteria causing your infection may not be killed. These bacteria may continue to grow and multiply so that your infection may not clear completely or it may return.
Side effects
Check with your doctor as soon as possible if you have any problems while being treated with Rifadin, even if you do not think the problems are connected with the medicine or are not listed in this leaflet.
Like other medicines, Rifadin can cause some side effects. If they occur, most are likely to be minor and temporary. However, some may be serious and need medical attention.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- Yellow discolouration of skin or eyes
- Heartburn, loss of appetite, nausea, vomiting, upset stomach, abdominal discomfort, wind, cramps or diarrhoea
- Drowsiness, fatigue, inability to concentrate, confusion, or mental problems
- Poor coordination, muscle weakness, pain in the fingers or toes, or numbness
- Oral thrush - white, furry, sore tongue and mouth
- Vaginal thrush - sore and itchy vagina and/or discharge
- Conjunctivitis or visual disturbances
- Menstrual disturbances.
Tell your doctor immediately if you notice any of the following:
- Severe red and/or itchy skin, blisters or pimples, bleeding, peeling or bruising of the skin
- Swelling of the face, lips, tongue or throat which may cause difficulty in breathing or swallowing
- Itching, weakness, loss of appetite, nausea, vomiting, abdominal pain, yellowing of the eyes or skin or dark urine
- Shortness of breath and wheezing
- Blood in the urine or any other urination disturbances
- Severe bleeding or bruising more easily than normal
- Fever, chills, headache or dizziness
- Bone pain.
Some people may get other side effects while taking Rifadin. Some of these side effects (for example changes in liver function) can only be found when your doctor does tests from time to time to check your progress.
Ask your doctor or pharmacist if you don't understand anything in this list.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Urine, faeces, saliva, sputum, sweat, tears and teeth may be coloured red-orange, yellow or brown by Rifadin. Soft contact lenses may be permanently stained.
After finishing Rifadin
Tell your doctor immediately if you notice any of the following side effects, particularly if they occur several weeks after stopping treatment with Rifadin:
- Severe abdominal cramps or stomach cramps
- Watery and severe diarrhoea, which may also be bloody
- Fever, in combination with one or both of the above.
These are rare but serious side effects. You may have a serious condition affecting your bowel, which may need urgent medical attention. However, this side effect is rare.
Do not take any diarrhoea medicine without first checking with your doctor.
After taking it
Storage
Keep Rifadin where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Rifadin capsules
Keep the capsules in a cool dry place where the temperature stays below 25°C.
Rifadin tablets#
Keep the tablets in a cool dry place where the temperature stays below 25°C.
Rifadin syrup
Keep the syrup in a cool dry place where the temperature stays below 25°C.
Disposal
If your doctor tells you to stop taking this medication or it has passed the expiry date, ask your pharmacist what to do with any left over.
Product description
What it looks like
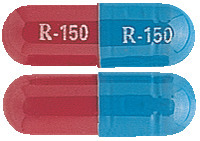
Rifadin capsules
Rifadin 150 mg capsules are blue/red capsules. They come in packs of 100 capsules.
Rifadin 300 mg capsules are red capsules. They come in packs of 100 capsules.
Rifadin tablets#
Rifadin 600 mg tablets are cyclamen red capsule shaped sugar coated tablets. They come in packs of 30 tablets.
Rifadin syrup
Rifadin syrup is a red liquid supplied in 60 mL bottles.
Ingredients
Rifadin preparations do not contain azo dyes.
Diabetics should note that Rifadin syrup contains 40% w/v of sugar.
Rifadin syrup contains potassium metabisulfite.
Rifadin capsules
Active Ingredient:
Rifadin 150 mg - 150 mg active per capsule
Rifadin 300 mg - 300 mg active per capsule
Inactive Ingredients:
The 150 mg and 300 mg capsules also contain:
- maize starch
- magnesium stearate
The capsule shell also contains
- titanium dioxide
- erythrosine
- indigo carmine
- gelatin
Rifadin tablets#
Active Ingredient:
Rifadin 600 mg - 600 mg active per tablet
Inactive Ingredients:
- sodium lauryl sulfate
- microcrystalline cellulose
- lactose monohydrate
- calcium stearate
- carmellose sodium
- maize starch
- magnesium stearate
The sugar coating also contains:
- acacia
- povidone
- erythrosine
- titanium dioxide
- sucrose
- purified talc
- magnesium carbonate hydrate
- kaolin
- colloidal anhydrous silica
- gelatin
Rifadin syrup
Active Ingredient:
Rifadin 100 mg/5mL - 100 mg active per 5 mL of syrup
Inactive Ingredients:
- agar
- sucrose
- methyl hydroxybenzoate
- propyl hydroxybenzoate
- potassium sorbate
- saccharin
- sodium metabisulfite
- polysorbate 80
- raspberry essence (PI 458)
- diethanolamine
- purified water
Manufacturer/Sponsor
Rifadin is supplied in Australia by:
sanofi-aventis australia pty ltd
12-24 Talavera Road
Macquarie Park NSW 2113
Australian Registration Numbers:
AUST R 233442 (150 mg capsules blister pack)
AUST R 233443 (300 mg capsules blister pack)
AUST R 227519 (600 mg tablet blister pack) #
AUST R 10114 (150 mg capsules)#
AUST R 10111 (300 mg capsules)#
AUST R 10112 (600 mg tablets)#
AUST R 10113 (syrup)
#Not marketed
Rifadin is supplied in New Zealand by:
sanofi-aventis new zealand limited
Level 8, 56 Cawley Street
Ellerslie
Auckland
This leaflet was prepared in: April 2020
® Registered Trademark
rifadin-ccdsv12-cmi11-apr20
Published by MIMS June 2020


 C43H58N4O12.
C43H58N4O12.