1 Name of Medicine
Relugolix, estradiol (as hemihydrate) and norethisterone acetate.
2 Qualitative and Quantitative Composition
Each Ryeqo 40/1/0.4 (Ryeqo) film-coated tablet contains 40 mg relugolix, 1 mg estradiol (as hemihydrate) and 0.5 mg norethisterone acetate.
Each film-coated tablet contains approximately 80 mg of lactose monohydrate.
For the full list of excipients, see Section 6.1 List of Excipients.
3 Pharmaceutical Form
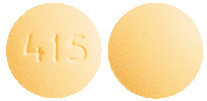
Film-coated tablet.
Light yellow to yellow, round film-coated tablet of 8 mm with "415" on one side and plain-faced on the other side.
4.1 Therapeutic Indications
Ryeqo is indicated in adult women of reproductive age for:
treatment of moderate to severe symptoms of uterine fibroids;
symptomatic treatment of endometriosis in women with a history of previous medical or surgical treatment for their endometriosis (see Section 5.1 Pharmacodynamic Properties).
4.2 Dose and Method of Administration
Dosage.
One tablet of Ryeqo must be taken once daily, at about the same time with or without food. Tablets should be taken with some liquid as needed (see Section 5.2 Pharmacodynamic Properties).
Bone mineral density (BMD) loss and osteoporosis.
Assessment of BMD by dual-energy X-ray absorptiometry (DXA) is recommended at baseline and after one year of treatment.
Use is recommended to be limited to 24 months, with extension of therapy conditional on stability of DXA and reassessment of risk/benefit in the individual patient by the treating physician.
Annual DXA is recommended while taking Ryeqo (see Section 4.4 Special Warnings and Precautions for Use).
Initiation of treatment.
Pregnancy must be ruled out prior to initiating treatment with Ryeqo.
When starting treatment, the first tablet must be taken within 5 days of the onset of menstrual bleeding. If treatment is initiated on another day of the menstrual cycle, irregular and/or heavy bleeding may initially occur.
Ryeqo can be taken without interruption. Discontinuation should be considered when the patient enters menopause, as the symptoms of both uterine fibroids and endometriosis are known to regress when menopause begins.
Contraceptive properties of Ryeqo.
Any hormonal contraception needs to be stopped prior to initiation of treatment, as concomitant use of hormonal contraceptives is contraindicated (see Section 4.3 Contraindications).
Nonhormonal methods of contraception must be used for at least 1 month after initiation of treatment.
After at least one month of Ryeqo use, Ryeqo inhibits ovulation in women taking the recommended dose and provides adequate contraception.
Women of childbearing potential must be advised that ovulation will return rapidly after discontinuing treatment. Therefore, a discussion with the patient, regarding appropriate contraceptive methods, must therefore take place prior to discontinuing treatment and alternative contraception needs to be started immediately after discontinuation of treatment (see Section 4.4 Special Warnings and Precautions for Use).
Method of administration.
Oral use. Ryeqo can be taken with or without food. Tablets should be taken with some liquid as needed.
Missed doses.
If a dose is missed, treatment must be taken as soon as possible and then continue the next day at the usual time.
If doses are missed for 2 or more consecutive days, a nonhormonal method of contraception is to be used for the next 7 days of treatment (see Section 4.6 Fertility, Pregnancy and Lactation).
Dosage adjustment.
Renal impairment.
No dose adjustment for Ryeqo in patients with mild, moderate, or severe renal impairment is required (see Section 5.2 Pharmacokinetic Properties).
Hepatic impairment.
No dose adjustment for Ryeqo in patients with mild or moderate hepatic impairment is required (see Section 5.2 Pharmacokinetic Properties). Ryeqo is contraindicated in women with severe liver disease if liver function values have not returned to normal (see Section 4.3 Contraindications).4.3 Contraindications
Hypersensitivity to the active substance(s) or to any of the excipients listed in Section 6.1 List of Excipients.
Venous thromboembolic disorder, past or present (e.g. deep venous thrombosis, pulmonary embolism).
Arterial thromboembolic cardiovascular disease, past or present (e.g. myocardial infarction, cerebrovascular accident, ischemic heart disease).
Known thrombophilic disorders (e.g. protein C, protein S or antithrombin deficiency or activated protein C (APC) resistance, including Factor V Leiden (see Section 4.4 Special Warnings and Precautions for Use)).
Known osteoporosis.
Headaches with focal neurological symptoms or migraine headaches with aura (see Section 4.4 Special Warnings and Precautions for Use).
Known or suspected sex steroid influenced malignancies (e.g. of the genital organs or the breasts).
Presence or history of liver tumours (benign or malignant) (see Section 4.4 Special Warnings and Precautions for Use).
Presence or history of severe hepatic disease as long as liver function values have not returned to normal.
Pregnancy or suspected pregnancy and breastfeeding (see Section 4.6 Fertility, Pregnancy and Lactation).
Genital bleeding of unknown aetiology.
Concomitant use of hormonal contraceptives.
4.4 Special Warnings and Precautions for Use
Ryeqo must only be prescribed after careful diagnosis.
Medical examination/consultation.
Prior to the initiation or reinstitution of Ryeqo, a complete medical history (including family history) must be taken. Blood pressure must be measured and a physical examination must be performed guided by the contraindications (see Section 4.3 Contraindications) and warnings for use (see Section 4.4 Special Warnings and Precautions for Use). During treatment, periodic check-ups must be carried out according to standard clinical practice.
Any hormonal contraception needs to be stopped prior to initiation of Ryeqo (see Section 4.3 Contraindications). Nonhormonal methods of contraception must be used for at least 1 month after initiation of treatment. Pregnancy must be ruled out prior to administering or re-initiation of Ryeqo.
Identified precautions.
Risk of thromboembolic disorders. The use of medicinal products containing an estrogen and a progestogen increases the risk of arterial or venous thromboembolism (ATE or VTE) compared with no use.
The risk of ATE/VTE with Ryeqo has not been established. Ryeqo contains doses of estrogen and progestogen lower than the doses used in combined hormonal contraceptives and are provided in combination with relugolix, a gonadotropin-releasing hormone (GnRH) receptor antagonist that suppresses ovarian production of estrogen and progesterone. Estradiol levels with Ryeqo are in the range observed in the early follicular phase of the menstrual cycle (see Section 5.1 Pharmacodynamic Properties).
If an ATE/VTE occurs, treatment must be discontinued immediately. Ryeqo is contraindicated in women with past or present venous or arterial thromboembolic disease (see Section 4.3 Contraindications).
Risk factors for venous thromboembolism (VTE).
The risk for venous thromboembolic complications in women using a product with an estrogen and progestogen may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see Table 1).
 The increased risk of thromboembolism in pregnancy, and particularly the 6-week period of the puerperium, must be considered (for information on "Pregnancy and lactation" (see Section 4.6 Fertility, Pregnancy and Lactation)).
The increased risk of thromboembolism in pregnancy, and particularly the 6-week period of the puerperium, must be considered (for information on "Pregnancy and lactation" (see Section 4.6 Fertility, Pregnancy and Lactation)).
Symptoms of VTE (deep vein thrombosis and pulmonary embolism).
In the event of symptoms, women must be advised to get urgent medical attention and to inform the physician that she is taking Ryeqo.
Symptoms of deep vein thrombosis (DVT) can include:
unilateral swelling of the leg and/or foot or along a vein in the leg;
pain or tenderness in the leg which may be felt only when standing or walking;
increased warmth in the affected leg; red or discoloured skin on the leg.
Symptoms of pulmonary embolism (PE) can include:
sudden onset of unexplained shortness of breath or rapid breathing;
sudden coughing which may be associated with haemoptysis;
sharp chest pain;
severe light headedness or dizziness;
rapid or irregular heartbeat.
Some of these symptoms (e.g. "shortness of breath", "coughing") are non-specific and might be misinterpreted as more common or less severe events (e.g. respiratory tract infections).
Risk factors for arterial thromboembolism (ATE).
Epidemiological studies have associated the use of estrogen/progestogen products with an increased risk for arterial thromboembolism (myocardial infarction) or for cerebrovascular accident (e.g. transient ischaemic attack, stroke). Arterial thromboembolic events may be fatal.
The risk for arterial thromboembolic complications in women using a product with an estrogen and progestogen may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see Table 2).

Symptoms of ATE.
In the event of symptoms, women must be advised to get urgent medical attention and to inform the physician that she is taking Ryeqo.
Symptoms of a cerebrovascular accident can include:
sudden numbness or weakness of the face, arm or leg, especially on one side of the body;
sudden trouble walking, dizziness, loss of balance or coordination;
sudden confusion, trouble speaking or understanding;
sudden trouble seeing in one or both eyes;
sudden, severe or prolonged headache with no known cause;
loss of consciousness or fainting with or without seizure.
Temporary symptoms suggest the event is a transient ischaemic attack.
Symptoms of myocardial infarction can include:
pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm, or below the breastbone;
discomfort radiating to the back, jaw, throat, arm, stomach;
feeling of being full, having indigestion or choking;
sweating, nausea, vomiting or dizziness;
extreme weakness, anxiety, or shortness of breath;
rapid or irregular heartbeats.
Risk of bone loss. In some women treated with Ryeqo, who had normal bone mineral density (BMD) at start of treatment, a bone loss varying from > 3-8% was reported. Following an initial non-clinically relevant decrease in BMD, it stabilised after 12-24 weeks of treatment and thereafter remained stable (as measured up to 2 years). The mean decrease in BMD during the first year of treatment with Ryeqo was 0.69%. However, decreases of > 3% were seen in 21% of the patients.
Therefore, a DXA scan is recommended at baseline, after the first 52 weeks of treatment, and annually thereafter. Depending on the degree of change in BMD, the benefit and risks of Ryeqo may need to be reconsidered.
The benefits and risks of Ryeqo in patients with a history of a low trauma fracture or other risk factors for osteoporosis or bone loss, including those taking medications that may affect BMD, should be considered prior to initiating treatment. It is recommended to perform a DXA scan before commencing treatment with Ryeqo in these patients. Ryeqo should not be initiated if the risk associated with BMD loss exceeds the potential benefit of the treatment to verify that the patient does not have an unwanted degree of BMD loss, that exceeds the benefit of treatment with Ryeqo.
Liver tumours or liver disease. Ryeqo is contraindicated in women with liver tumours, benign or malignant; or liver disease as long as liver function values have not returned to normal (see Section 4.3 Contraindications). Treatment must be discontinued if jaundice develops.
In clinical trials, asymptomatic transient elevations of serum alanine aminotransferase (ALT) at least 3 times the upper limit of the reference range occurred in < 1% of participants treated with Ryeqo. Acute liver test abnormalities may necessitate the discontinuation of Ryeqo use until the liver tests return to normal.
Change in menstrual bleeding pattern. Patients must be informed that treatment with Ryeqo usually leads to a reduction in menstrual blood loss or amenorrhoea within the first 2 months of treatment.
Women receiving Ryeqo, for the treatment of uterine fibroids, were likely to have amenorrhoea (51.6%) or cyclic bleeding (15.4%), with the rest (31.9%) having an irregular bleeding pattern at the week 24 assessment. Furthermore, at the week 52 assessment 70.6% of women receiving Ryeqo were likely to have amenorrhoea. For those patients with endometriosis, the majority of patients (65.2%) are likely to have amenorrhoea at the week 24 assessment.
In case of persistent excessive bleeding, patients must notify their physician.
Contraceptive properties of Ryeqo. Ryeqo provides adequate contraception when used for at least 1 month (see Section 4.2 Dose and Method of Administration). However, women of childbearing potential must be advised that ovulation will return rapidly after discontinuing treatment. Therefore, alternative contraception needs to be started immediately after discontinuation of treatment.
Reduced ability to recognise pregnancy. Women who take Ryeqo commonly experience amenorrhoea or a reduction in the amount, intensity, or duration of menstrual bleeding.
This change in menstrual bleeding pattern may reduce the ability to recognise the occurrence of a pregnancy in a timely manner. Perform pregnancy testing if pregnancy is suspected and discontinue treatment if pregnancy is confirmed.
Uterine fibroid prolapse or expulsion. Submucosal uterine fibroids are common (15% to 20% of women with uterine fibroids) and some may prolapse through the cervix or be expelled, sometimes with transient worsening of uterine bleeding. Women known or suspected to have submucosal uterine fibroids must be advised regarding the possibility of uterine fibroid prolapse or expulsion when treated with Ryeqo and should contact their physician if severe bleeding reoccurs after bleeding symptoms have improved while being treated with Ryeqo.
Depression. Carefully observe women with a history of depression and discontinue Ryeqo if depression recurs to a serious degree. Data are limited on the association of Ryeqo or other products containing estradiol and progestins with onset of depression or exacerbation of existing depression. Women must be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment.
Hypertension. Although small increases in blood pressure have been reported in women taking Ryeqo, clinically relevant increases are rare. However, if sustained clinically significant hypertension develops during the use of Ryeqo, hypertension should be treated, and the benefit of continued therapy should be assessed. If treatment with Ryeqo is discontinued, use may be resumed if normotensive values can be achieved with antihypertensive treatment.
Gallbladder disease. Conditions such as gallbladder disease, cholelithiasis and cholecystitis have been reported to occur or worsen with estrogen and progestogen use, including Ryeqo, but the evidence of an association with Ryeqo is inconclusive.
Lactose. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicinal product.
Use in hepatic impairment.
See Section 4.4 Special Warnings and Precautions for Use, Liver tumours or liver disease.
Use in renal impairment.
The exposure to relugolix is increased in patients with moderate or severe renal impairment (see Section 5.2 Pharmacokinetic Properties), although no dose adjustment is required (see Section 4.2 Dose and Method of Administration). The amount of relugolix removed by haemodialysis is unknown.
Use in the elderly.
There is no relevant use of Ryeqo in the elderly population in the indications.
Paediatric use.
The safety and efficacy of Ryeqo in children and adolescents aged less than 18 years have not been established. No data are available.
Effects on laboratory tests.
The use of estrogens and progestogens may influence the results of certain laboratory tests, including biochemical parameters of liver, thyroid, adrenal and renal function, plasma levels of (carrier) proteins, e.g. corticosteroid binding globulin and lipid/lipoprotein fractions, parameters of carbohydrate metabolism and parameters of coagulation and fibrinolysis. Changes generally remain within the normal laboratory range.4.5 Interactions with Other Medicines and Other Forms of Interactions
Recommendations regarding interactions with Ryeqo are based on evaluations of interactions for the individual components.
Potential for other medicinal products to affect the components of Ryeqo.
Relugolix. Oral P-glycoprotein (P-gp) inhibitors.
Concomitant use of Ryeqo with oral P-gp inhibitors is not recommended. Relugolix is a substrate of P-gp (see Section 5.2 Pharmacokinetic Properties) and in an interaction study with erythromycin, a P-gp and moderate cytochrome P450 (CYP) 3A4 inhibitor, the area under the curve (AUC) and maximum concentration (Cmax) of relugolix were increased by 4.1-fold and 3.8-fold, respectively. Concomitant use of P-gp inhibitors may increase the exposure of relugolix, including certain anti-infective medicinal products (e.g. erythromycin, clarithromycin, gentamicin, tetracycline), anti-fungal medicinal products (ketoconazole, itraconazole), antihypertensive medicinal products (e.g. carvedilol, verapamil), antiarrhythmic medicinal products (e.g. amiodarone, propafenone, quinidine), antianginal medicinal products (e.g. ranolazine), cyclosporine, human immunodeficiency virus (HIV) or hepatitis C virus (HCV) protease inhibitors (e.g. ritonavir). If concomitant use with once or twice daily oral P-gp inhibitors is unavoidable (e.g. azithromycin), take Ryeqo first, and separate dosing with the P-gp inhibitor by at least 6 hours and monitor patients more frequently for adverse reactions.
Strong cytochrome P450 3A4 (CYP3A4) and/or P-gp inducers.
Co-administration of Ryeqo with strong CYP3A4 and/or P-gp inducers is not recommended. In a clinical interaction study with rifampicin, a strong CYP3A4 and P-gp inducer, the Cmax and AUC of relugolix were reduced by 23% and 55%, respectively. Medicinal products that cause strong CYP3A4 and/or P-gp induction, such as anticonvulsants (e.g. carbamazepine, topiramate, phenytoin, phenobarbital, primidone, oxcarbazepine), anti-infective medicinal products (e.g. rifampicin, rifabutin, griseofulvin); St. John's wort (Hypericum perforatum); bosentan and HIV or HCV protease inhibitors (e.g. ritonavir,) and non-nucleoside reverse transcriptase inhibitors (e.g. efavirenz), may reduce the plasma concentrations of relugolix and may result in a decrease in therapeutic effects.
CYP3A4 inhibitors.
Concomitant use of relugolix with strong CYP3A4 inhibitors devoid of P-gp inhibition (voriconazole) did not increase the exposure of relugolix in a clinically meaningful manner. Furthermore, in a clinical interaction study, concomitant administration with atorvastatin, a weak CYP3A4 enzyme inhibitor, did not change the exposure of relugolix in a clinically meaningful manner.
Estradiol and norethisterone acetate. CYP3A4 inhibitors.
Medicinal products that inhibit the activity of hepatic drug-metabolising enzymes, e.g. ketoconazole, may increase circulating concentrations of the estrogen and norethisterone components in Ryeqo.
CYP enzyme inducers.
The metabolism of estrogens and progestogens may be increased by concomitant use of substances known to induce drug-metabolising enzymes, specifically cytochrome P450 enzymes, such as anticonvulsants (e.g. phenobarbital, phenytoin, carbamazepine) and anti-infectives (e.g. rifampicin, rifabutin, nevirapine, efavirenz).
Ritonavir and nelfinavir, although known as strong inhibitors, are also inducers and may decrease the exposure of estrogens and progestogens.
Herbal preparations containing St John's Wort (Hypericum perforatum) may induce the metabolism of estrogens and progestogens. Clinically, an increase in estrogen metabolism may lead to decreased effectiveness with regard to protection of bone loss. Therefore, long-term concomitant use of liver enzyme inducers with Ryeqo is not recommended.
Potential for the components of Ryeqo to affect other medicinal products.
Relugolix.
Relugolix is a weak inducer of CYP3A4. After co-administration with daily 40 mg doses of relugolix, the AUC and Cmax of midazolam, a sensitive CYP3A4 substrate, were decreased by 18% and 26%, respectively. However, based on the clinical study with midazolam, clinically meaningful effects of relugolix on other CYP3A4 substrates are not expected.
Relugolix is an inhibitor of breast cancer resistant protein (BCRP) in vitro, therefore, an interaction study was conducted with rosuvastatin, a BCRP and organic anion transporting polypeptide 1B1 (OATP1B1) substrate. After coadministration with daily 40 mg doses of relugolix, the AUC and Cmax of rosuvastatin were decreased by 13% and 23%, respectively. The effects are not considered clinically meaningful and therefore no dose adjustments of rosuvastatin upon concomitant use are recommended. Clinical effects of Ryeqo on other BCRP substrates have not been evaluated and the relevance for other BCRP substrates is unknown.
Relugolix may cause saturation of intestinal P-gp at the 40 mg dose, as relugolix exhibits more than dose proportional pharmacokinetics over the dose range of 10-120 mg, which could result in increased absorption of co-administered medicines that are sensitive substrates of P-gp. No clinically significant differences in the pharmacokinetics of dabigatran etexilate (P-gp substrate) were observed upon co-administration with relugolix, clinically meaningful effects of relugolix on other P-gp substrates are not expected.
Estradiol and norethisterone acetate.
Estrogen and progestogen medicinal products may affect the metabolism of certain other active substances. Accordingly, plasma concentrations may either increase (e.g. cyclosporin) or decrease (e.g. lamotrigine) with use of Ryeqo. Dose adjustment of these medicinal products may be necessary.4.6 Fertility, Pregnancy and Lactation
Effects on fertility.
Ryeqo inhibits ovulation and often causes amenorrhoea. Ovulation and menstrual bleeding will return rapidly after discontinuing treatment. There are no data on fertility following treatment with Ryeqo in women with endometriosis (see Section 5.1 Pharmacodynamic Properties).
Ryeqo inhibits ovulation in women taking the recommended dose and provides adequate contraception. A nonhormonal contraceptive method is recommended for use for 1 month after initiation of treatment and for 7 days following 2 or more missed consecutive doses. Concomitant use of hormonal contraceptives is contraindicated (see Section 4.3 Contraindications).
Women of childbearing potential must be advised that ovulation will return rapidly after discontinuing Ryeqo. A discussion with the patient, regarding appropriate contraceptive methods, must therefore take place prior to discontinuing treatment and alternative contraception needs to be started immediately after discontinuation of treatment (see Section 4.4 Special Warnings and Precautions for Use).
In a fertility and early embryonic development study in rats, oral administration of relugolix at doses up to 1000 mg/kg/day had no adverse effects on fertility, mating or early embryonic development. However, the binding affinity of relugolix for rat GnRH receptors is greater than 1000-fold less than for human GnRH, and the rat study only assessed non-pharmacological effects of relugolix. In a 39-week study in monkeys, relugolix did not induce toxicities in male reproductive organs but caused reversible decreases in ovary weight and corpora lutea in females at ≥ 5 mg/kg/day and decreased frequency of menses at 50 mg/kg/day (14 and 179 times the clinical exposure at the recommended clinical dose of 40 mg daily, based on AUC, respectively). In human GnRH-receptor knock-in mice, administration of relugolix at oral doses of ≥ 100 mg/kg twice daily to female mice induced a constant diestrus phase and decreased ovarian and uterine weights, which were reversible following cessation of treatment. In male knock-in mice, oral administration of relugolix decreased prostate and seminal vesicle weights at doses ≥ 3 mg/kg twice daily, which were reversible except for testis weight (not fully recovered in 28 days).
(Category D)
There is a limited amount of data from the use of relugolix in pregnant women. Studies in animals have shown that exposure to relugolix early in pregnancy may increase the risk of early pregnancy loss. Based on the pharmacological effects, an adverse effect on pregnancy cannot be excluded.
Ryeqo is contraindicated during pregnancy (see Section 4.3 Contraindications). Discontinue use of treatment if pregnancy occurs.
There appears to be little or no increased risk of harmful effects in children born to women who have used estrogens and progestogens as an oral contraceptive inadvertently during early pregnancy. The increased risk of VTE during the postpartum period must be considered when restarting Ryeqo (see Section 4.4 Special Warnings and Precautions for Use).
In an embryo-foetal development study in rabbits, oral administration of relugolix to pregnant rabbits during the period of organogenesis resulted in total litter loss and decreased number of live foetuses at 9 mg/kg/day (with an exposure comparable with the human exposure at the recommended clinical dose of 40 mg daily, based on AUC). No treatment related malformations were observed in surviving foetuses. No treatment related effects were observed at 3 mg/kg/day (about 0.2-fold the human exposure) or lower. The binding affinity of relugolix for rabbit GnRH receptors is unknown, although the affinity is likely greater in rabbits than in rats.
In a similar embryo-foetal development study in rats, oral administration of relugolix to pregnant rats during the period of organogenesis did not affect embryofetal development at up to 1,000 mg/kg/day (> 700 times the human exposure), a dose at which maternal toxicity (decreased body weight gain and food consumption) was observed. Since the binding affinity of relugolix for the rat GnRH receptor is more than 1,000-fold less than in humans, the rat is a pharmacologically unresponsive model, and the study represented an assessment of non-pharmacological targets of relugolix during pregnancy.
In animal studies, maternal administration of high doses of estrogens has produced urogenital malformations in the offspring. The relevance of these animal findings for the clinical use of estradiol is uncertain, but is considered likely to be low. Animal studies have also shown that high doses of progestogens can cause masculinisation of the female foetus.
Results from nonclinical studies indicate that relugolix is excreted into the milk of lactating rats. No data are available regarding the presence of relugolix or its metabolites in human milk or its effect on the breastfed infant. Detectable amounts of estrogen and progestogens have been identified in the breast milk of women receiving estrogen plus progestogen therapy. An effect on breastfeeding newborns/infants cannot be excluded.
Breastfeeding is contraindicated during the use of Ryeqo (see Section 4.3 Contraindications) and for 2 weeks following discontinuation of Ryeqo.
In lactating rats administered a single oral dose of 30 mg/kg radiolabelled relugolix on post-partum day 14, relugolix and/or its metabolites were present in milk at concentrations up to 10-fold higher than in plasma at 2 hours post-dose decreasing to low levels by 48 hours post-dose. The majority of relugolix-derived radioactivity in milk consisted of unchanged relugolix.4.7 Effects on Ability to Drive and Use Machines
Ryeqo has no or negligible influence on the ability to drive and use machines.
4.8 Adverse Effects (Undesirable Effects)
Summary of the safety profile.
The most frequent adverse drug reactions in patients being treated for uterine fibroids were hot flush (8.3%) and uterine bleeding (4.7%). For those patients being treated for endometriosis, the most common adverse drug reactions were headache (17.0%) and hot flush (11.7%).
Adverse drug reactions listed in Table 3 and Table 4 are classified according to frequency and system organ class. Within each frequency grouping, adverse drug reactions are presented in order of decreasing seriousness. Frequencies are defined as very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), and not known (cannot be estimated from available data).
Tabulated list of adverse drug reactions in patients with uterine fibroids (see Table 3).
 Tabulated list of adverse drug reactions in patients with endometriosis (see Table 4).
Tabulated list of adverse drug reactions in patients with endometriosis (see Table 4).

Reporting suspected adverse effects.
Reporting suspected adverse reactions after registration of the medicinal product is important. It allows continued monitoring of the benefit-risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions at www.tga.gov.au/reporting-problems.4.9 Overdose
Single doses of relugolix up to 360 mg (9 times the recommended clinical dose of 40 mg) have been administered to healthy men and women and were generally well tolerated.
Overdoses up to 2 times the recommended dose have been reported during the clinical development of relugolix in combination with estradiol and norethisterone acetate without reports of adverse events.
Supportive care is recommended if an overdose occurs. The amount of relugolix, estradiol or norethisterone removed by haemodialysis is unknown.
Serious ill effects have not been reported following acute ingestion of large doses of estrogen containing drug products by young children. Overdose of estradiol and norethisterone acetate may cause nausea and vomiting, and withdrawal bleeding may occur in women.
For information on the management of overdose, contact the Poisons Information Centre on 13 11 26 (Australia).
5 Pharmacological Properties
5.1 Pharmacodynamic Properties
Pharmacotherapeutic group: Pituitary and hypothalamic hormones and analogues, anti-gonadotrophin-releasing hormones:
ATC code: H01CC54
Mechanism of action.
Relugolix is a non-peptide GnRH receptor antagonist that binds to and inhibits GnRH receptors in the anterior pituitary gland. In humans, inhibition of GnRH receptor results in a dose dependent decrease in the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary gland. As a result, circulating concentrations of LH and FSH are reduced. The reduction in FSH concentrations prevents follicular growth and development, thereby reducing the production of estrogen. Prevention of an LH surge inhibits ovulation and development of the corpus luteum, which precludes the production of progesterone. Therefore, Ryeqo provides adequate contraception when taken for at least 1 month (see Section 4.2 Dose and Method of Administration).
Estradiol is the same as the endogenously produced hormone and is a potent agonist of the nuclear estrogen receptor (ER) subtypes. Exogenously administered estradiol alleviates symptoms associated with a hypoestrogenic state, such as vasomotor symptoms and bone mineral density loss.
Norethisterone acetate is a synthetic progestogen. As estrogens promote the growth of the endometrium, unopposed estrogens increase the risk of endometrial hyperplasia and cancer. The addition of a progestogen reduces the estrogen-induced risk of endometrial hyperplasia in non-hysterectomised women.
Clinical trials.
Effects on pituitary and ovarian hormones. After administration of relugolix, rapid, dose-dependent decreases in circulating concentrations of LH, FSH, and estradiol are observed. Near maximum decreases in estradiol concentrations is noted with a 40 mg dose to within the postmenopausal range. Across clinical studies, average estradiol concentrations were consistently maintained at least 10 picogram/mL higher with Ryeqo compared with relugolix alone. In the phase 3 clinical studies, in patients with uterine fibroids, with Ryeqo, median estradiol pre-dose concentrations after 24 weeks were approximately 33 picogram/mL, and in those with endometriosis were approximately 38 picogram/mL corresponding with estradiol concentrations associated with the early follicular phase of the menstrual cycle. Progesterone levels in both populations were maintained at < 3.0 nanogram/mL with Ryeqo.
Effects on ovulatory function. In a single cohort study in healthy premenopausal women, administration of Ryeqo once daily for 84 days substantially suppressed follicular growth throughout the 84-day treatment period (mean dominant follicle size of approximately 6 mm) and ovulation was inhibited in 100% of women as assessed by the Hoogland Skouby score. After discontinuation of treatment, all women assessed (66 of 67) returned to ovulation within 43 days (mean 23.5 days).
Uterine fibroids. Efficacy and safety over 24 weeks.
The efficacy and safety of Ryeqo once daily in patients with uterine fibroids was assessed in two replicate, 24 week, multinational, randomised, double blind, placebo-controlled studies in patients aged 18-50 with heavy menstrual bleeding associated with uterine fibroids (studies L1 and L2). Patients were required to have uterine fibroids confirmed by ultrasound and menstrual blood loss (MBL) volume of ≥ 80 mL, as assessed by the alkaline hematin method.
Both studies had 3 treatment groups: Women were randomised to receive relugolix 40 mg + estradiol 1 mg and norethisterone acetate 0.5 mg (E2/NETA) (Ryeqo) for 24 weeks, or placebo for 24 weeks, or relugolix 40 mg for 12 weeks followed by relugolix 40 mg co-administered with E2/NETA for 12 weeks. The median age of women was 42 years, and mean body mass index was 31.7 kg/m2. Approximately 49.4% of women were Black, 44.7% were White, and 5.9% were of other races.
Reduction in heavy menstrual bleeding.
In both studies, a statistically significant higher percentage of responders, defined as MBL volume of < 80 mL and at least a 50% reduction from baseline in MBL volume, was observed in favour of women treated with Ryeqo compared with placebo (Table 5). Reductions in MBL volume were seen as early as the first assessment (week 4). The results for other secondary endpoints related to bleeding are as shown in Table 5. All key secondary endpoints were alpha controlled.

Bone mineral density (BMD) measurements over 104 weeks.
The effect of Ryeqo on BMD was evaluated by DXA every 12 weeks. A total of 477 women who completed the 24-week pivotal studies (Study L1 and L2) were enrolled into a 28 week, open-label, single arm extension study (Study L3), where all women received Ryeqo. A total of 228 women who completed the extension study were enrolled into an additional 52-week study (randomised withdrawal study) where they were re-randomised to receive either Ryeqo or placebo (see Table 6).
 In the Ryeqo group, LS mean percent changes from baseline in BMD to week 36 and week 52 at the lumbar spine were -0.73% and -0.80%, respectively. While the upper bound of the 95% CI for week was below 0, the mean change from baseline was not considered clinically meaningful because the lower bound remained greater than -2.2%, the threshold considered clinically meaningful. The placebo group who subsequently received Ryeqo after 24 weeks of placebo treatment showed similar percent change in BMD, from baseline at the lumbar spine. During the randomised withdrawal study the LS mean percent change from the week 52 assessment in the Ryeqo group was 0.81%, whilst for those patients who completed 104 weeks of Ryeqo treatment the LS mean percent change from baseline was 0.04% (n = 32).
In the Ryeqo group, LS mean percent changes from baseline in BMD to week 36 and week 52 at the lumbar spine were -0.73% and -0.80%, respectively. While the upper bound of the 95% CI for week was below 0, the mean change from baseline was not considered clinically meaningful because the lower bound remained greater than -2.2%, the threshold considered clinically meaningful. The placebo group who subsequently received Ryeqo after 24 weeks of placebo treatment showed similar percent change in BMD, from baseline at the lumbar spine. During the randomised withdrawal study the LS mean percent change from the week 52 assessment in the Ryeqo group was 0.81%, whilst for those patients who completed 104 weeks of Ryeqo treatment the LS mean percent change from baseline was 0.04% (n = 32).
BMD measurements over 12 weeks in women with uterine fibroids treated with relugolix monotherapy.
In women treated with relugolix monotherapy for 12 weeks, in studies L1 and L2, BMD at the lumbar spine decreased by 2.0% and 1.92%, respectively from baseline. The difference in percent change in BMD between women treated with Ryeqo and relugolix monotherapy at week 12 was statistically significant, demonstrating the effectiveness of using relugolix in combination with E2/NETA (Ryeqo) to mitigate bone loss.
To compare effects of Ryeqo on percent change in BMD over 52 weeks treatment, an observational study of untreated age matched women with uterine fibroids was conducted to characterise longitudinal BMD of premenopausal women aged 18 to 50 years (natural history study). The percentage changes in BMD with Ryeqo for up to 52 weeks of treatment are consistent with those observed in this age-matched cohort of premenopausal women with uterine fibroids. Mean percent changes in BMD over 52 weeks indicated a slight decrease in BMD in age groups of 35 and older which was only slightly lower in women who received Ryeqo in comparison to women of this age group in the natural history study.
Effects on endometrium.
A subset of women underwent endometrial biopsy at baseline and at week 24 and at week 52. No cases of endometrial hyperplasia were identified in women with uterine fibroids.
Endometriosis. Efficacy and safety over 24 weeks.
The efficacy and safety of Ryeqo once daily, in patients with endometriosis was assessed in two replicate, 24-week, multinational, randomised, double-blind, placebo-controlled studies in patients aged 18-50 with moderate to severe pain associated with endometriosis (Studies S1 and S2). Patients were required to have endometriosis confirmed by direct visualisation during surgery and/or histological confirmation and were required to have moderate to severe pain as assessed based on an 11-point numerical rating scale (NRS).
Both studies had three treatment arms: women were randomised to receive relugolix 40 mg + estradiol 1 mg and norethisterone acetate 0.5 mg (E2/NETA) (Ryeqo) for 24 weeks, or placebo for 24 weeks, or relugolix 40 mg for 12 weeks followed by relugolix 40 mg co-administered with E2/NETA for 12 weeks. Patients were eligible for inclusion if they had moderate to severe pain before the screening period until after the run-in period (i.e. at least two cycles). A high percentage (83.2%) of the study population of Studies S1 and S2 reported having undergone previous surgeries/procedures for endometriosis treatment. A low percentage (8%) of the study population did not report previous surgical or medical treatment before inclusion into the studies. At baseline, most patients (92.6%) used analgesics for pelvic pain, including 29.1% of patients in Study S1 and 48.4% of patients in Study S2 who used opioids. The most frequently reported other pharmacotherapies for endometriosis included dienogest (19.4%), estrogen progestin oral contraceptive (15.2%) and GnRH agonists (7.6%). The median age of women was 34 years, and mean body mass index was 26 kg/m2. Approximately 91% of women were White, 6% were Black, and 3% were of other races.
Reduction in pain.
Studies S1 and S2 had two co-primary endpoints. The first co-primary endpoint was a responder analysis where a responder was defined as a woman who achieved a reduction from baseline in dysmenorrhea (DYS) NRS of at least 2.8 points over the last 35 days of treatment, without an increase in analgesic use (nonsteroidal anti-inflammatory drug or opioid). The second co-primary endpoint was a responder analysis where a responder was defined as a woman who achieved a reduction from baseline in non-menstrual pelvic pain (NMPP) NRS score of at least 2.1 points over the last 35 days of treatment, without an increase in analgesic use (nonsteroidal anti-inflammatory drug or opioid) for pain associated with endometriosis.
In both studies (S1 and S2), a statistically significant higher percentage of responders was observed in favour of women treated with Ryeqo compared with placebo (see Table 7).
 Key secondary efficacy endpoints included changes from baseline in the Endometriosis Health Profile-30 (EHP-30) pain domain scores (a measure of the effect of pain on daily activities), dysmenorrhea NRS scores, NMPP NRS scores, dyspareunia NRS scores and opioid use. The results for the key secondary endpoints were generally similar between studies demonstrating statistically significant differences compared with placebo (see Table 8). All key secondary endpoints were alpha controlled.
Key secondary efficacy endpoints included changes from baseline in the Endometriosis Health Profile-30 (EHP-30) pain domain scores (a measure of the effect of pain on daily activities), dysmenorrhea NRS scores, NMPP NRS scores, dyspareunia NRS scores and opioid use. The results for the key secondary endpoints were generally similar between studies demonstrating statistically significant differences compared with placebo (see Table 8). All key secondary endpoints were alpha controlled.

Efficacy over 104 weeks.
Upon completion of the 24-week Studies S1 and S2, eligible participants could enroll in an 80-week, open-label, single-arm extension study (S3), where all women received Ryeqo. The primary efficacy endpoints for study S3 were defined in a manner analogous to the co-primary endpoints for Studies S1 and S2. For women originally randomised to Ryeqo in Studies S1 and S2, the reduction in dysmenorrhea and NMPP NRS scores were maintained for up to 104 weeks, whereas for women who were originally randomised to placebo, a reduction in their endometriosis-associated pain was observed after receiving Ryeqo during Study S3 (see Table 9).

Bone mineral density (BMD) measurements over 104 weeks.
The effect of Ryeqo on BMD was evaluated by DXA every 12 weeks. A total of 802 women who completed the 24-week pivotal studies (Study S1 and S2) were enrolled into the extension study (Study S3), where all patients received Ryeqo (see Table 10).
 In the Ryeqo group, LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.69% and -0.45%, respectively. In the placebo group (received placebo for 24 weeks followed by Ryeqo for 80 weeks) LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.09% and -0.09%, respectively.
In the Ryeqo group, LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.69% and -0.45%, respectively. In the placebo group (received placebo for 24 weeks followed by Ryeqo for 80 weeks) LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.09% and -0.09%, respectively.
To compare effects of Ryeqo on percent change in BMD over 52 weeks treatment, an observational study of untreated age-matched women with endometriosis was conducted to characterise longitudinal BMD of premenopausal women aged 18-50 years (natural history study). Through 52 weeks of observation, there was minimal change in BMD with Ryeqo compared with those in an age-matched cohort of premenopausal women with endometriosis.
Effects on endometrium.
In the pivotal studies, no cases of endometrial hyperplasia or endometrial carcinoma assessed by biopsy were observed in women treated with Ryeqo for up to 52 weeks.
5.2 Pharmacokinetic Properties
The pharmacokinetic parameters of relugolix, estradiol (E2), total estrone (E1), and norethisterone (NET) following oral administration of a single Ryeqo tablet to healthy postmenopausal women under fasted conditions are summarized in Table 11.
 The pharmacokinetic parameters of relugolix, estradiol (E2), total estrone (E1), and norethisterone (NET) at steady state after once daily administration of Ryeqo for 6 weeks to healthy premenopausal women are summarized in Table 12.
The pharmacokinetic parameters of relugolix, estradiol (E2), total estrone (E1), and norethisterone (NET) at steady state after once daily administration of Ryeqo for 6 weeks to healthy premenopausal women are summarized in Table 12.

Absorption.
The absorption of relugolix after oral administration is primarily mediated by the P-gp efflux transporter, for which relugolix is a substrate. After oral administration, relugolix is rapidly absorbed, reaching an initial peak by 0.25 hours post dose followed by one or more subsequent absorption peaks through up to 12 hours post dose. The absolute bioavailability of relugolix is 11.6%. After administration of Ryeqo with a high fat, high-calorie meal, the AUC0-∞ and Cmax of relugolix were decreased by 38% and 55%, respectively, compared with the fasted state.
After oral administration of a single dose of Ryeqo in the fasted state, unconjugated estradiol concentrations increased slowly with mean concentrations reaching peak concentrations at 8 hours post dose. After administration of Ryeqo following consumption of a high-fat, high-calorie meal, no clinically meaningful effects of food on the exposure to estradiol or estrogenic metabolites were observed.
After oral administration, norethisterone acetate undergoes rapid biotransformation in the intestine and liver to norethisterone (NET). After oral administration of a single dose of Ryeqo in the fasted state, NET concentrations were initially quantifiable at 0.5 hours post dose, increasing rapidly thereafter with mean concentrations reaching peak concentrations within 1 hour.
Food effects.
Administration with food reduced the AUC and Cmax of relugolix by 38% and 55%, respectively, relative to fasted conditions; however, the decrease in exposure to relugolix is considered not to be clinically meaningful. No clinically meaningful effects of food on the exposure to estradiol, estrogenic metabolites, or norethisterone were observed.
Distribution.
Relugolix is 68% to 71% bound to human plasma proteins with a mean whole blood-to-plasma ratio of 0.78. Estradiol and norethisterone circulating in the blood bind to a similar extent to sex hormone-binding globulin (SHBG; 36% to 37%) and to albumin (61%), while only approximately 1-2% are unbound. The value for apparent volume of distribution (Vz) of 19 x 103 L derived from the absolute bioavailability study after intravenous administration indicates that relugolix distributes widely into tissues. The distribution of exogenous and endogenous estradiol is similar. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs.
Metabolism.
In vitro studies indicate that the primary CYP enzymes contributing to the overall hepatic oxidative metabolism of relugolix were CYP3A4/5 (45%) > CYP2C8 (37%) > CYP2C19 (< 1%) with the oxidative metabolites, metabolite A and metabolite B, formed by CYP3A4/5 and CYP2C8, respectively.
The metabolism of exogenous and endogenous estradiol is similar. Metabolism of estradiol occurs mainly in the liver and the gut but also in target organs and involves the formation of less active or inactive metabolites, including estrone, catechol estrogens and several estrogen sulphates and glucuronides. Estrogens are excreted with the bile, hydrolysed, and reabsorbed (enterohepatic circulation), and mainly eliminated in urine in biologically inactive form. Oxidation of estrone and estradiol involves cytochrome P450 enzymes, mainly CYP1A2, CYP1A2 (extra hepatic), CYP3A4, CYP3A5, and CYP1B1 and CYP2C9.
The most important metabolites of norethisterone are isomers of 5-alpha-dihydro-norethisterone and of tetrahydro-norethisterone, which are excreted mainly in the urine as sulphate or glucuronide conjugates.
Excretion.
Once absorbed, approximately 20% of relugolix is eliminated as unchanged active substance in the urine and 80% is eliminated through metabolism by multiple minor metabolic pathways and/or biliary secretion of unchanged active substance. Approximately 38% of the administered dose is excreted as metabolites (other than metabolite C) in the faeces and urine. Metabolite C, which is formed by intestinal microflora, is the primary metabolite in faeces (51%) and further reflects non absorbed active substance.
The mean terminal phase elimination half-life (t1/2) of relugolix, estradiol, and norethisterone following single dose administration of the Ryeqo tablet are 61.5 hours, 16.6 hours, and 10.9 hours, respectively. Steady state of relugolix is reached after 12 to 13 days of once daily administration. The degree of accumulation of relugolix upon once daily administration is approximately 2-fold, reflecting an effective half-life of approximately 25 hours and supporting once daily administration of relugolix.
The accumulation for E2 and NET upon once daily administration are reported to be 33% to 47%, although when coadministered with relugolix, a weak inducer of intestinal (presystemic) CYP3A mediated metabolism, the accumulation for E2 is expected to be similar or slightly lower.
Linearity/nonlinearity.
Relugolix is associated with greater than proportional increases in exposure with respect to dose, within the dose range from 1 to 80 mg, which is most pronounced at doses greater than 20 mg; and thought to be related to the saturation of intestinal P-gp, resulting in an increase in oral bioavailability.
The pharmacokinetics of relugolix upon once daily administration of 40 mg relugolix is time independent.
Special populations.
The single dose pharmacokinetic parameters were not different between Japanese and Caucasian healthy subjects, indicating absence of ethnic sensitivity on the pharmacokinetics of relugolix. Population PK analysis suggests that there are no clinically meaningful differences in exposure of relugolix based on age, race or ethnicity, weight, or BMI. As both estradiol and norethisterone acetate are well known components of hormonal combination products, no studies in special populations were conducted.
Renal impairment.
After administration of a single 40 mg dose of relugolix to patients with severe renal impairment, the exposure AUC0-∞ and Cmax of relugolix were increased by 1.5 and 1.1-fold, respectively, compared with healthy control subjects with normal renal function. After administration of a single 40 mg dose of relugolix to patients with moderate renal impairment, the exposure AUC0-∞ and Cmax of relugolix both were increased by 1.5-fold compared with healthy control subjects with normal renal function. Mild renal impairment was not a significant covariate for any of the pharmacokinetic parameters of relugolix in a population pharmacokinetic model. Although caution should be used to treat patients with moderate or severe renal impairment (see Section 4.4 Special Warnings and Precautions for Use), no dose adjustments with Ryeqo in patients with mild, moderate or severe renal impairment are required (see Section 4.2 Dose and Method of Administration).
The effect of end-stage renal disease with or without haemodialysis on the pharmacokinetics of estradiol, norethisterone and relugolix, the components of Ryeqo, in premenopausal women have not been evaluated. The amount of relugolix, estradiol or norethisterone removed by haemodialysis is unknown.
Hepatic impairment.
Ryeqo must not be used in patients with severe hepatic impairment (see Section 4.3 Contraindications). No dose adjustments for Ryeqo in patients with mild or moderate hepatic impairment are required (see Section 4.2 Dose and Method of Administration). After administration of a single 40 mg dose of relugolix to patients with mild hepatic impairment, the AUC0-∞ and Cmax of relugolix were decreased by 31% and 24%, respectively, compared with healthy control subjects with normal hepatic function. After administration of a single 40 mg dose of relugolix to patients with moderate hepatic impairment, the AUC0-∞ and Cmax of relugolix were decreased by 5% and increased by 1.2-fold, respectively, compared with healthy control subjects with normal hepatic function.
5.3 Preclinical Safety Data
Non-clinical studies have not been conducted with relugolix in combination with estradiol and norethisterone acetate.
Genotoxicity.
Relugolix was not mutagenic in the in vitro bacterial reverse mutation (Ames) assay or clastogenic in the in vitro chromosomal aberration assay in Chinese hamster lung cells or the in vivo rat bone marrow micronucleus assay.
There is limited evidence available in the literature suggesting that estradiol may be weakly genotoxic at high doses. No evidence could be found for an increase in the rate of gene mutation in bacterial or mammalian cells, but there was some evidence for the induction of chromosomal aberrations and aneuploidy in mammalian cells, and two groups reported an increase in the incidence of sister chromatid exchanges, indicative of DNA damage. Neither of these latter effects were induced by estradiol in human lymphocyte cultures. Importantly, there was no evidence for increased micronuclei formation in well controlled rodent bone marrow assays.
Carcinogenicity.
Relugolix was not carcinogenic in mice at oral doses up to 100 mg/kg/day or rats at oral doses up to 600 mg/kg/day, with exposures in both species higher than 250 times the human exposure at the recommended clinical dose of 40 mg daily, based on AUC. Since the binding affinity of relugolix for GnRH receptors in rats is more than 1000-fold less than in humans, the rat model only addressed the carcinogenic potential of any off-target effects of relugolix and its metabolites (and not malignancies arising from the pharmacodynamic effect of relugolix).
Supra-physiological doses of estradiol have been associated with the induction of tumours in estrogen-dependent target organs in all rodent species tested. The relevance of these findings with respect to humans has not been established.6 Pharmaceutical Particulars
6.1 List of Excipients
Lactose monohydrate, mannitol (E421), sodium starch glycollate, hyprolose (E463), magnesium stearate (E572), hypromellose type 2910 (E464), titanium dioxide (E171), triacetin (E1518), iron oxide yellow (E172).
6.2 Incompatibilities
Not applicable.
6.3 Shelf Life
In Australia, information on the shelf life can be found on the public summary of the Australian Register of Therapeutic Goods (ARTG). The expiry date can be found on the packaging.
6.4 Special Precautions for Storage
Store below 30°C.
6.5 Nature and Contents of Container
High-density polyethylene (HDPE) bottles with desiccant, closed with an induction sealed child resistant polypropylene cap.
Pack sizes.
28 film coated tablets (1 x bottle) or 84 film coated tablets (3 x bottles).
Not all pack sizes may be marketed.
6.6 Special Precautions for Disposal
In Australia any unused medicine or waste material should be disposed of by taking to your local pharmacy.
7 Medicine Schedule (Poisons Standard)
(Schedule 4) Prescription Only Medicine.
Summary Table of Changes


 The increased risk of thromboembolism in pregnancy, and particularly the 6-week period of the puerperium, must be considered (for information on "Pregnancy and lactation" (see Section 4.6 Fertility, Pregnancy and Lactation)).
The increased risk of thromboembolism in pregnancy, and particularly the 6-week period of the puerperium, must be considered (for information on "Pregnancy and lactation" (see Section 4.6 Fertility, Pregnancy and Lactation)).
 Tabulated list of adverse drug reactions in patients with endometriosis (see Table 4).
Tabulated list of adverse drug reactions in patients with endometriosis (see Table 4).

 In the Ryeqo group, LS mean percent changes from baseline in BMD to week 36 and week 52 at the lumbar spine were -0.73% and -0.80%, respectively. While the upper bound of the 95% CI for week was below 0, the mean change from baseline was not considered clinically meaningful because the lower bound remained greater than -2.2%, the threshold considered clinically meaningful. The placebo group who subsequently received Ryeqo after 24 weeks of placebo treatment showed similar percent change in BMD, from baseline at the lumbar spine. During the randomised withdrawal study the LS mean percent change from the week 52 assessment in the Ryeqo group was 0.81%, whilst for those patients who completed 104 weeks of Ryeqo treatment the LS mean percent change from baseline was 0.04% (n = 32).
In the Ryeqo group, LS mean percent changes from baseline in BMD to week 36 and week 52 at the lumbar spine were -0.73% and -0.80%, respectively. While the upper bound of the 95% CI for week was below 0, the mean change from baseline was not considered clinically meaningful because the lower bound remained greater than -2.2%, the threshold considered clinically meaningful. The placebo group who subsequently received Ryeqo after 24 weeks of placebo treatment showed similar percent change in BMD, from baseline at the lumbar spine. During the randomised withdrawal study the LS mean percent change from the week 52 assessment in the Ryeqo group was 0.81%, whilst for those patients who completed 104 weeks of Ryeqo treatment the LS mean percent change from baseline was 0.04% (n = 32). Key secondary efficacy endpoints included changes from baseline in the Endometriosis Health Profile-30 (EHP-30) pain domain scores (a measure of the effect of pain on daily activities), dysmenorrhea NRS scores, NMPP NRS scores, dyspareunia NRS scores and opioid use. The results for the key secondary endpoints were generally similar between studies demonstrating statistically significant differences compared with placebo (see Table 8). All key secondary endpoints were alpha controlled.
Key secondary efficacy endpoints included changes from baseline in the Endometriosis Health Profile-30 (EHP-30) pain domain scores (a measure of the effect of pain on daily activities), dysmenorrhea NRS scores, NMPP NRS scores, dyspareunia NRS scores and opioid use. The results for the key secondary endpoints were generally similar between studies demonstrating statistically significant differences compared with placebo (see Table 8). All key secondary endpoints were alpha controlled.

 In the Ryeqo group, LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.69% and -0.45%, respectively. In the placebo group (received placebo for 24 weeks followed by Ryeqo for 80 weeks) LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.09% and -0.09%, respectively.
In the Ryeqo group, LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.69% and -0.45%, respectively. In the placebo group (received placebo for 24 weeks followed by Ryeqo for 80 weeks) LS mean percent changes from baseline in BMD to week 52 and week 104 at the lumbar spine were -0.09% and -0.09%, respectively. The pharmacokinetic parameters of relugolix, estradiol (E2), total estrone (E1), and norethisterone (NET) at steady state after once daily administration of Ryeqo for 6 weeks to healthy premenopausal women are summarized in Table 12.
The pharmacokinetic parameters of relugolix, estradiol (E2), total estrone (E1), and norethisterone (NET) at steady state after once daily administration of Ryeqo for 6 weeks to healthy premenopausal women are summarized in Table 12.



