SUMMARY CMI
Rythmodan®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using Rythmodan®?
Rythmodan® contains the active ingredient disopyramide. Rythmodan® is used to treat and prevent ventricular arrhythmias (irregular heartbeat).
For more information, see Section 1. Why am I using Rythmodan®? in the full CMI.
2. What should I know before I use Rythmodan®?
Do not use if you have ever had an allergic reaction to Rythmodan or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use Rythmodan®? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with Rythmodan® and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use Rythmodan®?
- The dose of Rythmodan may be different for each person. Your doctor will decide the right dose for you.
- The daily dose of Rythmodan is usually taken in three equally divided doses.
More instructions can be found in Section 4. How do I use Rythmodan®? in the full CMI.
5. What should I know while using Rythmodan®?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using Rythmodan®? in the full CMI.
6. Are there any side effects?
All medicines have some unwanted side effects. Sometimes they are serious, but most of the time they are not. You may need medical treatment if you get some of the side effects.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
Rythmodan®
Active ingredient(s): disopyramide
Consumer Medicine Information (CMI)
This leaflet provides important information about using Rythmodan®. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using Rythmodan®.
Where to find information in this leaflet:
1. Why am I using Rythmodan®?
2. What should I know before I use Rythmodan®?
3. What if I am taking other medicines?
4. How do I use Rythmodan®?
5. What should I know while using Rythmodan®?
6. Are there any side effects?
7. Product details
1. Why am I using Rythmodan®?
Rythmodan® contains the active ingredient disopyramide. Rythmodan belongs to a group of medications called antiarrhythmics. This means it acts to correct irregular heartbeats to a normal rhythm and to slow an overactive heart.
Rythmodan® is used to treat and prevent ventricular arrhythmias.
Ask your doctor if you have any questions about why Rythmodan has been prescribed for you.
Your doctor may have prescribed Rythmodan for another reason. This medicine is available only with a doctor's prescription.
2. What should I know before I use Rythmodan®?
Warnings
Do not use Rythmodan® if:
- you are allergic to disopyramide, or any of the ingredients listed at the end of this leaflet.
Always check the ingredients to make sure you can use this medicine.
Some symptoms of an allergic reaction may include skin rash, itching, shortness of breath or swelling of the face, lips or tongue,which may cause difficulty in swallowing or breathing. - you are taking other antiarrhythmics or other heart medications without first discussing with your doctors.
- you are a child or adolescent, Rythmodan is not recommended for use in children.
- you are pregnant. Rythmodan is not recommended for use during pregnancy, unless you and your doctor or pharmacist have discussed the risks and benefits involved.
- Do not take Rythmodan after the expiry date (EXP) printed on the pack or if the packaging is torn of shows signs of tampering.
In that case, return it to your pharmacist.
Check with your doctor if you:
- Have any other medical conditions, especially the following:
- Diabetes
- Glaucoma or a family history of glaucoma
- Chronic muscular weakness (Myasthenia Gravis)
- Kidney problems
- Liver problems
- Heart problems including heart failure, heart attack, chest pain
- Low blood pressure (dizziness or light-headedness)
- Low or high potassium levels in your blood
- Bowel problems
- Difficult urination or
- Enlarged prostate
- All previous and pre-existing heart problems should be discussed with your doctor prior to starting Rythmodan
- Take any medicines for any other condition
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Rythmodan passes into breast milk and therefore there is a possibility that the breast-fed baby may be affected. Rythmodan is not recommended while you are breast-feeding.
Rythmodan is not recommended for use during pregnancy, unless you and your doctor or pharmacist have discussed the risks and benefits involved.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Rythmodan may interfere with each other. These include:
- Other antiarrhythmics used to treat heart conditions such as beta-blockers, amiodarone and calcium channel blockers
- Diuretics or antiangina medication
- Medicines used to treat epilepsy or fits, especially phenytoin and phenobarbitone
- Tricyclic and tetracyclic antidepressants
- Antibacterials to treat infections such as rifampicin, erythromycin, roxithromycin and clarithromycin
- Antifungals such as fluconazole, ketoconazole, itraconazole and amphotericin B
- Antimicrobials to treat infections, such as pentamidine
- Medications used to treat HIV
- Antihistamines such as terfenadine and astemizole
- Cisapride, a medicine used to treat stomach problems
- Pimozide, a medicine used to treat certain mental illnesses
- Laxatives for constipation
- Medicines for erectile dysfunction such as Viagra or Levitra
- Warfarin, a medicine used to prevent blood clots
These medicines may be affected by Rythmodan, or may affect how well it works. You may need different amounts of your medicine, or you may need to take different medicines. Your doctor or pharmacist will advise you.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Rythmodan®.
4. How do I use Rythmodan®?
How much to take / use
- The dose of Rythmodan may be different for each person. Your doctor will decide the right dose for you.
- Follow the instructions provided and use Rythmodan® until your doctor tells you to stop.
When to take / use Rythmodan®
- Rythmodan® should be used in a daily dosage of three equally divided doses.
- Rythmodan works best when there is a constant amount in the blood. To help keep the amount constant it is best to take the doses at evenly spaced intervals day and night.
- Take Rythmodan at about the same time each day for the best effect.
- It does not matter if Rythmodan is taken before or after food.
How to take Rythmodan®
- Swallow Rythmodan whole with plenty of fluid.
How long to take Rythmodan®
- Rythmodan must be taken everyday for as long as your doctor or pharmacist tells you.
- Rythmodan helps to control your condition but does not cure it.
- Do not stop taking your capsules because you are feeling better.
If you forget to use Rythmodan®
If it is almost time for your next dose (within 4 hours), skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed.
- Taking a double dose may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you use too much Rythmodan®
If you think that you have used too much Rythmodan®, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
If you take too much Rythmodan, you may feel cold and dizzy, light-headed, weak or you may faint. You may also experience palpitations (your heart may feel like it "skips a beat") and have difficulty breathing. You may notice your pulse is rapid and weak.
5. What should I know while using Rythmodan®?
Things you should do
Tell all the doctors, dentists, and pharmacists who are treating you that you are taking Rythmodan.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are taking Rythmodan.
If you plan to have surgery that needs a general anaesthetic, tell your doctor or dentist that you are taking Rythmodan.
Call your doctor as soon as possible if you:
- Have congestive heart disease or diabetes and experience hypoglycemia (low blood sugar), see side effects.
If the signs appear eat or drink a food containing sugar. - Experience dryness of the mouth, nose and throat persisting for more than 2 weeks. Rythmodan may cause dryness of the mouth, nose and throat. For temporary relief of mouth dryness melt bits of ice in your mouth.
- Become pregnant while taking Rythmodan.
Remind any doctor, dentist or pharmacist you visit that you are using Rythmodan®.
Things you should not do
- Do not give Rythmodan to anyone else, even if they have the same condition as you.
- Do not take Rythmodan to treat any other complaints unless your doctor or pharmacist tells you to.
- Do not stop taking Rythmodan, or lower the dosage, without checking with your doctor or pharmacist.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Rythmodan® affects you.
Rythmodan® may cause dizziness, light-headedness or fainting in some people. Make sure you know how you react to it before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed. If this occurs do not drive.
Drinking alcohol
Tell your doctor if you drink alcohol.
Alcohol may make the low blood sugar (hypoglycaemia) effect worse and/or increase the possibility of dizziness or fainting.
The effects of alcohol could be made worse while taking Rythmodan. It is not recommended that you drink alcohol while taking Rythmodan.
Looking after your medicine
- Keep your capsules in the pack until it is time to take them.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
When to discard your medicine (as relevant)
If your doctor or pharmacist tells you to stop taking Rythmodan or the capsules have passed their expiry date, ask your pharmacist what to do with any that are left over.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
The signs and symptoms of hypoglycaemia are: chills, cold sweats, confusion, cool and pale skin, drowsiness, headache, fast heartbeat, excessive hunger, nausea, shakiness, unusual tiredness/weakness. | Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Rythmodan® contains
| Active ingredient (main ingredient) | Disopyramide Either 100mg or 150mg |
| Other ingredients (inactive ingredients) | Magnesium stearate, maize starch, purified talc, gelatin, titanium dioxide. The 100mg capsules also contain yellow iron oxide and indigo carmine. |
Do not take this medicine if you are allergic to any of these ingredients.
Rythmodan does not contain lactose, sucrose, gluten, tartrazine or azo-dyes.
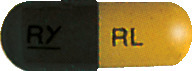
What Rythmodan® looks like
Rythmodan 100mg capsules are green and beige, marked with RY on one part and RL on the other. (AUST R 13537)
Rythmodan 150mg capsules# are white, marked with RY on one part and 150 on the other. (AUST R 13538)
Rythmodan is available in blister packs of 100 capsules.
#Not marketed
Who distributes Rythmodan®
Rythmodan is supplied in Australia by:
Pharmaco (Australia) Ltd
Level 13, 465 Victoria Avenue
Chatswood NSW 2067
Toll free number: 1800 201 564
This leaflet was prepared in August 2022.
Published by MIMS October 2022



 Chemical Formula: C21H29N3O.
Chemical Formula: C21H29N3O.