What is in this leaflet
This leaflet answers some common questions about Seasonique.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will provide.
If you have any concerns about this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Seasonique is used for
Seasonique is used to prevent pregnancy.
Seasonique is a combined oral contraceptive (COC), commonly known as a 'birth control pill' or 'the Pill.' It is an extended-dosing cycle taken continuously for 91 days. This means whilst taking Seasonique you may not have your monthly periods for up to 3 months (equivalent to 1 period every 3 months).
When taken correctly Seasonique prevents pregnancy in several ways:
- it inhibits the egg release by stopping it maturing
- it changes the cervical mucus consistency making it difficult for the sperm to reach the egg
- it changes the lining of the uterus making it less suitable for implantation
When the Pill is taken correctly by women under close observation in clinical trials, it is more than 99% effective in preventing pregnancy. However in real life the failure rate may increase if tablets are missed or taken incorrectly.
Like all other oral contraceptives Seasonique does not protect against HIV and other sexually transmitted infections (STIs). To protect yourself against STIs you need to use additional barrier contraceptives (e.g. condoms).
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor's prescription.
Before you take Seasonique
When you must not take it
Do not take Seasonique if you have an allergy to:
- any medicine containing ethinyloestradiol or levonorgestrel
- any of the ingredients listed at the end of this leaflet
- any other similar medicines (such as other oral contraceptives).
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take Seasonique if you have had or are at risk of having:
- deep vein thrombosis (DVT) - a blood clot in the blood vessels of the leg
- pulmonary embolism (PE) - a blood clot in the lungs
- venous thromboembolism (VTE) - a blood clot in the veins and heart
- arterial thromboembolism - (ATE) - a blood clot in the arteries
- a blood clot in other parts of the body
- heart valve or heart rhythm disorders that may be associated with the formation of blood clots
- heart attack or stroke
- chest pain (angina pectoris)
- high blood pressure which is uncontrolled
- some severe types of headache or migraine, including migraine accompanied by visual disturbances, weakness, speech disability or numbness in any part of your body
- A tumour that may grow under the influence of sex hormones (e.g. of the breast or genital organs)
- diabetes with blood vessel damage
- breast cancer or cancer of the lining of the womb, cervix or vagina, or you think you have these conditions
- unexplained vaginal bleeding
- liver tumour or liver disease (e.g. hepatitis and/or elevated liver enzymes)
- inflammation of the pancreas, which is associated with very high blood levels of triglycerides (fatty substances)
- yellowing of the whites of the eyes or of the skin (jaundice) during pregnancy or during previous use of an oral contraceptive
- high blood levels of cholesterol or triglycerides
- sickle cell anaemia
- changes in vision, such as blurring.
If you are not certain whether these may apply to you, or you are worried by anything in this list, tell your doctor.
Do not take this medicine if you are pregnant or you think you are pregnant. Pregnancy must be excluded before you start taking Seasonique.
Do not take this medicine in association with herbal remedy St John's Wort.
Do not give this medicine to a child.
Do not take this medicine if you have already experienced menopause.
Do not take this medicine after the expiry date (EXP) printed on the pack or if the packaging is torn or shows signs of tampering. If it is expired or damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take Seasonique
You must have a thorough medical check-up, including a Pap smear, breast check, blood pressure check and urine test.
Tell your doctor if you are allergic to any foods, dyes, preservatives or any other medicines.
Tell your doctor if you smoke. Oral contraceptives increase your risk of having a stroke or heart attack. The risk of serious side effects on the heart and blood vessels is even greater if you smoke and take oral contraceptives. The risk increases with age and with heavy smoking (15 or more cigarettes per day), especially in women older than 35 years. If you take Seasonique, you should not smoke.
The use of any combined hormonal contraceptive (CHC) increases the risk of VTE compared with no use. The VTE risk is highest in the first ever year of use. There is some evidence that the risk is increased when a CHC is re-started after a break in use of four weeks or more.
Tell your doctor (or go to Accident and Emergency immediately) if VTE symptoms develop, Symptoms can include:
- swelling of the leg and /or foot or along a vein in the leg
- pain or tenderness in the leg which may be felt only when standing or walking
- increased warmth in the affected leg; red or discoloured skin on the leg
- sudden onset of unexplained shortness of breath or rapid breathing
- sudden coughing
- sharp or sudden severe chest pain
- severe light headedness or dizziness
- sudden, severe or prolonged headache with no known cause
- rapid or irregular heartbeat
- sudden blurred vision or loss of sight in one or both eyes
There is some evidence that the use of CHCs may be associated with an increased risk of ATE.
Tell your doctor (or go to Accident and Emergency immediately) if ATE symptoms develop. Symptoms can include:
- sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- sudden trouble walking, dizziness, loss of balance or coordination
- sudden confusion, trouble speaking or understanding
- sudden blurred vision or loss of sight in one or both eyes
- sudden, severe or prolonged headache with no known cause
- loss of consciousness or fainting with or without seizure
- pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm or below the breastbone
- discomfort radiating to the back, jaw, throat, arm, stomach
- feeling of being full, having indigestion or choking
- sweating, nausea, vomiting or dizziness;
- extreme weakness, anxiety, or shortness of breath;
- rapid or irregular heartbeats.
Tell your doctor if you have any other health problems, especially:
- breast lumps, abnormal breast X-ray or mammogram
- diabetes
- heart disease
- high cholesterol or blood fats
- high blood pressure, a history of high blood pressure or high blood pressure during pregnancy
- migraine or other headaches
- epilepsy
- depression
- gallbladder disease
- fluid retention or kidney disease
- asthma
- fibroids
- yellowing of the whites of the eyes or skin (jaundice) during pregnancy or during previous oral contraceptive use
- hereditary angioedema (swelling of the face, lips, mouth, tongue or throat)
- chloasma (yellowish-brown patches on the skin, particularly the face.
- hepatitis or elevated liver enzymes
If you have any of these conditions you should have regular check-ups with your doctor to make sure that taking Seasonique is not making the conditions worse.
Tell your doctor if anyone in your family has had blood clots in the deep veins of the legs, a stroke or heart attack or you have any of the following conditions.
- obesity
- recent surgery or trauma
- recently had a baby
- lost a baby in the second trimester
- confined to bed rest for long periods.
Some women have an increased chance of blood clots due to factors such as age, family history of VTE, high body weight and smoking. Women assessed by their doctor as being at increased risk of VTE should not use Seasonique.
The risk of developing blood clots in the deep veins of your legs, which can break away and block a blood vessel elsewhere in your body, are increased if you have any of these conditions and use an oral contraceptive. Blood clots are a rare occurrence and can develop whether or not you are taking an oral contraceptive. They can also happen during pregnancy. The risk of having a blood clot is higher in oral contraceptive users than in non-users, but not as high as during pregnancy or just after having a baby.
VTE with any combined hormonal method of contraception is much less common than VTE in pregnancy and the period immediately after having a baby.
Pills containing levonorgestrel (such as Seasonique) or norethisterone appear to have lower VTE risk.
The risk of VTE with the COC is greatest for products containing over 50 micrograms of ethinyloestradiol. There is less risk for products containing less than 35 micrograms of ethinyloestradiol such as Seasonique. It is not known how Seasonique, with its 91-day cycle, influences the occurrence of such events in comparison to other levonorgestrel containing COCs, which are based on a 28-day cycle.
If you are at risk of prolonged immobilisation, due to major surgery or, any surgery to the legs or pelvis or major trauma), you should discuss this with your doctor. It is recommended to discontinue the use of Seasonique and not resume until two weeks after complete remobilisation. Another method of contraception should be used during this time to avoid unintentional pregnancy.
You should discuss this with your doctor before discontinuing the use of Seasonique.
Tell your doctor if you plan to become pregnant or are breast-feeding. Your doctor can discuss the risks and benefits involved with you.
If you have not told your doctor about any of the above, tell him/her before you start taking Seasonique.
Taking other medicines
Tell your doctor if you are taking any other medicines, including:
- all prescription medicines
- all medicines, vitamins, herbal supplements or natural therapies you buy without a prescription from a pharmacy, supermarket, naturopath or health food shop.
Some medicines may be affected by Seasonique or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor will advise you.
Tell your doctor or pharmacist if you are taking any of the following:
- rifampicin and rifabutin for the treatment of tuberculosis
- antibiotics such as ampicillin, other penicillins and tetracyclines
- anti-fungal agents such as griseofulvin
- medicines for epilepsy (such as phenytoin, primidone, carbamazepine and topiramate, phenobarbitone)
- ritonavir for the treatment of HIV infection.
- products used to treat hepatitis such as those containing ombitasvir, paritaprevir or dasabuvir
- modafinil used to treat excessive daytime sleepiness
- St. John's Wort, an ingredient in many medicines you can buy without a prescription from a pharmacy, health food shop or supermarket
- corticosteroids such as dexamethasone.
While you are taking any of these medicines and for the next 7 days after stopping them, you must also use an additional non-hormonal method of contraception (such as condoms or a diaphragm, but not the rhythm or temperature methods).
If you take rifampicin and some other medicines, you may need to use additional non-hormonal contraception for four weeks after finishing the course of treatment.
Concomitant use with products containing ombitasvir, paritaprevir, ritonavir or dasabuvir with or without ribavirin may increase liver enzymes.
If you are taking or begin taking these medicines while taking Seasonique, you must switch to an alternative method of contraception (e.g. progestogen-only contraception or non-hormonal methods) prior to commencing therapy.
Seasonique can be restarted 2 weeks following completion of treatment with this combination regimen.
Ask your doctor or pharmacist about how long you need to use additional non-hormonal contraception.
Tell your doctor or pharmacist if you are taking any of the following.
- atorvastatin used to treat high cholesterol
- indinavir for the treatment of HIV infection
- anti-fungal agents such as itraconazole and fluconazole
- paracetamol and ascorbic acid (Vitamin C).
- cyclosporin used to prevent organ rejection
- theophyllines used for asthma and other breathing difficulties
- corticosteroids
- lamotrigine used for seizures
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking Seasonique. Your doctor and pharmacist have more information on medicines to be careful with or avoid while you are taking this medicine.
How to take Seasonique
Follow all directions given to you by your doctor or pharmacist carefully. These directions may differ from the information contained in this leaflet.
Seasonique pack consists of 84 pink tablets of 150 micrograms levonorgestrel and 30 micrograms ethinyloestradiol and 7 white tablets containing 10 micrograms of ethinyloestradiol
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How to take it
The daily dosing regimen should start with the first tablet (#1) of Month 1 blister.
Take one tablet about the same time every day. Tablet taking is continuous for 91 days. You may take the tablets with or without food, and if necessary with a little liquid in the order shown at the blister pack.
Preparation of the pack
To help you keep track, there are 7 weekday sticker strips marked with the 7 days of the week. Choose the week sticker that starts with the day you begin taking the tablets. For example, if you start on a Wednesday, use the week sticker that starts with "WED". Stick the week sticker along the top of the Seasonique pack where it reads "Place week sticker here", so that the first day is above the tablet marked "1". There is now a day indicated above every tablet and you can see whether you have taken a certain pill. The arrows show the order you are to take the pills. Usually, so-called withdrawal bleeding starts when you are taking white tablets. Once you have taken the last white tablet, you should start with the following Seasonique pack, whether your bleeding has stopped or not. This means that you should start every pack on the same day of the week, and that the withdrawal bleed should occur on the same days each time. If you use Seasonique in this manner, you are protected against pregnancy during the whole 91 days. For continued protection against pregnancy make sure you have a new pack of Seasonique ready to start.
Do not confuse the tablets. One pink tablet containing levonorgestrel and ethinyloestradiol is taken daily for 84 consecutive days, followed by one white ethinyloestradiol tablet for 7 days.
When to take Seasonique
You must take Seasonique every day, regardless of how often you have sex.
The tablets must be taken every day at about the same time, if necessary with a little liquid, in the order shown on the blister pack. One tablet is to be taken daily for 91 consecutive days.
If you are concerned about this, please speak to your doctor or pharmacist.
Starting a hormonal contraceptive for the first time
To start taking Seasonique follow these steps:
- On the first day of your menstrual bleed, take a pink tablet containing levonorgestrel and ethinyloestradiol.
You may also begin on day 2-5 of the cycle, but then you must use extra protective measures (for example, a condom) for the first 7 days.
- One pink tablet should be taken daily for 84 consecutive days.
- One white tablet is taken for 7 consecutive days.
- A scheduled 'withdrawal' bleed should occur during the 7 days that the white tablets are taken.
Going on to further blister packs
Each subsequent 91-day cycle should be started without interruption on the same day of the week as you began your first dose of Seasonique, following the same schedule.
Switching from a different combined oral contraceptive, vaginal ring or transdermal patch
Follow the instructions below carefully.
When changing from a different combined oral contraceptive:
Follow the advice of your doctor. You should start with Seasonique on the day after the last active tablet (the last tablet containing the active substances) of your previous COC.
When changing from a vaginal ring or transdermal patch to Seasonique.
Follow the advice of your doctor. You should start using Seasonique on the day of removal but at the latest when the next application would have been due.
Switching from a progestogen-only contraceptive
You may switch any day from the progestogen-only pill (from an implant or the IUD on the day of its removal, from an injectable when the next injection would be due). In all of these cases you must use a barrier method of contraception (e.g. a condom) for the first 7 days of tablet-taking.
After having a miscarriage or abortion
Follow the advice of your doctor.
After having a baby
If you have just had a baby, talk to your doctor before you start taking Seasonique.
How long to take Seasonique
Continue taking your medicine for as long as your doctor tells you.
Your doctor may prescribe Seasonique for long periods, until you no longer need or want contraception.
If you are not sure how long you should be taking Seasonique, ask your doctor.
If you forget to take your tabets
White tablets: If you forget any of the white tablets (last 7 tablets in the pack), this has no effect on the reliability of Seasonique. Do not take the forgotten white tablet(s) and continue with the next tablet at the usual time.
Pink tablets: If you miss a pink tablet, depending on the day of the cycle on which the tablet has been missed, you may need to take additional contraceptive precautions, for example a barrier method such as a condom.
Take the pink tablets according to the following principles:
- If you are less than 12 hours late when taking a tablet, the protection against pregnancy is not reduced. Take the tablet as soon as you remember and then continue taking the tablets again at the usual time.
- If you are more than 12 hours late taking a tablet, the protection against pregnancy may be reduced. The greater the number of tablets you have forgotten the greater is the risk of becoming pregnant. There is a particularly high risk of becoming pregnant if you miss pink tablets at the beginning of the pack. Therefore you should follow the rules given below.
One pink tablet forgotten
One pink tablet forgotten between days 1-7
Take the tablet as soon as you remember even if this means taking two tablets at the same time. Continue taking the following tablets at the usual time. Use additional contraceptive precautions for the following 7 days e.g. a barrier method such as a condom. If you have had sex in the week before forgetting the tablet there is a possibility of pregnancy. So contact your doctor immediately.
One pink tablet forgotten between days 8-84
Take the tablet as soon as you remember even if this means taking two tablets at the same time. Continue taking the following tablets at the usual time. The protection against pregnancy is not reduced and you do not need to take extra contraceptive precautions.
More than one pink tablet forgotten in this pack
Days 1-7
If two pink tablets are missed, take two tablets as soon as you remember and additional two on the next day. Continue taking the following tablets at the usual time.
If 3 or more pink tablets are missed, do not take the forgotten tablets and continue taking the following tablets at the usual time. You may experience bleeding during the week following the missed tablets.
In any case use additional contraceptive precautions for the following 7 days e.g. a barrier method such as a condom. If you have had sex in the week before forgetting tablets there is a possibility of pregnancy. So contact your doctor immediately.
Days 8-84
If two pink tablets are missed, take two tablets as soon as you remember and additional two on the next day. Continue taking the following tablets at the usual time. Use additional contraceptive precautions for the following 7 days e.g. a barrier method such as a condom.
If 3 or more pink tablets are missed, do not take the forgotten tablets and continue taking the following tablets at the usual time. You may experience bleeding during the week following the missed tablets. Use additional contraceptive precautions for the following 7 days e.g. a barrier method such as a condom. If you have had sex during the days of missed tablets there is a possibility of pregnancy. So contact your doctor immediately.
If you have forgotten any of the pink tablets, and you have no bleeding during the week 13, you may be pregnant. Contact your doctor before you start the next pack.
If you vomit or have diarrhoea after taking Seasonique
If you vomit within 3-4 hours of taking a tablet or you have severe diarrhoea, there is a risk that the active substances in the pill are not fully absorbed into your body. The situation is similar to if you forget a tablet. After vomiting or diarrhoea, you must take another tablet as soon as possible. The advice given under "If you forget to take your tablets" should be followed.
If you don't want to change your normal tablet-taking pattern take the extra pink tablet from the last row in the pack.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much Seasonique.
Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
Symptoms of an overdose may include:
- feeling sick or vomiting
- dizziness
- feeling sleepy or tired
- women may also experience
- menstrual bleeding.
While you are taking Seasonique
Things you must do
Tell any other doctors, dentists and pharmacists who are treating you that you are taking Seasonique.
If you are about to start taking any new medicines, tell the doctor or pharmacist that you are taking Seasonique.
If you become pregnant while taking Seasonique, see your doctor immediately.
Use of Seasonique is generally not advisable when a woman is breast-feeding. If you want to take the pill while you are breast-feeding you should contact your doctor.
If you are about to have any blood tests, tell your doctor you are taking Seasonique.
Have regular check ups from your doctor, including a Pap smear. Oral contraceptives should not be prescribed for longer than one year without your doctor carrying out a check-up. Your doctor will advise you how often you need a Pap smear. A Pap smear can detect abnormal cells lining the cervix. Sometimes abnormal cells can progress to cervical cancer. The most important risk factor for cervical cancer is persistent human papillomavirus (HPV) infection. However, cervical cancer has been reported to occur more often in women using an oral contraceptive for a long time. This finding may not be caused by the oral contraceptive, but may be related to sexual behaviour and other reasons.
Perform regular breast self-examination. Risk factors for the development of breast cancer include increasing age, family history, obesity, never having had a baby, and late age for first full term pregnancy. Breast cancer has also been found slightly more often in women who use oral contraceptives than in women of the same age who do not use them. This slight increase in the number of breast cancer cases gradually disappears during the course of the 10 years after stopping use of oral contraceptives. It is not known whether the oral contraceptive causes the difference. It may be that the women were examined more often, so that the breast cancer was noticed earlier.
If you are concerned about contracting a sexually transmitted disease (STD), ask your partner to wear a condom when having sexual intercourse with you. Seasonique will not protect you from HIV-AIDS or any other sexually transmitted diseases (STDs) such as chlamydia, genital herpes, genital warts, gonorrhoea, hepatitis B, human papilloma virus and syphilis. To help protect yourself from STDs, you need to use a barrier contraceptive such as a condom.
Tell your doctor you are using Seasonique at least 4 weeks before any planned hospitalisation or surgery. Your doctor may tell you to stop taking Seasonique several weeks before surgery or at the time of immobilisation. Your doctor will tell you when you can start taking Seasonique after you are back on your feet.
To avoid pregnancy during this time you must use a non-hormonal method of contraception such as condoms or a diaphragm.
Bleeding between periods
When you take Seasonique, which has a 91-day extended dosing cycle, you should expect to have 4 scheduled periods per year (bleeding when you are taking the 7 white pills). Each period is likely to last about 3 days.
During the first few months that you are taking Seasonique, you may have unexpected bleeding. This bleeding or spotting tends to decrease with time. Do not stop taking Seasonique because of this bleeding or spotting. If the spotting continues for more than 7 consecutive days or if the bleeding is heavy, contact your doctor.
Things you must not do
Do not take Seasonique to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else even if they have the same condition as you.
Do not stop taking Seasonique without checking with your doctor. If you stop taking Seasonique or do not take a tablet every day, without using another form of contraception, you may become pregnant.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Seasonique.
All medicines can have side effects. Sometimes they are serious, but most of the time they are not. You may need medical treatment if you get some of the side effects.
It can be difficult to tell whether side effects are the result of taking Seasonique or are side effects of another medicine you are taking.
Do not be alarmed by the list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if....
Tell your doctor if you notice any of the following side effects and they worry you:
- changes in bleeding patterns, including breakthrough bleeding/spotting
- Painful periods
- missed periods, but if you have not taken Seasonique as directed you should check whether you are pregnant
- changes in mucus from the vagina
- changes in the cervix
- vaginal thrush (candida)
- breast pain, tenderness, enlargement, possible milk secretion
- changes in sex drive
- nausea or vomiting
- abdominal pain, cramps or bloating
- mood changes, including depression and/or worsening of existing depression
- headache, including migraines
- nervousness
- dizziness
- contact lenses becoming uncomfortable to wear
- weight change (increase or decrease)
- changes in appetite
- swelling of the hands, ankles or feet
- acne
- rash
- darkening of the skin, which may persist after stopping your medicine
- loss of scalp hair
- increase in body hair
The above list includes the more common side effects of your medicine.
Tell your doctor as soon as possible if....
Tell your doctor as soon as possible if you notice any worsening of conditions that you may already have such as:
- chorea (involuntary muscle spasm)
- porphyria
- systemic lupus erythematosus (Lupus)
- varicose veins
- gallbladder disease
- hereditary angioedema (swelling of the face, lips, mouth, tongue or throat).
The above list includes serious side effects that may require medical attention. Serious side effects are rare.
Go to hospital if....
Tell your doctor immediately, or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- sharp chest pain, coughing of blood, or sudden shortness of breath
- pain in the calf muscle area
- severe pain or swelling in one leg
- crushing chest pain or heaviness in the chest
- sudden severe headache or vomiting, dizziness or fainting, disturbances of vision or speech, weakness, or numbness in an arm or leg
- sudden changes or loss of vision
- breast lumps
- severe pain or tenderness in the stomach area
- jaundice or a yellowing of the skin or eyeballs, often with fever, fatigue, loss of appetite, dark coloured urine or light coloured bowel movements. Taking oral contraceptives has been associated with an increased risk of having a benign liver tumour and, in very rare cases, liver cancer. The risk appears to increase the longer oral contraceptives are taken
- migraine headaches for the first time
- more frequent migraines if you already suffer from them
- itchy rash
- you are an epileptic and your fits become more frequent
- rise in blood pressure. You may experience headache, blurred vision or palpitations. Sometimes your blood pressure may rise without you experiencing any of these symptoms. It is important to keep your routine doctor's appointments so that your blood pressure can be checked
- swelling around the eyes or mouth
- bloody diarrhoea, abdominal pain or tenderness, fever, nausea or vomiting.
Whilst these side effects are rare, they are serious. You may need urgent medical attention or hospitalisation.
Other side effects not listed above may also occur in some patients.
Tell your doctor if you notice anything else that is making you feel unwell, even if it is not on this list.
After taking Seasonique
Storage
Keep your tablets in the blister pack until it is time to take them. Once opened, the product should be stored in the original packaging inside the inner carton. If you take the tablets out of the blister pack they may not keep well.
Keep your tablets in a cool, dry place where the temperature stays below 30°C and is away from light. Do not store Seasonique or any other medicine, in a bathroom or near a sink. Do not leave Seasonique in the car on hot days or on window sills. Heat and dampness can destroy some medicines. Keep it where children cannot reach it. A locked cupboard at least one-and-a half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking Seasonique or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product Description
What it looks like
Seasonique pack contains 3 blisters in total: 2 blisters each holding 28 pink tablets and 1 blister holding 35 tablets in total- 28 pink tablets and 7 white tablets.
The pink tablets contain 150 micrograms levonorgestrel and 30 micrograms ethinyloestradiol. The white tablets contain 10 micrograms ethinyloestradiol.
The pink tablet is round, biconvex tablet, around 5.7 mm in diameter, embossed "172" on one side and "T" on the other side.
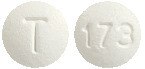
The white tablet is round, biconvex tablet, around 5.7 mm in diameter, embossed "173" on one side and "T" on the other side
Ingredients
Each pink film-coated tablet contains 150 micrograms of levonorgestrel and 30 micrograms ethinyloestradiol.
Each white tablet contains 10 micrograms ethinyloestradiol.
The pink tablets contain the following inactive ingredients:
- lactose anhydrous
- hypromellose
- microcrystalline cellulose
- magnesium stearate
- titanium dioxide (E171)
- Macrogol 400
- Polysorbate 80
The pink tablets contain the colouring agents:
- Allura Red AC (E129)
- Brilliant Blue FCF (E133)
The white tablets contain the following inactive ingredients:
- lactose anhydrous
- Polacrilin potassium
- microcrystalline cellulose
- magnesium stearate
- titanium dioxide (E171)
- Polydextrose
- hypromellose
- glycerol triacetate
- Macrogol 8000
Seasonique does not contain gluten or tartrazine.
Supplier
Seasonique is supplied in Australia by:
Theramex Australia Pty Ltd
Level 34, 60 Margaret Street,
Sydney NSW 2000
1800 THERAMEX or 1800 843 726
Australian Registration Number.
AUST R 238384
This leaflet was prepared in February 2019
® Registered Trade Mark
Published by MIMS May 2019


 It is important that women understand that VTE associated with COC use is rare in average-risk women. The risk in pregnancy (5-20 per 10,000 women over 9 months) and the risk in the postpartum period (45-65 per 10,000 women over 12 weeks) is higher than that as associated with COC use.
It is important that women understand that VTE associated with COC use is rare in average-risk women. The risk in pregnancy (5-20 per 10,000 women over 9 months) and the risk in the postpartum period (45-65 per 10,000 women over 12 weeks) is higher than that as associated with COC use. The adverse events associated with bleeding were consistently slightly higher for DP3-84/30 compared to Seasonique. Intermenstrual bleeding was reported in 12.1% of the DP3-84/30 patients compared to 11.5% of the DP3-84/10 patients and menorrhagia was reported in 7.7% of patients on DP3-84/30 compared to 5.8% on DP3-84/10. See Tables 3 and 4.
The adverse events associated with bleeding were consistently slightly higher for DP3-84/30 compared to Seasonique. Intermenstrual bleeding was reported in 12.1% of the DP3-84/30 patients compared to 11.5% of the DP3-84/10 patients and menorrhagia was reported in 7.7% of patients on DP3-84/30 compared to 5.8% on DP3-84/10. See Tables 3 and 4.
 The following serious adverse events have been reported in women using COCs, which are discussed (see Section 4.4 Special Warnings and Precautions for Use): venous thromboembolic disorders, arterial thromboembolic disorders, hypertension, liver tumours, depression.
The following serious adverse events have been reported in women using COCs, which are discussed (see Section 4.4 Special Warnings and Precautions for Use): venous thromboembolic disorders, arterial thromboembolic disorders, hypertension, liver tumours, depression. The decrease in the unscheduled bleeding/ spotting over treatment cycles was confirmed in the comparative PSE-302 study. After one year of treatment, the total number of days of bleeding/ spotting was similar for Seasonique and the 28 day comparator.
The decrease in the unscheduled bleeding/ spotting over treatment cycles was confirmed in the comparative PSE-302 study. After one year of treatment, the total number of days of bleeding/ spotting was similar for Seasonique and the 28 day comparator.
 Chemical name: (-)-13-Ethyl-17-hydroxy-18, 19-dinor-17 α-pregn-4-en-20-yn-3-one.
Chemical name: (-)-13-Ethyl-17-hydroxy-18, 19-dinor-17 α-pregn-4-en-20-yn-3-one. Chemical name: 19-Nor-17 α- pregna-1,3,5 (10)-trien-20-yne-3,17 diol.
Chemical name: 19-Nor-17 α- pregna-1,3,5 (10)-trien-20-yne-3,17 diol.