What is in this leaflet
This leaflet answers some common questions about Sensipar. It does not contain all the available information. It does not take the place of talking to your doctor, nurse or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Sensipar against the benefits he/she expects it will have for you.
If you have any concerns about taking Sensipar, ask your doctor, nurse or pharmacist.
Read this leaflet carefully before you start Sensipar and keep it with the medicine. You may need to read it again.
What Sensipar is used for
Sensipar is used to treat:
- a condition called secondary hyperparathyroidism (high-per-para-THIGH-royd-izm) in people with kidney disease who require dialysis treatment.
- a condition called primary hyperparathyroidism when surgical removal of the parathyroid gland is not a treatment option.
- high blood calcium levels in people with cancer of the parathyroid gland.
Secondary hyperparathyroidism
Kidney disease can cause a condition called secondary hyperparathyroidism, which can have a big impact on your health. Four small glands located behind the thyroid gland in your neck are called parathyroid glands. They make a hormone called parathyroid hormone (PTH). Normally, PTH makes sure you have just enough calcium and phosphorus in your blood to keep your bones, heart, muscles, nerves and blood vessels working well. When your kidneys are working properly, PTH keeps your calcium and phosphorus levels normal by moving the right amounts of calcium and phosphorus in and out of your bones.
When your kidneys aren't working properly, the calcium and phosphorus balance in your body is upset, and your parathyroid glands send out too much PTH to your body. This condition is called secondary hyperparathyroidism, and it can cause bone disease and also may be a risk factor for heart disease and abnormal calcium deposits in blood vessels and other parts of the body. Sensipar lowers PTH by telling your parathyroid glands to stop releasing too much PTH into your blood. It also lowers your calcium and phosphorus levels.
Primary hyperparathyroidism/Cancer of the parathyroid gland
An overactive parathyroid gland results in a condition called primary hyperparathyroidism, which can impact your health. Four small glands located behind the thyroid gland in your neck are called parathyroid glands. They make a hormone called parathyroid hormone (PTH). When your parathyroid glands are working normally, PTH keeps your calcium levels normal by moving the right amounts of calcium in and out of your bones.
Primary hyperparathyoidism is caused by an enlargement of one or more of the parathyroid glands occasionally due to cancer of the parathyroid gland. In primary hyperparathyroidism, your parathyroid glands send out too much PTH to your body and your blood level of calcium becomes high. Sensipar lowers PTH by telling your parathyroid glands to stop releasing too much PTH into your blood. It also lowers your blood calcium levels.
Your doctor may have prescribed Sensipar for another reason. Ask your doctor if you have any questions about why Sensipar has been prescribed for you.
Before you take Sensipar
When you must not take Sensipar
Do not take Sensipar if you are allergic to the active ingredient or any of the ingredients in Sensipar listed at the end of this leaflet.
Symptoms of an allergic reaction may include:
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- skin rash, itching or hives.
Talk to your doctor, nurse or pharmacist if you have any questions about this information.
Do not give Sensipar to a child. There is not enough information at present to recommend use of Sensipar in children.
Do not take Sensipar after the expiry date (Exp.) stamped on the pack. If you take this medicine after the expiry date has passed, it may not work as well.
Do not take Sensipar if the packaging is torn or shows signs of tampering or if the tablets do not look quite right.
Before you start to take Sensipar
Tell your doctor if:
- you have or have had any medical conditions, including:
- seizures (sometimes called fits or convulsions, see 'Side effects' section).
- heart failure (or a heart condition, see 'Side effects' section).
- intolerance to sugars (sometimes called lactose intolerance, see 'Ingredients' section).
- ulcers (stomach or intestinal), serious vomiting, inflammation of the stomach and swallowing tube.
- you are pregnant or intend to become pregnant.
Your doctor will discuss the risks and benefits of taking Sensipar if you are pregnant.
- you are breastfeeding or planning to breastfeed.
It is not known whether Sensipar passes into breast milk.
- you are taking any other medicines, including any medicines you buy without a prescription from a pharmacy, supermarket or health food shop (for example St John's Wort).
If you have not told your doctor about any of the above, tell him/her before you take Sensipar.
Taking other medicines
Tell your doctor if you are taking ketoconazole, erythromycin, itraconazole, rifampicin, phenytoin, amitriptyline, flecainide, vinblastine, thioridazine or medicines known as tricyclic antidepressants. Some of these medicines can affect how Sensipar works, while others are affected by Sensipar.
Driving and using machines
Dizziness and seizures have been reported by patients taking Sensipar. If you experience these side effects, do not drive or operate machines.
How to take Sensipar
Sensipar must be taken orally either with, or shortly after food. The tablets must be taken whole and are not to be divided.
Follow all directions given to you by your doctor, nurse and pharmacist carefully. They may differ from the information in this leaflet.
If you do not understand the instructions below, ask your doctor, nurse or pharmacist for help.
How much Sensipar to take
If you are being treated for secondary hyperparathyroidism
The usual starting dose for Sensipar is 30 mg (one tablet) once per day. Your doctor will take regular blood samples to measure how you are responding to Sensipar and will adjust your dose as necessary in order to control your parathyroid hormone, calcium and phosphate levels.
Once your condition is under control, your doctor will continue to regularly check your blood and your dose may be adjusted further in order to maintain long-term control of your parathyroid hormone, calcium and phosphate levels.
If you are being treated for primary hyperparathyroidism/ cancer of the parathyroid gland
The usual starting dose for Sensipar is 30 mg (one tablet) twice per day. Your doctor will take regular blood samples to measure how you are responding to Sensipar and will adjust your dose as necessary in order to control your calcium levels. Once your condition is under control, your doctor will continue to regularly check your blood and your dose may be adjusted further in order to maintain long-term control of your calcium levels.
If you forget to take Sensipar
If you have forgotten a dose of Sensipar, you should take your next dose as normal.
If you take more Sensipar than you should (overdose)
If you take more Sensipar than you should you must contact your doctor, nurse or pharmacist immediately.
While you are taking Sensipar
Things you must do
Always follow your doctor's instructions carefully. If you are about to start using a new medicine, tell your doctor, nurse and pharmacist that you are taking Sensipar.
If you become pregnant while you are taking Sensipar, tell your doctor.
Things you must not do
Do not take Sensipar to treat any other complaint unless your doctor says so.
Do not give Sensipar to anyone else, even if their symptoms seem similar to yours.
Side effects
Tell your doctor as soon as possible if you have any problems while taking Sensipar, even if you do not think the problems are connected with the medicine or are not listed in this leaflet.
Like other medicines, Sensipar may cause side effects. Some side effects may be serious and need medical attention. Other side effects are minor and are likely to be temporary.
Sensipar lowers your calcium level. If calcium levels become too low, you may have signs of low calcium. Signs of low calcium may include numbness or tingling around the mouth, muscle aches or cramps and seizures. If you have any of these symptoms, you should tell your doctor straight away. People with kidney disease not requiring dialysis are at increased risk of developing hypocalcaemia.
Ask your doctor, nurse or pharmacist to answer any questions you may have.
If any of the following happens, stop taking Sensipar and go straight to the hospital, as you may need urgent medical attention:
- Allergic reaction
- Skin rash over a large area of the body
- Swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- Shortness of breath
- Wheezing
- Faintness, rapid pulse or sweating.
Tell your doctor, nurse or pharmacist immediately if you notice any of the following:
- Nausea and vomiting.
People taking Sensipar have a greater chance of developing nausea and /or vomiting. If nausea or vomiting is making it difficult to take your medicines or is of any concern to you, you should tell your doctor.
- Seizure (also known as a fit or convulsion).
The risk of having seizures is greater in people who have had seizures before. Lowering the calcium level too much may also increase the risk of having a seizure. If you have a seizure you should tell your doctor straight away.
- Dizziness or light headedness, or worsening of a heart condition.
Sensipar may cause low blood pressure or affect the heart's function in people who have a heart condition (heart failure). If you know you have a heart condition, tell your doctor.
- Rash.
Pinkish, itchy swellings on the skin, also called hives or nettle rash. Itchy rash.
- Bleeding from the stomach or intestines.
Bleeding from the stomach or intestines may occur in some patients. You may experience severe pain or tenderness in the stomach, vomit blood or material that looks like coffee grounds, or have black or tar-like stools.
Tell your doctor, nurse or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some people.
After taking Sensipar
Storage
Keep your Sensipar in a cool place, under 30 degrees C.
The expiry date (Exp.) for Sensipar is stamped on the outer box and the blister label. Do not take Sensipar after this date, the last day of the month shown.
As with all medicines, you should keep Sensipar out of the reach and sight of children.
Product description
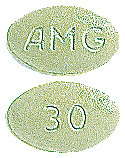
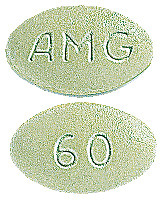
What it looks like
Sensipar is a light green film-coated tablet. They are oval-shaped and have "30", "60" or "90" marked on one side and "AMG" on the other side. Each tablet contains 30 mg, 60 mg or 90 mg of cinacalcet. They come in blister packs.
Ingredients
Active ingredient
The active ingredient in Sensipar is cinacalcet hydrochloride.
Other ingredients
The other ingredients of Sensipar are pre-gelatinised maize starch, microcrystalline cellulose, povidone, crospovidone, colloidal anhydrous silica, magnesium stearate and water.
The tablets are coated with: Carnauba wax,
Opadry green (containing lactose monohydrate, hypromellose, titanium dioxide (E171), glycerol triacetate, FD&C Blue (E132), iron oxide yellow (E172)) and Opadry clear (containing hypromellose, macrogol).
If you have been told by your doctor that you have an intolerance to certain sugars (for example, lactose), tell your doctor before taking Sensipar.
Sponsor
Sensipar is supplied in Australia by:
Amgen Australia Pty Ltd
Level 7, 123 Epping Road
North Ryde
NSW 2113
ABN 31 051 057 428
Australian Registration Numbers
Sensipar 30 mg in a blister pack AUST R 98399
Sensipar 60 mg in a blister pack AUST R 98404
Sensipar 90 mg in a blister pack AUST R 98407
(R) Registered Trademark
This leaflet was prepared in February 2020.
Published by MIMS April 2020


 The incidence of serious adverse events (29% vs 31%) and deaths (2% vs 3%) was similar in the cinacalcet and placebo groups, respectively.
The incidence of serious adverse events (29% vs 31%) and deaths (2% vs 3%) was similar in the cinacalcet and placebo groups, respectively. Mean iPTH and Ca x P by treatment group for the overall study population during the 6-month treatment period are presented in Figure 1 and Figure 2.
Mean iPTH and Ca x P by treatment group for the overall study population during the 6-month treatment period are presented in Figure 1 and Figure 2.
 In patients receiving cinacalcet, reductions in iPTH and Ca x P occurred within 2 weeks and were maintained for at least 12 months of treatment (n = 99 on cinacalcet, 111 on placebo).
In patients receiving cinacalcet, reductions in iPTH and Ca x P occurred within 2 weeks and were maintained for at least 12 months of treatment (n = 99 on cinacalcet, 111 on placebo).
 Whilst a 15 mg dose of cinacalcet was used in the paediatric PK study, this dose strength is not registered.
Whilst a 15 mg dose of cinacalcet was used in the paediatric PK study, this dose strength is not registered. The empirical formula of cinacalcet hydrochloride is C22H22F3N.HCl and it has a molecular weight of 393.9 g/mol (hydrochloride salt) and 357.4 g/mol (free base). It has one chiral centre having an R-absolute configuration. The R-enantiomer is the more potent enantiomer and has been shown to be responsible for pharmacodynamic activity.
The empirical formula of cinacalcet hydrochloride is C22H22F3N.HCl and it has a molecular weight of 393.9 g/mol (hydrochloride salt) and 357.4 g/mol (free base). It has one chiral centre having an R-absolute configuration. The R-enantiomer is the more potent enantiomer and has been shown to be responsible for pharmacodynamic activity.