What is in this leaflet
This leaflet is designed to provide answers to some common questions about this medicine. It does not contain all the available information.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Solian against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with this medicine. You may need to read it again.
What Solian is used for
The name of your medicine is Solian. It contains the active ingredient called amisulpride.
Solian belongs to a group of medicines called antipsychotics. Solian is used to treat symptoms of schizophrenia.
Schizophrenia is a condition which affects the way you think, feel and/or act. Schizophrenia may cause symptoms such as hallucinations (e.g. hearing, seeing or sensing things which are not there), delusions, unusual suspiciousness, emotional and social withdrawal. People with schizophrenia may also feel depressed, anxious or tense.
Your doctor may have prescribed Solian for another reason.
Ask your doctor if you have any questions about why Solian has been prescribed for you.
Before taking it
When you must not take it
Do not take Solian if:
- you have an ALLERGIC REACTION to Solian or any of the ingredients listed at the end of this leaflet.
Signs of an allergic reaction may include a skin rash, itching, shortness of breath or swelling of the face, lips or tongue. - you are breastfeeding or plan to breastfeed.
- you are taking the following medicines
- medicines used to treat irregular heart rhythm such as quinidine, disopyramide, amiodarone and sotalol
- cisapride
- antibiotics such as erythromycin and pentamidine, given as an injection into the veins
- levodopa, a medicine used in Parkinson's disease
- thioridazone, an antipsychotic
- methadone, medicine used to treat pain or addiction - the packaging is torn or shows signs of tampering or the tablets do not look quite right.
- the expiry date on the pack has passed.
Do not take Solian if you have or have had any of the following medical conditions:
- phaeochromocytoma, a rare tumour of the adrenal glands which sit near the kidneys
- tumour of the pituitary gland, a small gland at the base of the brain
- breast cancer
- liver disease
Solian must not be taken by children up to the age of puberty. There is limited information on the use of Solian in adolescents and its use is not recommended from puberty to the age of 18 years. If you are not yet 18 years of age, ask your doctor if Solian is right for you.
Before you start to take it
Your doctor must know about all the following before you start to take Solian.
Tell your doctor if:
- you have had an allergic reaction to any medicine which you have taken previously to treat your current condition.
- you are pregnant, think you may be pregnant or intend to become pregnant. Solian is not recommended for use in pregnancy. If you need to take Solian during pregnancy you should discuss the benefits and risks of taking it with your doctor. Newborns of mothers who have taken Solian during pregnancy need to be carefully monitored.
- you suffer from lactose intolerance because Solian tablets contain lactose.
- you have kidney or liver disease, Parkinson's disease or fits (seizures).
- you have problems with the heart and blood vessels.
- you have, or have a history of blood clots.
- you have hyperglycaemia (high sugar levels in the blood) or a family history of diabetes. Your doctor may recommend monitoring your blood sugar levels while you are taking Solian.
- you suffer from dementia.
- you have mental/mood changes or suicidal thoughts. Patients (and caregivers of patients) need to monitor for any worsening of their condition and/or the development of thoughts of suicide, suicidal behaviour or thoughts of harming themselves. Seek medical advice immediately if these symptoms present.
- you have risk factors for stroke.
- you have a history, or family history, of breast cancer
- you have a history of sleep apnoea
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food store.
Some medicines and Solian may interfere with each other. These include:
- medicines used to treat irregular heart rhythm such as quinidine, disopyramide, amiodarone and sotalol
- other medicines used to treat heart problems such as diltiazem, verapamil, clonidine, digoxin and drugs known as beta blockers (e.g. propranolol)
- intravenous amphotericin B (amphotericin), an anti-fungal given by injection into the veins
- other antipsychotics such as thioridazine, clozapine, chlorpromazine, trifluperazine, pimozide, haloperidol, imipramine and lithium
- diuretics
- stimulant laxatives
- glucocorticosteroids
- diagnostics drugs such as tetracosactides
- medicines taken for anxiety or to help you sleep (central nervous system depressants)
- anaesthetics (a medicine used during surgery)
- medicines taken for depression
- some strong pain killers
- antihistamines, medicines to treat allergies, which cause drowsiness
- some medicines taken to control blood pressure
If you are unsure about any medicine you are taking, you should check with your doctor or pharmacist. They will have more information on medicines to be careful of while you are taking Solian.
How to take it
How much to take
Your doctor will tell you how many Solian tablets you should take, or the amount of Solian Solution you should take. The dosage is adjusted for each individual and can range from 50mg a day up to 800mg a day. In some cases your doctor may increase the dose to 1200mg a day.
When taking Solian Solution, the dosage syringe supplied should be used to measure the correct dose. Each 1mL marking is equal to 100mg.
After introducing the measuring syringe into the bottle, draw the plunger of the measuring syringe up to the graduation mark corresponding to the number of milligrams to be administered.
Solian tablets and Solian Solution should be taken once or twice a day as advised by your doctor. Your doctor may increase or decrease your dose depending on your condition.
Do not take more than the dose your doctor has recommended.
How to take it
Solian tablets should be swallowed whole with a glass of water.
Solian Solution is swallowed. It may be mixed with water if preferred.
When to take it
Solian tablets and Solian Solution should preferably be taken before meals. Take your prescribed dose at about the same time each day.
How long do I take it
It is important that you do NOT stop taking Solian unless your doctor tells you. Do not stop taking your Solian just because you feel better. It is very important to continue Solian because it will help you stay well.
If you forget to take it
If you forget to take your medicine, take your dose as soon as you remember. Do not take a double dose to make up for the dose that you missed.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 POISON or 0800 764766), or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much Solian. Show the doctor your pack of tablets or bottle. Do this even if there are no signs of discomfort or poisoning.
If you have taken too much Solian, the most common signs are drowsiness and slurred speech.
While you are using it
Things you must do
It is very important to continue taking Solian because it will help you stay well.
Tell all doctors, dentists and pharmacists who are treating you that you are taking Solian.
While you are taking Solian, tell your doctor or pharmacist before you start any new medicine.
Tell your doctor immediately, or go to the nearest hospital, if you have any of the following suicidal thoughts or mental/mood changes:
- thoughts or talk of death or suicide
- thoughts or talk of self-harm or harm to others
- any recent attempts of self-harm
- increase in aggressive behaviour, irritability or agitation
- depressed mood or worsening of depression
Occasionally, the symptoms of depression may include thoughts of suicide or self-harm. These symptoms may continue to get worse during the early stages of treatment until the effect of the medicine becomes apparent. All mentions of suicide or violence must be taken seriously.
Things to be careful of
Solian may cause drowsiness in some people.
Be careful driving or operating machinery until you know how Solian affects you.
Be careful if you are elderly or unwell.
Some people may experience side effects such as drowsiness, confusion, dizziness and unsteadiness. Solian may affect your ability to move or balance. This may increase the risk of a fall, sometimes leading to fractures.
The effects of alcohol could be made worse while taking Solian. It is NOT recommended that you drink alcohol while taking Solian.
Be careful while taking antihistamines, sleeping tablets or tablets to relieve pain while taking this medicine. Solian can increase drowsiness caused by medicines affecting your nervous system.
Things you must NOT do
Do not drive or operate machinery until you know how Solian affects you.
Do not give Solian to anyone else. Your doctor has prescribed it for you and your condition.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Solian.
Like other medicines, Solian can cause some side effects. If they occur, most are likely to be minor and temporary. However, some may be serious and may need medical attention. Some of the side effects are dose related, so it is important that you never exceed your prescribed dose.
While you are taking Solian
Tell your doctor if you notice any of the following and they worry you:
- drowsiness
- weight gain
- dizziness
- increased appetite
- nausea
- vomiting
- constipation
- dry mouth
- blurred vision
- insomnia
- anxiety
- agitation
- problems with orgasm
These are the most common side effects of Solian.
Rare side effects include sleep walking and sleep eating.
Some people may feel dizzy in the early stages of treatment, especially when getting up from a lying or sitting position. This side effect usually passes after taking Solian for a few days.
Sometimes trembling, noticeable muscle stiffness or spasm, slowness of movement, excess saliva, restlessness, an overwhelming urge to move and either distress or movements such as pacing, swinging of the legs while seated, rocking from foot to foot, or both can occur. This will usually be reduced if your dose of Solian is lowered by your doctor or if your doctor prescribes you an additional medicine.
High blood sugar has been reported in patients taking Solian. Symptoms of high sugar levels in the blood include passing more urine than normal, persistent excessive thirst, increased appetite with a loss in weight and weakness.
Some people experience increased sensitivity to the sun or notice symptoms of sunburn (such as redness, itching, swelling, blistering) which may occur more quickly than normal.
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- muscle symptoms including pain, weakness, twitching or stiffness
- abnormal movements mainly of the face or tongue
- fever
- unexplained infections
- faster breathing
- sweating
- yellowing of the skin and eyes, also called jaundice
- light coloured bowel motions
- dark coloured urine
If this occurs, stop taking Solian immediately and contact your doctor.
After prolonged use in women, medicines of this type can cause:
- breast pain
- milk secretion
- an absence of their monthly period
- changes in the regularity of their periods
Tell your doctor if your monthly periods are absent for six months or more.
After prolonged use in men, medicines of this type can cause breast enlargement or impotence.
Incidences of abnormal liver function have been occasionally reported.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Tell your doctor if you notice any symptoms that worry you, even if you think the problems are not connected with the medicine or are not listed in this leaflet.
After taking it
Storage
Keep your tablets in the blister pack until it is time to take them. If you take the tablets out of the blister pack they may not keep well.
Store Solian Solution in the original bottle. Solian Solution has an expiry of two months once opened. Any solution remaining after this should be discarded.
Keep Solian tablets in a cool, dry place where the temperature stays below 30°C.
Solian Solution should be stored in a cool, dry place where the temperature stays below 25°C.
Do not store Solian or any other medicine in the bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
There will be an expiry date (month, year) on your Solian container. The medicine should not be taken after this date.
Disposal
If your doctor tells you to stop taking Solian or the tablets or Solution have passed their expiry date, ask your pharmacist what to do with the amount left over.
Product description
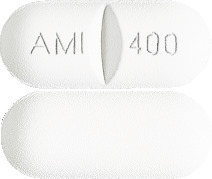
What it looks like
Solian tablets are available in three different strengths:
The 100 mg strength is a white, flat faced, breakable tablet, marked "AMI 100".
The 200 mg strength is a white, flat faced, breakable tablet, marked "AMI 200".
The 400 mg strength is a white, film-coated, breakable, oblong tablet, marked "AMI 400".
The 100 mg strength is available in a pack size of 30 tablets.
The 200 mg strength is available in a pack size of 60 tablets.
The 400 mg strength is available in a pack size of 60 tablets.
Solian Solution is a clear yellow coloured liquid. It is available in 60mL brown glass bottles.
Ingredients
Active Ingredient:
Solian 100 tablets - 100 mg amisulpride per tablet.
Solian 200 tablets - 200 mg amisulpride per tablet.
Solian 400 tablets - 400 mg amisulpride per tablet.
Solian Solution - 100mg amisulpride per mL.
Inactive Ingredients:
The tablets also contain:
- sodium starch glycollate type A
- lactose monohydrate
- microcrystalline cellulose
- hypromellose
- magnesium stearate
The 400 mg tablets also contain:
- PEG-40 stearate
- titanium dioxide
The oral liquid also contains:
- Gesweet® 2023
- Hydrochloric acid
- Methyl hydroxybenzoate
- Propyl hydroxybenzoate
- Potassium sorbate
- Caramel Flavour® E_9422058
- Purified water
Manufacturer
Solian is distributed in Australia by:
sanofi-aventis australia pty ltd
12-24 Talavera Road
Macquarie Park NSW 2113
Australia
Freecall No: 1800 818 806
Solian is distributed in New Zealand by:
sanofi-aventis new zealand limited
56 Cawley Street
Ellerslie, Auckland 1051
New Zealand
Freecall No: 0800 283 684
The Australian Registration numbers for Solian are as follows:
Solian 100*: AUST R 96422
Solian 200*: AUST R 96425
Solian 400*: AUST R 74272
Solian Solution 100mg/mL: AUST R 94484
*Not marketed in New Zealand
This leaflet was prepared in November 2021
solian-ccdsv15-cmiv19-25feb22
Published by MIMS April 2022



 The following CIOMS frequency rating is used, when applicable: very common ≥ 10%; common ≥ 1 and < 10%; uncommon ≥ 0.1 and < 1%; rare ≥ 0.01 and < 0.1%; very rare < 0.01%; not known (cannot be estimated from available data).
The following CIOMS frequency rating is used, when applicable: very common ≥ 10%; common ≥ 1 and < 10%; uncommon ≥ 0.1 and < 1%; rare ≥ 0.01 and < 0.1%; very rare < 0.01%; not known (cannot be estimated from available data).
