What is in this leaflet
This leaflet answers some common questions about Somac.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available. You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on this medicine.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Somac against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Somac is used for
Ulcers
Somac is used to treat and help heal duodenal and gastric ulcers.
Depending on the position of the ulcer it is called a gastric or duodenal ulcer. A gastric ulcer occurs in the stomach. A duodenal ulcer occurs in the duodenum which is the tube leading out of the stomach.
These can be caused in part by too much acid being made in the stomach.
Most people who have a peptic ulcer also have bacteria called Helicobacter pylori in their stomach. When Somac is taken with antibiotics the combination therapy will kill the Helicobacter pylori and let your ulcer heal.
Somac may also be used to prevent ulcers associated with the use of non-steroidal anti-inflammatory drugs (NSAIDs). These are medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis (inflammation of the joints).
Reflux disease
Somac is also used to treat reflux oesophagitis or reflux disease. This can be caused by “washing back” (reflux) of food and acid from the stomach into the food pipe, also known as the oesophagus.
Reflux can cause a burning sensation in the chest rising up to the throat, also known as heartburn.
Somac is also used to prevent reflux oesophagitis from coming back.
Zollinger-Ellison syndrome
Somac is also used to treat a rare condition called Zollinger-Ellison syndrome, where the stomach produces very large amounts of acid, much more than in ulcers and reflux disease.
This medicine belongs to a group of medicines called proton pump inhibitors (PPIs).
This medicine works by decreasing the amount of acid the stomach makes, to give relief from the symptoms and allow healing to take place.
Ask your doctor if you have any questions about why it has been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is not addictive. This medicine is available only with a doctor’s prescription.
This medicine is not expected to affect your ability to drive a car or operate machinery.
However, do not drive a car or operate machines if you experience side effects such as dizziness or blurred vision.
Somac should not be given to children under 5 years of age. There is not enough information to recommend the use of this medicine for children under the age of 5 years.
Before you take Somac
When you must not take it
Do not take Somac if you have an allergy to:
- any medicine containing pantoprazole
- any of the ingredients listed at the end of this leaflet
Some symptoms of an allergic reaction include skin rash, itching, shortness of breath or swelling of the face, lips or tongue, which may cause difficulty in swallowing or breathing.
Do not take this medicine if you have severe liver disease or cirrhosis.
Do not take Somac in combination with antibiotics or any other medicine if:
- you are allergic to any of the antibiotics or medicines your doctor may prescribe with Somac
- you have moderate to severe liver or kidney disease
Do not take Somac in combination with atazanavir or nelfinavir (anti-viral medications). Do not take it after the expiry date printed on the pack or if the packaging is damaged or shows signs of tampering. If it has expired or is damaged return it to your pharmacist for disposal.
Before you start to take it
Tell your doctor or pharmacist if you have any allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any other medical conditions.
Tell your doctor if you are pregnant, intend to become pregnant, or are breast-feeding. Your doctor can discuss the risks and benefits involved. If you have not told your doctor about any of the above, tell them before you take Somac.
Tell your doctor if you have any of the following symptoms:
- unintentional weight loss
- repeated vomiting
- vomiting blood
- difficulty or pain when swallowing
- you look pale and feel weak
- you notice blood in your stools
Your doctor may need to perform some additional tests before you take Somac.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Somac may interfere with each other. These include:
- warfarin, phenprocoumon - medicines used to prevent blood clots (anticoagulants)
- atazanavir, nelfinavir – medicines used to treat viral infections such as HIV
- ketoconazole, itraconazole, posaconazole - medicines used to treat fungal infection
- methotrexate - a medicine used to treat arthritis and some types of cancer
- erlotinib or related medicines used to treat cancer
- tacrolimus, mycophenolate mofetil – medicines used to suppress the immune system
- fluvoxamine - a medicine used to treat anxiety and depression
These medicines may be affected by Somac, or may affect how well it works. You may need to use different amounts of your medicine, or take different medicines.
Your doctor or pharmacist has more information on medicines to be careful with or to avoid while taking Somac.
How to take Somac
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box/bottle, ask your doctor or pharmacist for help.
How much to take
The usual dose is 40 mg per day.
However, if your doctor also prescribes antibiotics in combination with Somac for the treatment of duodenal ulcers, the dose of Somac is 80 mg per day. The first 40 mg dose should be taken in the morning and the second should be taken before the evening meal for 7 days.
Your doctor will prescribe the dose that is right for you.
In children over 5 years of age, the dose of Somac for reflux oesophagitis or reflux disease is based on weight and may be 20 mg or 40 mg, depending on the condition being treated. Somac should not be taken for longer than 8 weeks.
The dose and frequency of Somac that your doctor prescribes for you depends on your medical condition.
Your doctor may change the dose as your condition changes.
How to take it
Swallow your tablets whole with a little water with or without food.
If you are using Somac granules, take it half an hour before a meal without chewing or crushing the granules. Take the granules in apple juice, orange juice or water as follows:
- open sachet
- sprinkle intact granules into a small volume of apple juice, pulp-free orange juice, or water (at least 15 mL). Alternatively, a tablespoon may be used
- mix briefly just before drinking
- drink straight away
- to ensure that you have taken all the medicine, rinse the container thoroughly once or twice with apple juice, orange juice or water to remove any remaining granules and drink immediately
You can also take the granules in applesauce as follows:
- open sachet
- sprinkle intact granules on a teaspoon of applesauce.
- swallow within 10 minutes of preparation
Somac granules are intended for people who have difficulty swallowing tablets including those who require a nasogastric tube.
When to take it
Take Somac at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
If you are taking other medicines, like antibiotics, in combination with Somac therapy, follow the instructions for the use of each medicine carefully.
Do not crush or chew the tablets or granules. Somac tablets and granules have a special coating to protect them from the acidic contents of your stomach. For Somac to work effectively, this coating must not be broken.
How long to take it
Continue taking your medicine for as long as your doctor or pharmacist tells you.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking it as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for hints.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 764 766), or go to Accident and Emergency at your nearest hospital, if you or anyone else may have taken too much Somac. Do this even if there are no signs of discomfort or poisoning. Urgent medical attention may be needed.
While you are taking Somac
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking Somac.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon that you are taking this medicine.
If you become pregnant while you are taking this medicine, tell your doctor or pharmacist immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Keep all of your doctor’s appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Tell your doctor if your reflux symptoms return after you stop taking this medicine. The symptoms of reflux may return after stopping this medicine suddenly, especially if you have taken it for a while.
Things you must not do
Do not use this medicine to treat any other complaints unless your doctor tells you to.
Do not give this medicine to anyone else, even if they have the same symptoms as you.
Things that may help your condition
Some self help measures suggested below may help your condition. Your doctor or pharmacist can give you more information about these measures.
- Alcohol –
your doctor may advise you to limit your alcohol intake. - Aspirin and many other medicines used to treat arthritis, period pain, headaches –
these medicines may irritate the stomach and may make your condition worse. Your doctor or pharmacist may suggest other medicines you can take. - Caffeine –
your doctor may advise you to limit the number of drinks which contain caffeine, such as coffee, tea, cocoa and cola drinks, because they contain ingredients that may irritate your stomach. - Eating habits –
eat smaller, more frequent meals. Eat slowly and chew your food carefully. Try not to rush at meal times. - Smoking –
your doctor may advise you to stop smoking or at least cut down. - Weight –
your doctor may suggest losing some weight to help your condition.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Somac. It helps most people peptic ulcers or reflux disease, but it may have unwanted side effects in a few people.
All medicines have some unwanted side effects. Sometimes they are serious, but most of the time they are not. You may need medical attention if you get some of the side-effects.
Ask your doctor or pharmacist any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- headache
- dizziness
- diarrhoea
- nausea or vomiting
- stomach pain
- excessive gas in the stomach or bowel
- indigestion
- constipation
- dry mouth
- metallic taste
- weakness or tiredness
- increased sweating or body temperature
- blurred vision
- skin problems such as itchiness and rash
- trouble sleeping
These are the more common side effects of Somac.
Tell your doctor immediately if you notice any of the following:
- unusual tiredness or weakness
- nausea, vomiting, loss of appetite, feeling generally unwell, fever, itching, yellowing of the skin and eyes, and dark coloured urine
- blood in the urine
- increased or decreased need to urinate
- severe skin problems such as itchiness, redness, rash with swelling, blistering or peeling of the skin or rash when exposed to the sun, possibly with pain in the joints and general fever
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- chest pain
- shortness of breath
- high blood pressure
- water retention, swelling
- bleeding or bruising more easily than normal
- depression, confusion or anxiety
- bone fracture of the hip, wrist or spine (mainly a risk in people who take high doses of PPIs or use them long term (a year or longer))
- symptoms such as seizures, abnormal or fast heartbeat, jerking/shaking movements or muscle cramps. These can be a sign of low magnesium, calcium or potassium levels in your blood
- severe and/or persistent diarrhoea, because this medicine has been associated with a small increase in infectious diarrhoea
The above list includes serious side effects that may require medical attention. Serious side effects are rare.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some people.
Ask your doctor or pharmacist if you do not understand anything in this list.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking Somac
Storage
Keep your tablets in their blister or bottle, and granules in their sachet pack until it is time to take them. If you take the tablets or granules out of the blister, bottle or sachet pack they may not keep well.
Keep the medicine in a cool dry place where the temperature stays below 25°C (granules) or 30°C (tablets).
Do not store it or any other medicines in the bathroom, near a sink or windowsill. Do not leave it in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres (5 feet) above the ground, is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or if the medicines have passed their expiry date, ask your pharmacist what to do with any tablets or granules that are left over.
Product description
What it looks like
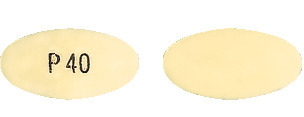
Somac comes in 20 mg and 40 mg tablets, and 40 mg granules.
Somac 20 mg tablets - yellow and oval shaped, marked with ‘P20’ on one side.
Somac 40 mg tablets - yellow and oval shaped, marked with ‘P40’ on one side.
Somac 40 mg granules – pale yellowish to dark brownish in colour.
Somac 40 mg tablets are available in blister packs of 5 and 30 tablets and bottle packs of 30 tablets.
Somac 20 mg tablets are available in blister packs of 30 tablets.
Somac 40 mg granules are available in single aluminium foil sachets in packs of 5 and 30 sachets.
Ingredients
Tablets
Somac 40 mg tablets contain the equivalent of 40 mg pantoprazole and Somac 20 mg tablets contain the equivalent of 20 mg pantoprazole. Somac tablets also contain:
- sodium carbonate anhydrous
- mannitol
- crospovidone
- povidone
- calcium stearate
- hypromellose
- titanium dioxide
- iron oxide yellow
- propylene glycol
- methacrylic acid copolymer
- polysorbate 80
- sodium lauryl sulfate
- triethyl citrate
- opacode brown S-1-16530 printing ink
Granules
Somac 40 mg granules contain the equivalent of 40 mg pantoprazole.
Somac granules also contain:
- microcrystalline cellulose
- sodium carbonate anhydrous
- crospovidone
- hypromellose
- polysorbate 80
- povidone
- titanium dioxide
- iron oxide yellow
- EUDRAGIT L30D-55
- triethyl citrate
- purified talc
Somac tablets and granules do not contain gluten, lactose, sucrose, tartrazine or other azo dyes.
Supplier
Somac tablets and granules are supplied in Australia by:
Takeda Pharmaceuticals Australia Pty Ltd
Level 39
225 George Street
Sydney NSW 2000
Australia
Telephone: 1800 012 612
www.takeda.com/en-au
The Australian Registration Number(s) are as follows:
Somac tablets (blister packs)
40 mg - AUST R 69792
20 mg - AUST R 70829
Somac tablets (bottle packs)
40 mg - AUST R 69791
Somac granules
40 mg - AUST R 148005
SOMAC® is a registered trademark of Takeda GmbH
This leaflet was prepared in August 2022
Published by MIMS September 2022



 The following safety data for patients aged 2 to 16 years (n = 250) is collated from 5 clinical studies (3001A1-109-US, 3001K1-110-US, 3001A1-322-US, 3001A1-326-US and BYK1023/MEX008). See Table 3.
The following safety data for patients aged 2 to 16 years (n = 250) is collated from 5 clinical studies (3001A1-109-US, 3001K1-110-US, 3001A1-322-US, 3001A1-326-US and BYK1023/MEX008). See Table 3.




 Pantoprazole 20 mg and 40 mg/day doses were therapeutically equivalent based on the pre-defined equivalence criterion of the 90% confidence interval of the difference between doses being within ± 20%.
Pantoprazole 20 mg and 40 mg/day doses were therapeutically equivalent based on the pre-defined equivalence criterion of the 90% confidence interval of the difference between doses being within ± 20%. Pantoprazole 20 mg once daily was statistically significantly superior to misoprostol 200 microgram twice daily with regard to "therapeutic failure" and to "endoscopic failure". Reflux oesophagitis was included as an efficacy end-point in the study which may have biased the results in favour of pantoprazole. A causal association between NSAIDs and reflux oesophagitis has not been established. In addition, proton pump inhibitors such as pantoprazole have documented beneficial treatment effects on reflux oesophagitis while misoprostol (a prostaglandin E1 analogue) has negligible therapeutic effects.
Pantoprazole 20 mg once daily was statistically significantly superior to misoprostol 200 microgram twice daily with regard to "therapeutic failure" and to "endoscopic failure". Reflux oesophagitis was included as an efficacy end-point in the study which may have biased the results in favour of pantoprazole. A causal association between NSAIDs and reflux oesophagitis has not been established. In addition, proton pump inhibitors such as pantoprazole have documented beneficial treatment effects on reflux oesophagitis while misoprostol (a prostaglandin E1 analogue) has negligible therapeutic effects. All three treatments, 20 mg pantoprazole, 40 mg pantoprazole and 20 mg omeprazole, were proven to be of equivalent and high efficacy.
All three treatments, 20 mg pantoprazole, 40 mg pantoprazole and 20 mg omeprazole, were proven to be of equivalent and high efficacy.
