What is in this leaflet
This leaflet answers some common questions about TACIDINE. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking TACIDINE against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What TACIDINE is used for
TACIDINE contains the active ingredient nizatidine.
Nizatidine belongs to a group of medicines called histamine (H2) antagonist or histamine (H2) blockers. These medicines work by reducing the amount of stomach acid produced which in turn reduces the pain and allows the ulcers and/or reflux disease to heal in most people.
Ulcers
TACIDINE is used to treat both gastric ulcers and duodenal ulcers. A gastric ulcer occurs in the stomach. A duodenal ulcer occurs in the duodenum (which is part of your small intestine). The ulcers can be caused in part by too much acid being made in the stomach.
TACIDINE is also used to help stop duodenal ulcers from coming back.
Reflux Disease
TACIDINE is also used to treat reflux oesophagitis or reflux disease. This is caused by "washing back" (reflux) of food and acid from the stomach into the food pipe (also known as the oesophagus).
Reflux causes burning sensation in the chest rising up to the throat (heartburn) and most often occurs after eating or at night.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
TACIDINE is not recommended for use in children, as the safety and effectiveness have not been established.
This medicine is not addictive.
This medicine is available only with a doctor's prescription.
Before you take TACIDINE
When you must not take it
Do not take TACIDINE if you have an allergy to:
- any medicine containing nizatidine
- any other histamine (H2) blocking medicine (e.g. cimetidine, ranitidine, famotidine)
- any of the ingredients listed at the end of this leaflet
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If you take this medicine after the expiry date has passed, it may not work as well.
If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- kidney disease
- liver disease
- chronic lung disease
- diabetes
- a weakened immune system or lowered resistance to infection, sometimes caused by certain diseases or treatments
Tell your doctor if you are pregnant or plan to become pregnant or are breastfeeding or plan to breast feed. Your doctor can discuss with you the risks and benefits involved.
The active ingredient in TACIDINE passes into breast milk and there is a possibility that your baby may be affected.
Tell your doctor if you plan to have surgery.
If you have not told your doctor about any of the above, tell them before you start taking TACIDINE.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and TACIDINE may interfere with each other. These include:
- aspirin
- certain antacids used to treat heartburn and indigestion such as Mylanta and Gelusil
These medicines may be affected by TACIDINE or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take TACIDINE
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
How much to take
The dose varies from person to person:
- duodenal and stomach ulcers - the recommended dosage is 150 mg twice a day or 300 mg once in the evening
- to stop duodenal ulcers from coming back - the usual dosage is 150 mg once daily
- reflux disease - the recommended dosage is 150 mg twice daily
Elderly people and those who have kidney problems may need to take a lower dose.
How to take it
Swallow the capsules whole with a full glass of water.
When to take it
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
TACIDINE can be taken with or without food.
The 150 mg capsule is usually taken twice a day - one capsule in the morning and one capsule in the evening before you go to bed.
The 300 mg capsule is usually taken once a day at bedtime.
How long to take it
Continue taking your medicine for as long as your doctor tells you.
This medicine helps to control your condition but does not cure it. It is important to keep taking your medicine even if you feel well.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much TACIDINE. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking TACIDINE
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking TACIDINE.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, including dental surgery, tell the surgeon, anaesthetist or dentist that you are taking this medicine. It may affect other medicines used during surgery.
If you are taking it for an ulcer, you should go to your doctor regularly for checkups to make sure that TACIDINE has healed your ulcer.
If you become pregnant while taking this medicine, tell your doctor immediately.
Keep all of your doctor's appointments so that your progress can be checked.
Things you must not do
Do not take TACIDINE to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor. If you stop taking your medicine too soon then your condition may not have been properly treated.
Things to be careful of
Be careful driving or operating machinery until you know how TACIDINE affects you. This medicine may cause dizziness or light-headedness in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Things that would be helpful for your condition
Some self-help measures suggested below may help your condition. Talk to your doctor or pharmacist about these measures and for more information.
- alcohol - your doctor may advise you to limit your alcohol intake
- aspirin and other medicines used to treat arthritis/period pain/headaches - these medicines may irritate the stomach and may make your condition worse. Your doctor or pharmacist may suggest other medicines you can take
- caffeine - your doctor may advise you to limit the number of drinks which contain caffeine, such as coffee, tea, cocoa and cola drinks, as the caffeine may irritate your stomach
- eating habits - eat smaller, more frequent meals. Eat slowly and chew your food carefully. Try not to rush at meal times
- smoking - your doctor may advise you to stop smoking or at least cut down
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking TACIDINE.
This medicine helps most people with ulcers or reflux disease, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- sweating
- itchy skin rash or hives
- headaches, being short of breath when exercising,
- flatulence, vomiting, diarrhoea, constipation
- impotence
The above list includes the more common side effects of your medicine. They are usually mild and short-lived.
Incidences of abnormal liver function, accompanied by jaundice (yellow skin) have been rarely reported by patients taking this medicine. This side effect has been reversed when TACIDINE is stopped.
Prolonged use of TACIDINE may impair the absorption of Vitamin B12.
Tell your doctor immediately if you notice any of the following:
- yellowing of the whites of the eyes or skin, also called jaundice
- dark urine
- symptoms of anaemia, which may include tiredness, dizziness and looking pale
- confusion
The above list includes serious side effects that may require medical attention.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at the nearest hospital:
- vomiting blood or food
- passing black (blood-stained) bowel motions
- symptoms of a severe allergic reaction which may include skin rash, itching or hives; swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing; wheezing or shortness of breath
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After taking TACIDINE
Storage
Keep your capsules in the pack until it is time to take them. If you take the capsules out of the pack they may not keep well.
Keep your capsules in a cool dry place where the temperature stays below 25°C.
Do not store TACIDINE or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine, or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
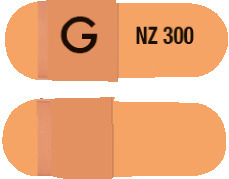
TACIDINE capsules are available in 2 strengths:
- TACIDINE 150 mg strength - hard gelatin capsule where one half of the capsule is pale yellow and has "NZ 150" printed in black. The other half of the capsule is dark yellow and has "G" printed in black
- TACIDINE 300 mg strength - hard, light brown, gelatin capsule with "NZ 300" printed in black on one half of the capsule and "G" printed in black on the other half
Ingredients
TACIDINE contains either 150 mg or 300 mg of nizatidine as the active ingredient.
The capsule also contains:
- colloidal anhydrous silica
- croscarmellose sodium
- pregelatinised maize starch
- purified talc
- sodium lauryl sufate
- magnesium stearate
- quinoline yellow (150 mg only)
- allura red AC (150 mg only)
- iron oxide red (300 mg only)
- iron oxide yellow
- titanium dioxide
- gelatin
- TekPrint SW-9008 Black Ink (ARTG PI No: 2328)
- TekPrint SW-9009 Black Ink (ARTG PI No: 2343).
TACIDINE capsules contain phenylalanine.
Sponsor
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in January 2024.
Australian registration numbers:
TACIDINE 150mg - AUST R 94204
TACIDINE 300mg - AUST R 94205
TACIDINE® is a Viatris company trade mark
Tacidine_cmi\Jan24/00
Published by MIMS March 2024


 Some elderly patients may have creatinine clearances of less than 50 mL/min and, based on pharmacokinetic data in patients with renal impairment, the dose for such patients should be reduced accordingly. The clinical effects of this dosage reduction in patients with renal failure have not been evaluated.
Some elderly patients may have creatinine clearances of less than 50 mL/min and, based on pharmacokinetic data in patients with renal impairment, the dose for such patients should be reduced accordingly. The clinical effects of this dosage reduction in patients with renal failure have not been evaluated. Chemical name: N-[2-[[[2-(dimethylamino) methyl]-4-thiazolyl]- methyl]thio]- ethyl]-N'-methyl-2-nitro-1, 1-ethenediamine.
Chemical name: N-[2-[[[2-(dimethylamino) methyl]-4-thiazolyl]- methyl]thio]- ethyl]-N'-methyl-2-nitro-1, 1-ethenediamine.