What is in this leaflet
This leaflet answers some common questions about Temolide. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Temolide against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet.
You may need to read it again.
What Temolide is used for
Temolide is used to treat patients with brain tumours. Temolide is also used to treat adult patients with advanced metastatic malignant melanoma.
Your doctor, however, may prescribe Temolide for another purpose.
Ask your doctor if you have any questions about why Temolide has been prescribed for you.
Temolide belongs to a group of medicines called cytotoxic or chemotherapy medicines.
Temolide works by killing cancer cells and stopping cancer cells from growing and multiplying.
This medicine is only available with a doctor's prescription.
Use in children
Temolide capsules are used to treat children 3 years and older, with specific forms of brain tumour (glioblastoma multiforme or anaplastic astrocytoma, showing recurrence or progression after standard therapy).
Before you take it
When you must not take it
Do not take Temolide if:
- you are allergic to Temolide (temozolomide), dacarbazine (DTIC) or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include:
- hives, itching or skin rash
- swelling of the face, lips or tongue. This may lead to difficulty swallowing.
- shortness of breath, wheezing, difficulty breathing or a tight feeling in your chest.
- you or your partner are pregnant or intend to become pregnant.
Temolide may cause birth defects if either the male or female is using Temolide at the time of conception or during pregnancy. Therefore, female patients must have a negative pregnancy test before starting Temolide. Both male and female patients and their partners should each use some kind of birth control while taking Temolide. Male patients whose partners are already pregnant should use a condom to minimise exposure of the unborn baby to Temolide in the sperm.
- you are breastfeeding.
- you have a very low level of white blood cells, red blood cells or platelets.
Do not use Temolide after the expiry date printed on the bottle.
Do not use Temolide if the packaging shows signs of tampering.
Before you start to take it
You must tell your doctor if:
- you vomit frequently.
Your doctor may give you medicine to control the vomiting
- you are anaemic or have blood clotting problems.
- you intend to have children.
Temolide may cause infertility in men.
- you have liver or kidney problems.
- you have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes
Taking other medicines
Tell your doctor if you are taking any other medicines, including medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by Temolide or may affect how well Temolide works. These include other medicines used to treat cancer or any other treatment that may lower your immune system. You may need different amounts of your medicine or you may need to use different medicines. Your doctor will advise you.
How to take it
Follow all directions given to you by your doctor carefully.
They may differ from the information contained in this leaflet.
How much to take
Your doctor has worked out the exact dose of Temolide for you according to your individual needs.
You may be given other medication to take before or after Temolide to help stop nausea.
If you are taking Temolide in combination treatment with radiation (newly diagnosed patients):
If you are a patient with a newly diagnosed brain tumour, your doctor will start you on a dose of Temolide every day for 42 days (up to 49 days) in combination with radiation therapy. This is the first part of the treatment ("concomitant phase") in which you complete the radiation therapy. Your treatment will be interrupted for 4 weeks to give your body a chance to recover.
Then, you will start the next phase of treatment ("adjuvant phase") and your Temolide dose will change. In this phase, there are up to 6 treatment cycles. Each treatment cycle lasts 28 days. You will take your new dose of Temolide capsules once daily for the first five days ("dosing days") of each cycle, followed by 23 days without Temolide; this adds up to a 28 day treatment cycle. After day 28, the next cycle will begin, in which you will again take this medicine once daily for five days followed by 23 days without Temolide. Before each new treatment cycle begins, your blood will be tested to determine if the Temolide dose needs to be adjusted.
If you are taking only Temolide (patients treated for recurrent brain tumour):
Take the dose the doctor has prescribed once a day for five days.
Depending on your response to Temolide, a new treatment cycle will begin each 28 days. You will then take this medicine again once daily for five days.
Before each new treatment cycle, your blood will be tested to see if the dose needs to be changed.
How to take it
Each time you start a new treatment cycle, be sure you understand exactly how many capsules of each strength you need to take on each day of dosing.
All patients
Temolide comes in different strength capsules (shown on the outer label in mg). Each strength is a different colour. Depending on the dose of Temolide that your doctor prescribes, you may have to take several capsules on each dosing day of the treatment cycle
Be sure you understand exactly how many capsules you need to take of each strength. Ask your doctor or pharmacist to write down the number of each strength (include colour) that you need to take on each dosing day.
- Be sure you know exactly which days are your dosing days.
- Be sure you review the dose with your health care provider each time you start a new cycle. Sometimes the dose or the mix of capsules you need to take will be different from the last cycle.
Once you take the medicine home, if you are confused or unsure about how to take your dose, call for re-instruction before beginning the treatment cycle. Errors in how you take this medicine may have serious health consequences
Swallow the capsules whole with a glass of water. Do not open or chew the capsules.
When to take it
Take Temolide without food at least one hour before a meal.
It is good practice to take Temolide at about the same time each day.
If vomiting occurs after you take your capsules, do not take another dose that day.
How long to take it
Your doctor will tell you when your treatment should be stopped.
If you forget to take it
If you miss a dose, take the missed dose as soon as possible during the same day. If a full day has gone by, check with your doctor.
Do not double the next dose unless your doctor tells you to do so.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (Phone 13 11 26 - Australia or 0800 764 766 - New Zealand) for advice, if you think you or anyone else may have taken too much Temolide. Do this even if there are no signs of discomfort or poisoning.
While you are taking Temolide
Things you must do
Tell all doctors, dentists and pharmacists who are treating you that you are being treated with Temolide.
Tell your doctor if you feel sick or vomit while being treated with Temolide.
Your doctor may give you another medicine to help stop this.
Tell your doctor if you become unusually pale or tired, get blood clotting problems or frequent infections while being treated with Temolide.
These could be caused by a low level of red blood cells, platelets or white blood cells in the blood. This is more common in patients over 70 years of age. Your doctor may need to change your dose of Temolide.
If you or your partner becomes pregnant while you are being treated with Temolide, tell your doctor.
Be sure to keep all your doctor's appointments so your progress can be checked.
Your doctor may need to do some blood and other tests from time to time to check on your progress and detect any unwanted side effects.
Keep follow up appointments with your doctor.
It is important to have your follow-up doses of Temolide at the appropriate times to get the best effects from your treatment.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are being treated with Temolide.
Store Temolide out of the reach of children.
Things you must not do
Do not open the capsules. If a capsule is damaged, avoid contact with your skin, eyes and nose. Avoid inhaling the powder. If you touch the powder or get some in your eyes or nose, wash the area with water.
Do not give Temolide to anyone else, even if they have the same condition as you.
Do not use Temolide to treat any other complaints unless your doctor tells you to.
Things to be careful of
Be careful driving or operating machinery, until you know how Temolide affects you.
As with other medicines, Temolide may make some people feel tired.
If this occurs do not drive.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Temolide.
Like other medicines that treat cancer, Temolide may have unwanted side effects. Sometimes they may be serious, most of the time they are not. You may need medical attention if you get some of these side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- nausea, vomiting, feeling unwell
- tiredness, sleepiness
- constipation
- headache
- loss of appetite or weight
- diarrhoea
- fever or high temperature
- rash, hair loss, itching
- dizziness, weakness
- general body pain
- stomach pain, indigestion
- different taste sensation
- mouth ulcers
- coughing
- sleeplessness
These are the more common side effects of Temolide.
Tell your doctor as soon as possible if you notice any of the following:
- shortness of breath
- tingling or numbness in hands or feet
- bruising, bleeding or being unusually pale or tired
This could be caused by a low level of platelets or red blood cells in the blood. - shivering that is associated with chills and fever
This could be sign of an infection caused by a low level of white blood cells in the blood. - development of red or purple spots under the skin
These may be serious side effects. You may need medical attention.
These last two side effects of Temolide may take some time to occur. Therefore, even after you have finished your treatment with Temolide, you should tell your doctor immediately if you notice these side effects.
Other side effects not listed above may also occur in some patients.
Tell your doctor if you notice anything else that is making you feel unwell.
Do not be alarmed by this list of possible side effects.
You may not experience any of them.
After using it
Storage
Keep your Temolide capsules in the bottle until it is time to use them.
Keep Temolide in a cool dry place where the temperature stays below 25 °C.
Do not leave it in the car or on window sills.
Keep it where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
Return any unused medicine to your pharmacist.
Product description
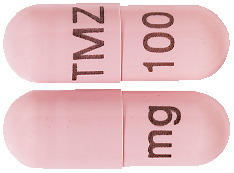
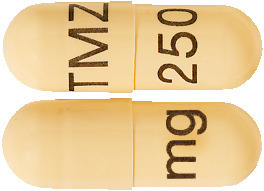
What it looks like
The 5 mg capsules are light green opaque, marked with black imprint “TMZ 5 mg”
The 20 mg capsules are rich yellow marked with black imprint “TMZ 20 mg”
The 100 mg capsules are flesh coloured, marked with black imprint “TMZ 100 mg”
The 140 mg capsules are powder blue marked with black imprint “TMZ 140 mg”
The 180*mg capsules are orange marked with black imprint “TMZ 180 mg”
The 250 mg capsules are buff coloured marked with black imprint “TMZ 250 mg”
Tell your pharmacist if you notice any change in the appearance of the capsule.
Ingredients
Active ingredient:
Temozolomide
Inactive ingredients:
- Anhydrous lactose (in the 5mg and 20mg capsules only),
- sodium starch glycollate
- stearic acid
- tartaric acid
- cellulose microcrystalline
- anhydrous colloidal silica.
The capsule shells also contain the following ingredients:
- gelatin
- titanium dioxide
- water
- Opacode Monogramming Ink S-1-277002
- Indigo Carmine CI73015 (Temolide 5 mg and 140 mg)
- Iron Oxide Yellow CI77492 (Temolide 5 mg, 20 mg and 250 mg)
- Iron Oxide Red CI77491 (Temolide 100 mg and 250 mg)
- Iron oxide black CI77499 (Temolide 100mg and 250mg)
- Sunset Yellow FCF CI5985 (Temolide 250 mg)
- Allura Red AC CI16035(Temolide 180 mg)
Temolide does not contain sucrose, gluten, tartrazine or other azo dyes.
Sponsor
Southern Cross Pharma Pty Ltd
56 Illabunda Drive
Malua Bay NSW 2536
ABN 47 094 447 677
Date of Information:
4 August 2016
Australian Registration Number:
5 mg capsule AUST R 192690
20 mg capsule AUST R 192679
100 mg capsule AUST R 192688
140 mg capsule AUST R 192695
180 mg capsule AUST R 192682
250 mg capsule AUST R 192686
*The 180mg capsules are not marketed.