What is in this leaflet
This leaflet answers some common questions about TENORMIN. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking TENORMIN against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What TENORMIN is used for
TENORMIN belongs to a group of medicines called beta-blockers.
It works by affecting the body's response to certain nerve impulses, especially in the heart. As a result, it decreases the heart's need for blood and oxygen and therefore reduces the amount of work the heart has to do. It widens the blood vessels in the body, causing blood pressure to fall. It also helps the heart to beat more regularly.
TENORMIN is used to:
- lower high blood pressure, which is called hypertension
- prevent angina
- treat irregular heart rhythm or beat called arrhythmias
- treat heart attacks, or reduce your risk of heart complications following a heart attack
TENORMIN may be either used alone or in combination with other medicines to treat your condition.
Hypertension:
All people have blood pressure. This pressure helps to push blood all around your body. Your blood pressure changes during the day, depending on how busy you are or how you are feeling.
You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
Regular blood pressure checks are the only way of knowing that you have hypertension. There are usually no symptoms of hypertension and you may feel fine. If hypertension is not treated, serious health problems such as stroke, heart disease and kidney failure may occur.
TENORMIN helps to lower your blood pressure.
Angina:
Angina is a discomfort or pain felt in your chest. The pain may also be felt down your arms or neck and sometimes your shoulders and back. This may be caused by not enough oxygen or blood reaching areas of your heart. Angina pain is often brought on by exercise or stress.
TENORMIN is used to prevent angina. It is not used to relieve a sudden attack of angina.
Irregular heart beat (arrhythmia):
A number of factors such as some heart diseases, an over active thyroid gland or chemical imbalances may cause your heart to have an irregular heart beat or rhythm.
TENORMIN helps restore your heart's normal rhythm.
Reducing heart complications after heart attack:
After a heart attack, you may have complications such as an irregular heart beat or an increased chance of having another heart attack.
TENORMIN helps to prevent these complications from occurring.
Ask your doctor if you have any questions about why TENORMIN has been prescribed for you. Your doctor may have prescribed TENORMIN for another reason.
TENORMIN is not recommended for use in children, as there have been no studies of its effects in children.
There is no evidence that TENORMIN is addictive.
This medicine is only available with a doctor's prescription.
Before you take TENORMIN
When you must not take it
Do not take TENORMIN if:
- you have or have had asthma (difficulty in breathing, wheezing and coughing), bronchitis or other lung problems in the past.
- you have the following conditions:
- a history of allergic problems, including hayfever. Symptoms of an allergy may include: rash, itching, watery eyes or sneezing.
- a very slow heart beat (less than 45-50 beats/minute)
- a severe blood vessel disorder causing poor circulation in the arms and legs
- certain other heart conditions
- phaeochromocytoma (a rare tumour of the adrenal gland) which is not being treated with other medicines
- low blood pressure (hypotension)
- too much acid in your blood (metabolic acidosis)
- you are receiving:
- certain anaesthetics for medical dental procedures
- emergency treatment for shock or severely low blood pressure
- you have an allergy to atenolol, the active ingredient in TENORMIN or any of the ingredients listed at the end of this leaflet, or to any other beta-blocker medicine.
Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; rash, itching or hives on the skin or you may feel faint.
- you are pregnant, intend to become pregnant, are breast feeding or intend to breast feed.
Your doctor will discuss the possible risks and benefits of using TENORMIN during pregnancy and breast feeding. TENORMIN passes into breast milk and may therefore affect the breast-fed baby.
If you are not sure whether any of these apply to you, check with your doctor.
Do not use TENORMIN if the expiry date (EXP) printed on the pack has passed.
Do not use TENORMIN if the package is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking TENORMIN, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor if:
- you have any allergies to:
- any other medicine, including eye drops, or other beta-blocker medicines
- any other substances, such as foods, preservatives or dyes
- insect stings
TENORMIN may make allergies worse or make them harder to treat.
- you have or have had a history of any of the following conditions:
- heart problems
- diabetes
- an over active thyroid gland called hyperthyroidism.
- kidney problems
- circulation problems
If you have not told your doctor about any of the above, tell them before you take TENORMIN.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and TENORMIN may interfere with each other. These include:
- other beta-blocker medicines
- medicines used to treat high blood pressure or angina
- medicine used to treat heart problems
- insulin and tablets used to treat diabetes
- medicines used to treat arthritis, pain, or inflammation
If any of these medicines and TENORMIN are taken together, it may affect how each of them work. You may need to take different amounts of your medicine, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or to avoid while taking TENORMIN.
If you have not told your doctor about any of these things, tell them before you take any TENORMIN.
How to take TENORMIN
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
How much to take
Hypertension:
The usual dose is from 50mg (1 tablet) up to 200mg (4 tablets) of TENORMIN daily.
If your dose is 100mg or less, take it once a day. If you need to take more than 100mg (2 tablets), take half of your TENORMIN in the morning and the other half in the evening.
Angina or Irregular Heart Beat:
The usual dose is from 50mg (1 tablet) up to 100mg (2 tablets) taken as a single dose or half the dose in the morning and half at night.
Heart attack:
The usual dose is 50mg (1 tablet) of TENORMIN daily.
Certain people such as the elderly or those with kidney problems, may require a lower dose.
When to take it
It does not matter if you take your TENORMIN before or after food.
Swallow TENORMIN with a glass of water, during or immediately after a meal.
Take your tablet at the same time everyday. Taking your tablets at the same time each day will have the best effect. It will also help you remember when to take the tablets.
How long to take it
Take TENORMIN everyday. Continue taking TENORMIN until your doctor advises you to stop.
TENORMIN helps treat your condition, but does not cure it.
Do not stop taking TENORMIN without checking with your doctor. Your doctor may want you to gradually reduce the amount of TENORMIN you are taking. This should take place over a period of about 2 weeks before stopping completely. Do not stop suddenly as this may worsen your condition.
Make sure you keep enough TENORMIN to last over weekends and holidays.
If you forget to take it
If it is less than six hours from when you missed your dose, take it as soon as you remember, and then go back to taking your tablets at the same time you would normally.
If it is more than six hours since your last dose, skip the dose you missed and take your next dose when you would normally.
Do not take a double dose of TENORMIN to make up for the dose that you missed.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much TENORMIN. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much TENORMIN, you may feel faint or dizzy or you may find it difficult to breathe.
While you are taking TENORMIN
Things you must do
Attend all of your doctor's appointments so that your progress can be checked.
Tell any doctors, dentists and pharmacists who are treating you that you are taking TENORMIN.
If you are about to be started on any new medicines, tell your doctor, dentist or pharmacist that you are taking TENORMIN.
Tell your doctor immediately if you become pregnant while taking TENORMIN.
Tell your doctor immediately if you have an allergic reaction to any foods, medicines or insect stings. TENORMIN can cause allergic reactions to be worse and harder to treat.
If you have diabetes, check your blood sugar level regularly and report any changes to your doctor. TENORMIN may affect your diabetes. It may hide the symptoms of low blood sugar levels, such as a fast heart beat. It may also take longer for your blood sugar level to get back to normal even if you follow the usual treatment for diabetes. Your diabetic medicines may have to be changed or the doses adjusted.
If you continue to have angina attacks, or have more of them whilst taking TENORMIN, tell your doctor. TENORMIN is used to help prevent angina, so your angina attacks should become less severe and occur less often.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly. You may feel light-headed or dizzy after taking TENORMIN. This is because your blood pressure is falling suddenly.
If this problem gets worse or continues, talk to your doctor.
To help your body get used to the change in blood pressure, you may find the following hints useful:
- Stand up slowly when getting up from a chair or bed. This will allow your body get used to the change in position and blood pressure.
- If you feel dizzy, sit or lie down until you feel better.
- If you feel faint, sit down and put your head between your knees.
Drink lots of water when exercising and during hot weather when taking TENORMIN, especially if you sweat a lot. If you do not drink enough water while taking TENORMIN, you may feel faint, light-headed or sick. The recommended healthy minimum water intake is 6-8 glasses a day.
If you are having surgery (even at the dentist), tell your doctor or dentist that you are taking TENORMIN. TENORMIN may affect some of the medicines used during surgery.
If you have to have any medical tests while you are taking TENORMIN, tell your doctor. TENORMIN may affect the results of some tests.
Things you must not do
Do not stop taking TENORMIN or change the dose without checking with your doctor.
Do not take any new medicines with TENORMIN, unless your doctor has told you to.
Do not use TENORMIN to treat any other complaint unless your doctor tells you to.
Do not give TENORMIN to anyone else, even if their symptoms seem similar or they have the same condition as you.
Things to be careful of
Take care driving or operating machinery until you know how TENORMIN affects you. TENORMIN may cause dizziness, fatigue, light-headedness or faintness in some people.
Make sure you know how you react to TENORMIN before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or lightheaded.
Be careful not to over exercise when you first start taking TENORMIN. It helps prevent angina resulting from physical activity and exercise. You may be tempted to exercise too much. Talk to your doctor about how much exercise you can do.
Dress warmly during cold weather, especially if you will be outside for a long time (for example, when playing or watching sport in winter). TENORMIN, like other beta-blocker medicines, may make you more sensitive to cold temperatures, especially if you have circulation problems. Beta-blockers tend to decrease blood circulation in the skin, fingers and toes.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking TENORMIN.
If you get any side effects, do not stop taking TENORMIN without first talking to your doctor. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- stomach upsets such as diarrhoea, constipation, abdominal pain or heartburn (indigestion)
- dry mouth, change in taste sensation
- dizziness, headache or buzzing or ringing in the ears
- slow or irregular heart beat
- dry eyes, problems with vision
- runny or blocked nose
- difficulty sleeping, nightmares
- skin reactions (e.g. rash, itching, worsening of psoriasis)
- cold fingers and toes
- increased hair loss
- tingling, 'pins and needles' or walking unsteadily
- sexual problems
These side effects are usually mild.
Tell your doctor immediately if you notice any of the following:
- confusion or disorientation
- depression or mood changes or a worsening of these
- unusual thoughts, hallucinations (seeing, feeling or hearing things that are not there)
- light-headedness or fainting which may be due to low blood pressure
- yellowing of the skin and/or eyes (jaundice)
These are serious side effects. You may need urgent medical attention. Serious side effects are rare.
If any of the following happen, tell your doctor immediately, or go to Accident and Emergency at your nearest hospital:
- wheezing, chest tightness or difficulty breathing
- unexplained bruising
- swelling of the face, lips or throat
These are very serious side effects and you may need urgent medical attention or hospitalisation. These side effects are rare.
Other side effects not listed here may occur in some patients. Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking TENORMIN
Storage
Keep your tablets in a cool, dry place where the temperature stays below 25°C. Protect from light.
Keep your tablets in the pack until it is time to take them. If you take TENORMIN out of the pack it will not keep well.
Do not store it or any other medicine in the bathroom or near a sink. Do not leave it in the car or on a window sill. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking TENORMIN, or the tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What TENORMIN looks like
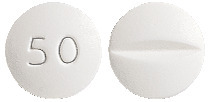
TENORMIN 50 mg tablets are white, round, biconvex, film coated, tablets marked with 50 on one side and bisected on the other.
TENORMIN tablets come in calendar packs containing 30 tablets.
Tablet Ingredients
Each TENORMIN tablet contains atenolol 50 mg as the active ingredient.
Plus the following inactive ingredients:
- magnesium stearate
- magnesium carbonate hydrate
- maize starch
- sodium lauryl sulfate
- gelatin
- hypromellose
- glycerol
- titanium dioxide
TENORMIN does not contain lactose, sucrose, gluten, tartrazine or any other azo dyes.
Sponsor
AstraZeneca Pty Ltd
ABN 54 009 682 311
66 Talavera Road
MACQUARIE PARK NSW 2113
Telephone: 1800 805 342
Australian Registration Number:
TENORMIN 50 mg tablets - AUST R 287200
This leaflet was prepared in October 2017.
TENORMIN is a trade mark of the AstraZeneca group of companies.
Doc ID-001066877 v3.0
Published by MIMS May 2018


 Molecular formula: C14H22N2O3.
Molecular formula: C14H22N2O3.