1. Why am I using Trientine Waymade?
Trientine Waymade contains the active ingredient trientine dihydrochloride. Trientine Waymade binds to copper and is known as a chelating agent.
Trientine Waymade is used to treat Wilson’s disease in people who can not take another medicine called penicillamine because of side effects.
Wilson’s Disease is a condition which results in too much copper in the body. This medicine binds to copper and allows it to pass out of the body.
2. What should I know before I use Trientine Waymade?
Warnings
Do not use Trientine Waymade if:
- you are allergic to trientine dihydrochloride, or any of the ingredients listed at the end of this leaflet. Always check the ingredients to make sure you can use this medicine.
Check with your doctor if you:
- have any other medical conditions
- take any medicines for any other condition.
If you were already taking another trientine medicine, your doctor may change your daily dose when switching to Trientine Waymade treatment.
Your doctor will need to regularly check for symptoms of your disease and copper levels in your blood and urine. Regular monitoring is especially important at the start of your treatment or when your dose is changed, in growing children and pregnant women to ensure that copper levels are maintained at a suitable level. The doctor may need to increase or decrease your dose of Trientine Waymade.
Regular monitoring is also important if you have liver or kidney problems.
This medicine may reduce the level of iron in your blood and your doctor may prescribe you iron supplementation (see additional information under 3. What if I am taking other medicines?).
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant. Trientine Waymade can be harmful to the unborn baby when taken by a woman during pregnancy so your doctor will discuss with you the benefits and risks of using it. If you are pregnant and taking Trientine Waymade you will be monitored throughout your pregnancy for any effect on the baby or changes in your copper levels.
Talk to your doctor if you are breastfeeding or intend to breastfeed. It is not known if Trientine Waymade passes into your breast milk.
Children
Do not give this medicine to a child under the age of 6 years. Safety and effectiveness in children younger than 6 years have not been established.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with Trientine Waymade and affect how it works.
Some medicines should not be given at the same time as they may stop Trientine Waymade from being absorbed into the body.
If you take other medicines, including non-prescription medicines, vitamins or supplements, they should be taken at least one hour before or after your dose of Trientine Waymade.
Medicines that may reduce the effect of Trientine Waymade include:
- Mineral supplements containing iron or zinc
If your doctor advises you to take an iron supplement or an antacid, separate the dose by at least 1 hour before or after your Trientine Waymade dose.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Trientine Waymade.
4. How do I use Trientine Waymade?
How much to take
- Your doctor will decide the correct dose for you.
- Adults: the usual dose is 3 to 5 capsules a day. The total daily dose should be divided into 2 to 4 smaller doses as directed by your doctor.
- Children: the dose will depend on age and body weight. The total daily dose should be divided into 2 or 3 smaller doses as directed by your doctor.
- Follow the instructions provided and use Trientine Waymade until your doctor tells you to stop. This medicine is for long-term use because Wilson’s disease is a life-long condition.
When to take Trientine Waymade
- Trientine Waymade should be taken on an empty stomach, at least 1 hour before or 2 hours after food.
- The capsules should be swallowed whole with water and should not be opened or chewed. Tell your doctor if you have difficulties swallowing this medicine.
If you forget to take Trientine Waymade
Discuss with your Doctor or Pharmacist about what to do if you miss your dose. Trientine Waymade should be taken regularly at the same time each day. If you miss your dose at the usual time, take your next dose at scheduled time.
Do not take a double dose to make up for the dose you missed.
Do not exceed the daily dose prescribed by your Doctor.
If you use too much Trientine Waymade
If you think that you have used too much Trientine Waymade, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using Trientine Waymade?
Things you should do
Keep all of your doctor’s appointments so that your progress can be checked.
- Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Call your doctor straight away if you:
- notice your symptoms get worse during treatment with Trientine Waymade, especially when first starting treatment.
Remind any doctor, dentist or pharmacist you visit that you are using Trientine Waymade.
Things you should not do
- Do not stop using this medicine suddenly.
- Do not change your treatment without speaking with your doctor.
- Do not open or break the capsules. If the capsule contents comes into contact with your body, wash the area immediately with water.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Trientine Waymade affects you.
Looking after your medicine
- Keep container tightly closed.
- Store at 2° to 8°C (Refrigerate. Do not freeze).
- Store in the original container and retain the silica gel sachet in the bottle in order to protect from moisture.
Follow the instructions in the carton on how to take care of your medicine properly.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.

Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell. Other side effects not listed here may occur in some people.
Some of these side effects (for example, changes in liver function, changes in blood tests) can only be found when your doctor does tests from time to time to check your progress.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Trientine Waymade contains

Do not take this medicine if you are allergic to any of these ingredients.
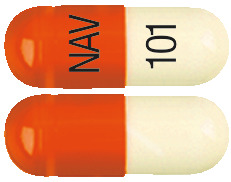
What Trientine Waymade looks like
Trientine Waymade are cylindrical hard gelatin capsules filled with a white to off white color powder. The capsule has an opaque orange colour cap printed with ‘NAV’ in black ink and an opaque white coloured body printed with “101” in black ink.
Trientine Waymade is supplied in a white bottle with a screw cap, containing 100 capsules and a sachet of dried silica gel as desiccant.
Do not eat the desiccant.
(Aust R 327984).
Who distributes Trientine Waymade
Clinect Pty Ltd
120-134 Atlantic Drive, Keysborough
VIC 3173, Australia
Free Call Australia: 1800 899 005
This leaflet was prepared in January 2021
Published by MIMS March 2021

 There have been reports of neurological deterioration at the start of treatment in Wilson's disease patients treated with copper chelators including trientine, with symptoms of, for example, dystonia, rigidity, tremor and dysarthria (see Section 4.2 Dose and Method of Administration).
There have been reports of neurological deterioration at the start of treatment in Wilson's disease patients treated with copper chelators including trientine, with symptoms of, for example, dystonia, rigidity, tremor and dysarthria (see Section 4.2 Dose and Method of Administration).
