What is in this leaflet
This leaflet answers some common questions about Ultibro Breezhaler 110/50.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available.
You should ensure that you speak to your pharmacist or doctor to obtain the most up-to-date information on the medicine. You can also download the most up-to-date leaflet from www.novartis.com.au. Those updates may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your doctor has weighed the risks of you having Ultibro Breezhaler 110/50 against the benefits they expect it will have for you.
If you have any concerns about having this medicine, ask your doctor or pharmacist.
Keep this leaflet. You may need to read it again.
What Ultibro Breezhaler 110/50 is used for
Ultibro capsules are for the treatment of chronic obstructive pulmonary disease, also called COPD. COPD is a serious lung condition that can cause difficulty in breathing, and constant coughing. Symptoms of COPD include shortness of breath, cough, chest discomfort and coughing up phlegm. Ultibro Breezhaler 110/50 helps to improve your condition and reduce exacerbations (periodic worsening of symptoms) from occurring.
Ultibro capsules for inhalation belong to a group of medicines called bronchodilators. These medicines are used to keep the air passages in the lungs open and make breathing easier.
Ultibro Breezhaler 110/50 blocks tightening of these muscles in the lungs and also relaxes the muscles in the walls of the small air passages in the lungs. This helps open up the airways, making it easier for air to get in and out of the lungs.
Ultibro capsules for inhalation contain the active ingredients, indacaterol maleate and glycopyrronium bromide (glycopyrrolate) in a capsule form.
The capsules are for oral inhalation only. The powder from the capsule is inhaled (breathed into the lungs), using the Breezhaler® inhalation device provided with the medicine.
Ask your doctor if you have any questions about why Ultibro Breezhaler 110/50 has been prescribed for you.
This medicine is only available with a doctor's prescription.
It is not addictive.
Before you use Ultibro Breezhaler 110/50
When you must not use it
Do not use Ultibro Breezhaler 110/50 if you have ever had an allergic reaction to indacaterol maleate or glycopyrronium bromide (the active ingredients) or to any of the other ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; rash, itching or hives on the skin.
Do not breast-feed while you are using this medicine. It is not known if the active ingredients pass into the breast milk and could affect your baby.
Do not use this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. In that case, return it to your pharmacist.
Before you start to use it
Tell your doctor if you have any of the following medical conditions:
- asthma (in this case you should not be treated with Ultibro)
- heart problems
- suffer from seizures or fits
- thyroid gland problems
- diabetes
- are taking similar medicines for your lung disease (see section "Taking other medicines")
- kidney problems
- severe liver problems
- eye problem called narrow-angle glaucoma
- difficulty passing urine
Your doctor may want to take special precautions if you have any of the above conditions.
Ultibro Breezhaler 110/50 is used as a maintenance treatment for your COPD. Do not use Ultibro Breezhaler to treat a sudden attack of breathlessness or wheezing.
Tell your doctor if you are pregnant or intend to become pregnant. Ultibro is not recommended for use during pregnancy. If it is necessary for you to use this medicine during pregnancy, your doctor will discuss with you the benefits and risks involved.
There are a number of other medicines that work in the same way as Ultibro and that are commonly prescribed. Some of these similar medicines that can be used to treat your lung disease include ipratropium, oxitropium, tiotropium (also called anticholinergics) and eformoterol or salmeterol (also called long-acting beta agonists). Please speak to your doctor or pharmacist if you still have any of these medicines because it may not be intended that you will use them while you are taking Ultibro.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines and Ultibro may interfere with each other. These include:
- medicines used in the treatment of depression (e.g. tricyclic antidepressants, monoamine oxidase inhibitors)
- medicines for your lung disease which contain active substances similar (same class) to those in Ultibro (e.g. ipratropium, oxitropium, tiotropium, eformoterol, salmeterol). Use of these may increase the risk of experiencing possible side effects.
- medicines that decrease the level of potassium in your blood. These include diuretics (also known as "water tablets" and used to treat hypertension, e.g. hydrochlorothiazide), other bronchodilators such as methylxanthines (e.g. theophylline) or steroids (e.g. prednisolone)
- beta-blockers used in the treatment of hypertension or other cardiac problems (e.g. propranolol) or in the treatment of glaucoma (e.g. timolol)
You may need to take different amounts of your medicines or you may need to take different medicines. Your doctor and pharmacist have more information.
If you have not told your doctor about any of these things, tell him/her before you start using Ultibro Breezhaler 110/50.
How to use Ultibro Breezhaler 110/50
You may have been given a treatment plan by your doctor to help you manage your COPD and to know what to do when it worsens. Make sure that you understand this plan by talking to your doctor and pharmacist about it. In particular, do not stop other medications that are used to treat COPD even if you feel well. Only stop other prescribed medications on medical advice.
Follow all directions given to you by your doctor and pharmacist carefully. These directions may differ from the information contained in this leaflet.
If you do not understand the instructions on the label or in the carton, ask your doctor or pharmacist for help.
How much to use
The dose for adults is the inhalation (puff) of the content of one capsule each day, every day. There is no gain to be had from exceeding this dose. Take your puff at the same time each day to help minimise your symptoms throughout the day and night. It will also help you remember to use your medicine.
If you do not feel an improvement after taking Ultibro, you should speak to your doctor.
How to use the Breezhaler
Carefully read the instructions and follow the diagrams inside the carton that show you how to use the Breezhaler properly.
Make sure you understand how to use the device properly. If you are not sure, ask your doctor or pharmacist for help.
Do not exceed the recommended dose prescribed by your doctor.
How long to use it
Continue to use this medicine for as long as your doctor tells you to.
If it helps your breathing problems, your doctor may want you to keep using it for a long time. This medicine helps to control your condition but it does not cure it. You will need to use other medications as well and this will be outlined in your COPD management plan.
If you still smoke, you should stop. If have not taken advice about an exercise program, consider asking for it.
If you forget to use it
If it is almost time for your next dose, skip the one you missed and use the next dose when you are meant to.
Otherwise, use it as soon as you remember, and then go back to using it as you would normally.
Do not use a double dose to make up for the one that you missed. This may increase the chance of you getting an unwanted side effect.
If you have trouble remembering when to use your medicine, ask your pharmacist for some hints.
If you use too much (Overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have used too much Ultibro. Do this even if there are no signs of discomfort or poisoning.
While you are using Ultibro Breezhaler 110/50
Things you must do
Only use the inhalation device contained in this pack.
Use this medicine exactly as your doctor has prescribed. Try not to miss any doses and use it even if you feel well. If you do not follow your doctor's instructions, you may not get relief from your breathing problems or you may have unwanted side effects.
If you find that the usual dose of Ultibro Breezhaler 110/50 is not giving as much relief as before, or does not last as long as usual, contact your doctor so that your condition can be checked. This is important to ensure your COPD is controlled properly.
If you become pregnant while using this medicine, tell your doctor. Your doctor can discuss with you the risks of using it while you are pregnant.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are using Ultibro Breezhaler 110/50.
Tell any other doctor, dentist or pharmacist who treats you that you are using this medicine.
Things you must not do
Do not exceed the recommended daily dose - it will not help you to do this. Instead, check your COPD management plan and seek medical attention. Do not swallow the capsules.
Do not take any other medicines for your breathing problems without checking with your doctor.
Do not give this medicine to anyone else, even if their condition seems similar to yours.
Do not use it to treat any other complaints unless your doctor tells you to.
Things to be careful of
Be careful driving, operating machinery or doing jobs that require you to be alert until you know how Ultibro affects you. This medicine may cause dizziness in some people. Make sure you know how you react before you drive a car, operate machinery, or do anything else that could be dangerous. If you are dizzy, do not drive.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are using Ultibro Breezhaler.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by these lists of possible side effects. You may not experience any of them. Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following side effects and they worry you:
- crushing chest pain (signs of insufficient blood and oxygen supply of the heart)
- excessive thirst, high urine output, increased appetite with weight loss, tiredness (high level of sugar in the blood)
- changes in vision, increased pressure in the eye
- blocked nose, sneezing, coughing, headache with or without fever (signs of upper respiratory tract infection)
- symptoms of a hypersensitivity reaction, such as difficulties in breathing or swallowing, swelling of tongue, lips and face, skin rash, itching, and hives
- irregular heartbeat
- symptoms of paradoxical bronchospasm, such as difficulty breathing with wheezing or coughing.
- swelling mainly of the tongue, lips, face and throat (possible signs of angioedema)
- urinary tract infection: painful and frequent urination (signs of cystitis)
- combination of sore throat, runny nose (signs of nasopharyngitis).
- feeling of pressure or pain in the cheeks and forehead (possible symptoms of sinus congestion)
- dizziness
- headache
- cough
- sore throat
- upset stomach, indigestion
- cavities
- fever
- chest pain
- difficulty and pain when passing urine (possible symptoms of bladder obstruction or urinary retention)
- pain in muscles, bones or joints
- fast heart beat or palpitations (signs of abnormal heart beat)
- nose bleeds
- muscle spasm
- itching/rash
- swollen hands, ankles and feet
- dry mouth
- nausea, vomiting, diarrhoea and abdominal pain (possible symptoms of gastroenteritis)
- problem falling asleep
- pain in extremities (e.g. arms or legs)
- tiredness
- tingling or numbness, decreased skin sensitivity
- voice alteration (hoarseness)
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if any of the following happen:
- COPD symptoms (breathlessness, wheezing, cough) do not improve or if they worsen during your treatment
Stop taking Ultibro and tell your doctor immediately or go to Accident and Emergency at your nearest hospital if any of the following happen:
- if you experience tightness of the chest, coughing, wheezing or breathlessness immediately after inhalation of Ultibro (signs of paradoxical bronchospasm)
- if you experience difficulties in breathing or swallowing, swelling of tongue, lips and face, skin rash, itching, and hives (signs of hypersensitivity reaction)
- if you experience eye pain or discomfort, temporary blurring of vision, visual halos or coloured images in association with red eyes; these may be signs of an acute attack of narrow-angle glaucoma.
Tell your doctor if you notice anything else that is making you feel unwell. Some people may have other side effects not yet known or mentioned in this leaflet. Some side effects may only be found when your doctor orders blood tests from time to time.
After using Ultibro Breezhaler 110/50
Cleaning and storage
- Follow the instructions in the carton on how to properly clean and take care of your Ultibro Breezhaler 110/50.
- Store it in a cool dry place away from moisture.
- Do not store the device or any other medicine in the bathroom or near a sink.
- Do not leave it in the car or on window sills.
Keep this medicine where children cannot see or reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop using this medicine or the expiry date has passed, ask your pharmacist how to dispose of it properly.
Product description
What it looks like
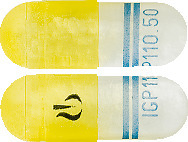
Indacaterol maleate/ glycopyrronium bromide (glycopyrrolate) 110/50 microgram capsules
Transparent yellow cap and natural transparent body capsules containing a white to practically white powder, with the product code "IGP110.50" printed in blue under two blue bars on body and the company logo printed in black on cap.
Breezhaler
A white plastic Breezhaler inhalation device is also supplied in the pack.
Ingredients
Active Ingredient
Each capsule contains 110 micrograms of indacaterol as indacaterol maleate and 50 micrograms of glycopyrronium as glycopyrronium bromide (glycopyrrolate).
Other ingredients
Ultibro capsules also contain lactose, tartrazine and magnesium stearate.
Sponsor
Ultibro Breezhaler 110/50 is supplied in Australia by:
Novartis Pharmaceuticals Australia Pty Limited
ABN 18 004 244 160
54 Waterloo Road
Macquarie Park NSW 2113
Telephone 1-800-671-203
Web site: www.novartis.com.au
® = Registered Trademark
This leaflet was prepared in August 2020.
Australian Registration Numbers.
Ultibro Breezhaler 110/50 microgram: AUST R 206449
(ulb081220c.doc) based on PI (ulb081220i.doc)
Published by MIMS February 2021



 The mean pre-dose FEV1 (average of the values taken at -45 and -15 min prior to the morning dose of study drug) was clinically meaningful and statistically significant in favor of Ultibro Breezhaler 110/50 at Week 26 compared to fluticasone/salmeterol (100 mL, p < 0.001) [ILLUMINATE], at Week 52 compared to placebo (189 mL, p < 0.001) [ENLIGHTEN] and at all visits up to Week 64 compared to glycopyrronium (70-80 mL, p-value < 0.001) and tiotropium (60-80 mL, p-value < 0.001) [SPARK]. In the [FLAME] study, the mean pre-dose FEV1 was a secondary efficacy endpoint which showed clinically meaningful and statistically significant result in favor of Ultibro Breezhaler 110/50 at all visits up to Week 52 compared to fluticasone/salmeterol (62-86 mL, p < 0.001).
The mean pre-dose FEV1 (average of the values taken at -45 and -15 min prior to the morning dose of study drug) was clinically meaningful and statistically significant in favor of Ultibro Breezhaler 110/50 at Week 26 compared to fluticasone/salmeterol (100 mL, p < 0.001) [ILLUMINATE], at Week 52 compared to placebo (189 mL, p < 0.001) [ENLIGHTEN] and at all visits up to Week 64 compared to glycopyrronium (70-80 mL, p-value < 0.001) and tiotropium (60-80 mL, p-value < 0.001) [SPARK]. In the [FLAME] study, the mean pre-dose FEV1 was a secondary efficacy endpoint which showed clinically meaningful and statistically significant result in favor of Ultibro Breezhaler 110/50 at all visits up to Week 52 compared to fluticasone/salmeterol (62-86 mL, p < 0.001).

 In the [SHINE] serial spirometry subset, Ultibro Breezhaler demonstrated a statistically significant improvement in FEV1 compared to placebo (400 mL, p < 0.001) and tiotropium (160 mL, p < 0.001) at 2 hours post-dose at Week 26.
In the [SHINE] serial spirometry subset, Ultibro Breezhaler demonstrated a statistically significant improvement in FEV1 compared to placebo (400 mL, p < 0.001) and tiotropium (160 mL, p < 0.001) at 2 hours post-dose at Week 26. In the [ILLUMINATE] study, Ultibro Breezhaler 110/50 demonstrated significant overall improvements in lung function compared with fluticasone/salmeterol, across all key subgroups, including age, gender, smoking history, disease severity, and reversibility.
In the [ILLUMINATE] study, Ultibro Breezhaler 110/50 demonstrated significant overall improvements in lung function compared with fluticasone/salmeterol, across all key subgroups, including age, gender, smoking history, disease severity, and reversibility.