What is in this leaflet
This leaflet answers some common questions about Vancocin capsules. It does not contain all the available information that is known about Vancocin capsules.
It does not take the place of talking to your doctor.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Vancocin capsules against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with this medicine. You may need to read it again.
What Vancocin capsules are used for
Vancocin capsules contains the active vancomycin (as vancomycin hydrochloride).
Vancocin capsules are an antibiotic used to treat serious infections involving the bowel. It works by killing or stopping the growth of the bacteria causing your infection.
Ask your doctor if you have any questions about why Vancocin capsules have been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor’s prescription.
There is no evidence that it is addictive.
Before you take it
When you must not take it
Do not take Vancocin capsules if you have ever had an allergic reaction to:
- any medicines containing vancomycin and similar antibiotics e.g. teicoplanin.
- any of the ingredients listed at the end of this leaflet.
Signs of an allergic reaction may include shortness of breath, wheezing or difficulty in breathing; swelling of the face, lips, tongue or any other parts of the body; rash, itching or hives on the skin.
Do not take Vancocin capsules if the expiry date on the pack has passed.
Do not take Vancocin capsules if the packaging is torn or shows signs of tampering.
Before you start to take it
Tell your doctor if you are allergic to any other medicines or any foods, dyes or preservatives.
Tell your doctor if you have or have had any of the following medical conditions:
- kidney or liver disease
- a special sensory impairment (e.g. blindness)
- pre-existing hearing loss
- inflammatory bowel disorders.
Do not take Vancocin capsules if you are pregnant or plan to become pregnant unless you and your doctor have discussed the benefits and risks involved.
Do not take Vancocin capsules if you are breast feeding or plan to breast feed. It is not recommended for use while breastfeeding as it is found in breast milk.
If you have not told your doctor about any of these things, tell them before you take Vancocin capsules.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with Vancocin capsules. These include:
- some other medicines used to treat infections, such as amikacin, amphotericin, colistin, gentamicin, neomycin, tobramycin and piperacillin/tazobactam.
- cisplatin, an anticancer medicine
- some fluid tablets (diuretics), such as etacrynic acid and furosemide (frusemide)
- anaesthetic agents
- cholestyramine, a powder taken to lower cholesterol levels
- suxamethonium or vecuronium, medicines used to relax muscles.
These medicines may be affected by Vancocin capsules or may affect how well it works. You may need different amounts of your medicines or may need to take different medicines. Your doctor or pharmacist has more information on medicines to be careful with or to avoid while taking Vancocin capsules.
Use in elderly or patients with pre-existing kidney disease
Elderly patients or those with a pre-existing kidney condition may be more sensitive to the effects or side effects of this medicine.
How to take it
How much to take
Your doctor will tell you how many Vancocin capsules you need to take each day. This will depend on the type of infection. The dose varies from patient to patient.
If you are elderly or have a pre-existing kidney condition, you may need to take fewer capsules.
The total dose for children should not exceed 2 grams per day.
How to take it
Swallow the capsules whole with a full glass of water.
When to take it
Vancocin capsules can be taken with or without food.
How long to take it
Continue taking Vancocin capsules for as long as your doctor tells you.
It is important to complete the full course prescribed by your doctor, even if you begin to feel better after a few days. If you do not, the bacteria causing your infection may not clear completely or your symptoms may return.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking your capsules as you would normally.
If you are not sure whether to skip the dose, talk to your doctor or pharmacist.
Do not take a double dose to make up for the dose that you missed.
If you have trouble remembering to take your tablets, ask your pharmacist for some hints.
If you take too much
Immediately telephone your doctor or Poisons Information Centre (13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much Vancocin capsules. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
Tell your doctor if the symptoms of your infection do not improve within a few days or if they become worse.
Tell any other doctors, dentists and pharmacists who are treating you that you are taking Vancocin capsules, especially if you are being started on any new medicines.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking Vancocin capsules. Vancocin capsules may affect other medicines used during surgery.
Tell your doctor if you become pregnant while taking Vancocin capsules.
Things you must not do
Do not take Vancocin capsules to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or change the dosage without first checking with your doctor. If you stop taking it, your condition may worsen.
Things to be careful of
As with any new medicine, you should take care when driving or operating machinery until you know how Vancocin capsules affects you.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Vancocin capsules.
This medicine helps most people with bacterial infections of the bowel, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Tell your doctor if you notice any of the following side effects and they worry you:
- indigestion
- stomach ache
- nausea
- chills
- diarrhoea
- vomiting.
Tell your doctor as soon as possible if you notice any of the following and they worry you:
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bleeding or bruising more easily than normal
- vertigo, dizziness or tinnitus (ringing in the ears)
- itchy rash
- loss of appetite
- fatigue.
Tell your doctor immediately or go to casualty at your nearest hospital if you notice any of the following:
- irregular or fast heartbeat
- chest tightness, wheezing, breathlessness
- redness of the upper body or pain and muscle spasm of the chest and back
- skin blister and bleeding in the lips, eyes, mouth, nose and genitals
- high fever and rash.
These are serious side effects of Vancocin capsules. You may need urgent medical attention. Serious side effects are rare.
Hearing loss has occurred in some patients taking Vancocin capsules. Most of these have occurred in patients who have pre-existing conditions such as kidney disease or partial hearing loss.
After finishing it
Tell your doctor immediately if you notice any of the following side effects, particularly if they occur several weeks after stopping treatment with Vancocin capsules:
- severe stomach cramps or pain
- severe, watery or bloody diarrhoea
- fever, in combination with one of the above.
These are rare but serious side effects. You may have a serious condition affecting your bowel and may need urgent medical attention.
Do not take any diarrhoea medicine without first checking with your doctor.
Tell your doctor if you notice anything else that is making you feel unwell. Some people may get other side effects while using Vancocin capsules.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking it
Storage
Keep your capsules in the blister pack until it is time to take them. If you take your capsules out of the blister pack they may not keep as well.
Keep your medicine in a cool, dry place where the temperature stays below 25°C. Protect from moisture.
Keep it where young children cannot reach it. A locked cupboard at least one-and-a-half metres above ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking Vancocin capsules or you find that the expiry date has passed, ask your pharmacist what to do with any capsules that are left over.
Product Description
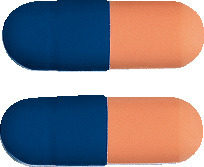
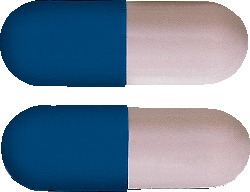
What it looks like
Vancocin 125 mg capsules are opaque peach and opaque blue. They are available in packs of 20.
Vancocin 250 mg capsules are opaque mushroom grey and opaque blue. They are available in packs of 20.
Ingredients
Active ingredient:
125 mg capsules
Each capsule contains vancomycin hydrochloride equivalent to 125 mg of vancomycin.
250 mg capsules
Each capsule contains vancomycin hydrochloride equivalent to 250 mg of vancomycin.
Inactive ingredients:
- macrogol 6000.
Capsule shell:
- gelatin
- indigo carmine
- iron oxide red
- titanium dioxide
- iron oxide yellow (125 mg only)
- iron oxide black (250 mg only).
Vancocin capsules do not contain lactose, sucrose, tartrazine or any other azo dyes.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos St
St Leonards NSW 2065
Australian Registration Numbers:
125 mg: AUST R 14674
250 mg: AUST R 14657
This leaflet was revised in June 2022.
Published by MIMS September 2022